Do You Believe In Magic? – by Dr. Paul Offit
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Here at 10almonds, we like to examine and present the science wherever it leads, so this book was an interesting read.
Dr. Offit, himself a much-decorated vaccine research scientist, and longtime enemy of the anti-vax crowd, takes aim at alternative therapies in general, looking at what does work (and how), and what doesn’t (and what harm it can cause).
The style of the book is largely polemic in tone, but there’s lots of well-qualified information and stats in here too. And certainly, if there are alternative therapies you’ve left unquestioned, this book will probably prompt questions, at the very least.
And science, of course, is about asking questions, and shouldn’t be afraid of such! Open-minded skepticism is a key starting point, while being unafraid to actually reach a conclusion of “this is probably [not] so”, when and if that’s where the evidence brings us. Then, question again when and if new evidence comes along.
To that end, Dr. Offit does an enthusiastic job of looking for answers, and presenting what he finds.
If the book has downsides, they are primarily twofold:
- He is a little quick to dismiss the benefits of a good healthy diet, supplemented or otherwise.
- His keenness here seems to step from a desire to ensure people don’t skip life-saving medical treatments in the hope that their diet will cure their cancer (or liver disease, or be it what it may), but in doing so, he throws out a lot of actually good science.
- He—strangely—lumps menopausal HRT in with alternative therapies, and does the exact same kind of anti-science scaremongering that he rails against in the rest of the book.
- In his defence, this book was published ten years ago, and he may have been influenced by a stack of headlines at the time, and a popular celebrity endorsement of HRT, which likely put him off it.
Bottom line: there’s something here to annoy everyone—which makes for stimulating reading.
Click here to check out Do You Believe In Magic, and expand your knowledge!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Sugar Alcohol That Reduces BMI!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Inositol Does-It-Ol’!
First things first, a quick clarification up-front:
Myo-inositol or D-chiro-inositol?
We’re going to be talking about inositol today, which comes in numerous forms, but most importantly:
- Myo-inositol (myo-Ins)
- D-chiro-inositol (D-chiro-Ins)
These are both inositol, (a sugar alcohol!) and for our purposes today, the most relevant form is myo-inositol.
The studies we’ll look at today are either:
- just about myo-inositol, or
- about myo-inositol in the presence of d-chiro-inositol at a 40:1 ratio.
You have both in your body naturally; wherever supplementation is mentioned, it means supplementing with either:
- extra myo-inositol (because that’s the one the body more often needs more of), or
- both, at the 40:1 ratio that we mentioned above (because that’s one way to help balance an imbalanced ratio)
With that in mind…
Inositol against diabetes?
Inositol is known to:
- decrease insulin resistance
- increase insulin sensitivity
- have an important role in cell signaling
- have an important role in metabolism
The first two things there both mean that inositol is good against diabetes. It’s not “take this and you’re cured”, but:
- if you’re pre-diabetic it may help you avoid type 2 diabetes
- if you are diabetic (either type) it can help in the management of your diabetes.
It does this by allowing your body to make better use of insulin (regardless of whether that insulin is from your pancreas or from the pharmacy).
How does it do that? Research is still underway and there’s a lot we don’t know yet, but here’s one way, for example:
❝Evidence showed that inositol phosphates might enhance the browning of white adipocytes and directly improve insulin sensitivity through adipocytes❞
Read: Role of Inositols and Inositol Phosphates in Energy Metabolism
We mentioned its role in metabolism in a bullet-point above, and we didn’t just mean insulin sensitivity! There’s also…
Inositol for thyroid function?
The thyroid is one of the largest endocrine glands in the body, and it controls how quickly the body burns energy, makes proteins, and how sensitive the body should be to other hormones. So, it working correctly or not can have a big impact on everything from your mood to your weight to your energy levels.
How does inositol affect thyroid function?
- Inositol has an important role in thyroid function and dealing with autoimmune diseases.
- Inositol is essential to produce H2O2 (yes, really) required for the synthesis of thyroid hormones.
- Depletion of inositol may lead to the development of some thyroid diseases, such as hypothyroidism.
- Inositol supplementation seems to help in the management of thyroid diseases.
Read: The Role of Inositol in Thyroid Physiology and in Subclinical Hypothyroidism Management
Inositol for PCOS?
A systematic review published in the Journal of Gynecological Endocrinology noted:
- Inositol can restore spontaneous ovarian activity (and consequently fertility) in most patients with PCOS.
- Myo-inositol is a safe and effective treatment to improve:
- ovarian function
- healthy metabolism
- healthy hormonal balance
While very comprehensive (which is why we included it here), that review’s a little old, so…
Check out this cutting edge (Jan 2023) study whose title says it all:
Inositol for fertility?
Just last year, Mendoza et al published that inositol supplementation, together with antioxidants, vitamins, and minerals, could be an optimal strategy to improve female fertility.
This built from Gambiole and Forte’s work, which laid out how inositol is a safe compound for many issues related to fertility and pregnancy. In particular, several clinical trials demonstrated that:
- inositol can have therapeutic effects in infertile women
- inositol can also be useful as a preventive treatment during pregnancy
- inositol could prevent the onset of neural tube defects
- inositol also reduces the occurrence of gestational diabetes
Due to the safety and efficiency of inositol, it can take the place of many drugs that are contraindicated in pregnancy. Basically: take this, and you’ll need fewer other drugs. Always a win!
Read: Myo-Inositol as a Key Supporter of Fertility and Physiological Gestation
Inositol For Weight Loss
We promised you “this alcohol sugar can reduce your BMI”, and we weren’t making it up!
Zarezadeh et al conducited a very extensive systematic review, and found:
- Oral inositol supplementation has positive effect on BMI reduction.
- Inositol in the form of myo-inositol had the strongest effect on BMI reduction.
- Participants with PCOS and/or who were overweight, experienced the most significant improvement of all.
Want some inositol?
As ever, we don’t sell it (or anything else), but for your convenience, here’s myo-inositol and d-chiro-inositol at a 40:1 ratio, available on Amazon!
Share This Post
-
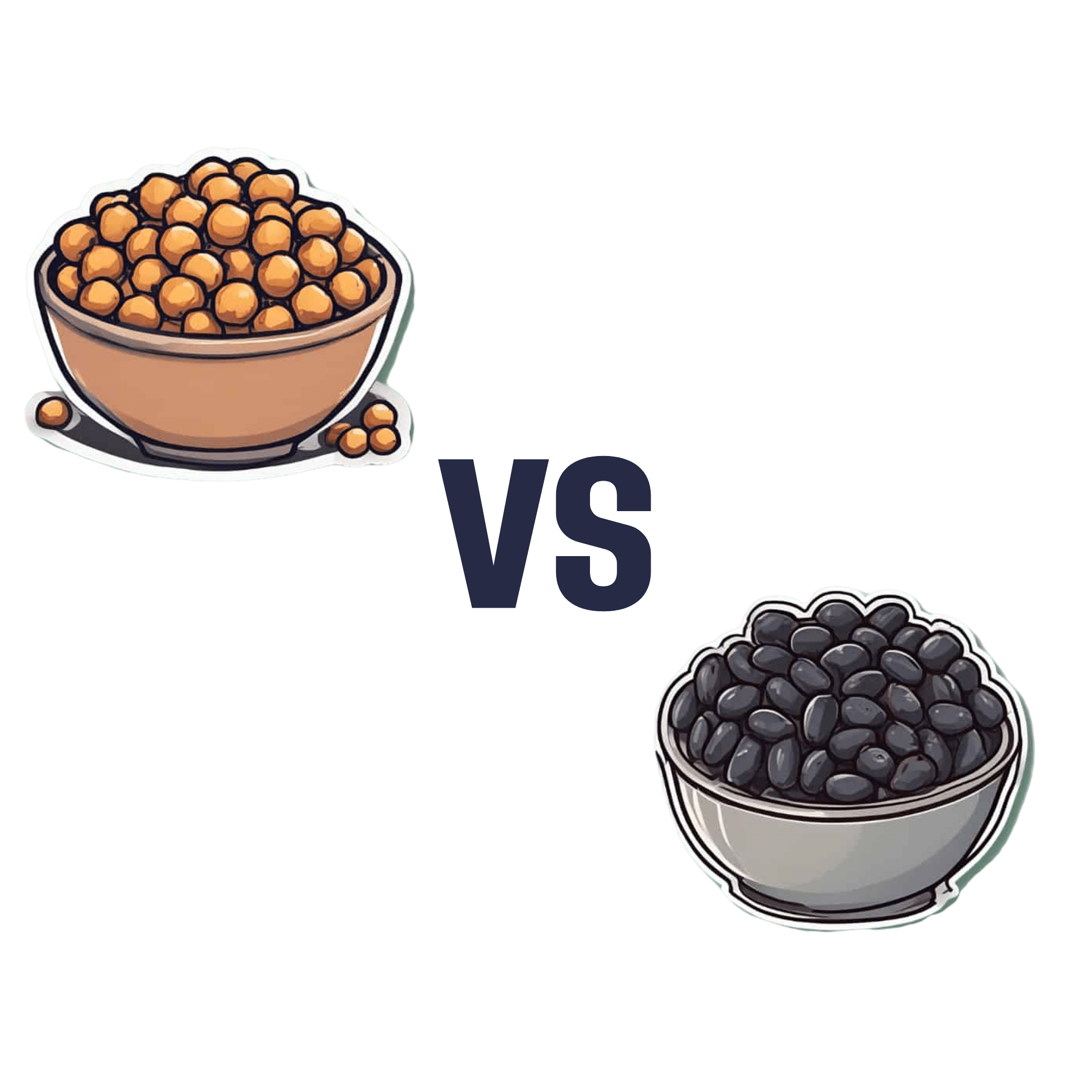
Chickpeas vs Black Beans – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing chickpeas to black beans, we picked the black beans.
Why?
They’re both great! But we consider the nutritional profile of black beans to be better:
In terms of macros, black beans have a little more protein, while chickpeas have more carbohydrates. Generally speaking, people are not usually short of carbs in their diet, so we’ll go with the one with more protein. Black beans also have more fiber, which is important for heart health and more.
In the category of micronutrients, black beans have twice as much potassium and twice as much calcium, as well as twice as much magnesium. Chickpeas, meanwhile are better for manganese and slightly higher in B vitamins, but B vitamins are everywhere (especially vitamin B5, pantothenic acid; that’s literally where its name comes from, it means “from everywhere”), so we don’t consider that as much of a plus as the black beans doubling up on potassium, calcium, and magnesium.
So, do enjoy both, but if you’re going to pick, or lean more heavily on one, we recommend the black beans
Further reading
See also:
- Why You’re Probably Not Getting Enough Fiber (And How To Fix It)
- Easily Digestible Vegetarian Protein Sources
- What Matters Most For Your Heart? Eat More (Of This) For Lower Blood Pressure
Enjoy!
Share This Post
-
We Hope This Email Blows Your Tits Clean Off
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Right Kind Of “Email Hacks”!
Are you a Gmailer or an Outlookista? Whatever your preference, you’re probably facing many of the same challenges that most of us face in our work and personal lives:
Email’s greatest strength (its ease of accessibility) brings about its greatest problem (our inboxes are cluttered and chaotic), not to mention that each of us are usually managing a whole flock of email addresses.
Sometimes we put productivity resources up against each other; that’s not what we’re going to do today! Each of these can play a role alongside each other; grab as many as will make your life easier:
ProtonMail: this is an email client; it’s the nicest, simplest, easiest, free email client that doesn’t track, let alone share, everything you do.
Bonus: there also exists ProtonCalendar (it’s a calendar that doesn’t share your data), ProtonDrive (it’s a cloud storage provider that doesn’t share your data) and, because they’re indeed serious about your privacy, ProtonVPN (it’s a VPN that, of course, doesn’t share your data).
Clean Email: maybe you’re stuck with the email provider you have. It happens. But it doesn’t have to be a chaotic mess. This tool will make tidying your email (and keeping it tidy!) a simplified dream.
See How Clean Your Email Can Get With Just A Few Clicks!
Right Inbox: a Gmail extension with many useful features, including read receipts, emails scheduled for later (e.g: time your email to send at 7am to look like a morning lark when in fact you’re peacefully snoozing), add unforwardable “For Your Eyes Only” notes to emails, and more.
Power Up Your Gmail With The Right Inbox Extension!
Email Finder: find the verified work email address of any person, so long as you know what company you’re looking for them in! No more “I thought it was lastname.firstname@ and it was firstname.lastname@”, no more “the wrong John Smith”, no more “undelivered” bounceback notices. Just: your email delivered.
Never Hear From The Mailer Daemon Again, With Email Finder!
Unroll.me: love your subscriptions, but hate the clutter? Unroll.me aggregates them for you in a virtual roll-up, with an “unroll” button to read them.
Get What You Really Want From Your Subscriptions, With Unroll.Me!
On which note, anything you’d like to hear more of from us? Let us know! You can always just hit reply, or use the feedback widget at the bottom of this email
Share This Post
Related Posts
-
STI rates are increasing among midlife and older adults. We need to talk about it
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Globally, the rates of common sexually transmissible infections (STIs) are increasing among people aged over 50. In some cases, rates are rising faster than among younger people.
Recent data from the United States Centers for Disease Control and Prevention shows that, among people aged 55 and older, rates of gonorrhoea and chlamydia, two of the most common STIs, more than doubled between 2012 and 2022.
Australian STI surveillance data has reflected similar trends. Between 2013 and 2022, there was a steady increase in diagnoses of chlamydia, gonorrhoea and syphilis among people aged 40 and older. For example, there were 5,883 notifications of chlamydia in Australians 40 plus in 2013, compared with 10,263 in 2022.
A 2020 study of Australian women also showed that, between 2000 and 2018, there was a sharper increase in STI diagnoses among women aged 55–74 than among younger women.
While the overall rate of common STIs is highest among young adults, the significant increase in STI diagnoses among midlife and older adults suggests we need to pay more attention to sexual health across the life course.
Fit Ztudio/Shutterstock Why are STI rates rising among older adults?
STI rates are increasing globally for all age groups, and an increase among midlife and older people is in line with this trend.
However, increases of STIs among older people are likely due to a combination of changing sex and relationship practices and hidden sexual health needs among this group.
The “boomer” generation came of age in the 60s and 70s. They are the generation of free love and their attitude to sex, even as they age, is quite different to that of generations before them.
Given the median age of divorce in Australia is now over 43, and the internet has ushered in new opportunities for post-separation dating, it’s not surprising that midlife and older adults are exploring new sexual practices or finding multiple sexual partners.
People may start new relationships later in life. Tint Media/Shutterstock It’s also possible midlife and older people have not had exposure to sexual health education in school or do not relate to current safe sex messages, which tend to be directed toward young people. Condoms may therefore seem unnecessary for people who aren’t trying to avoid pregnancy. Older people may also lack confidence negotiating safe sex or accessing STI screening.
Hidden sexual health needs
In contemporary life, the sex lives of older adults are largely invisible. Ageing and older bodies are often associated with loss of power and desirability, reflected in the stereotype of older people as asexual and in derogatory jokes about older people having sex.
With some exceptions, we see few positive representations of older sexual bodies in film or television.
Older people’s sexuality is also largely invisible in public policy. In a review of Australian policy relating to sexual and reproductive health, researchers found midlife and older adults were rarely mentioned.
Sexual health policy generally targets groups with the highest STI rates, which excludes most older people. As midlife and older adults are beyond childbearing years, they also do not feature in reproductive health policy. This means there is a general absence of any policy related to sex or sexual health among midlife or older adults.
Added to this, sexual health policy tends to be focused on risk rather than sexual wellbeing. Sexual wellbeing, including freedom and capacity to pursue pleasurable sexual experiences, is strongly associated with overall health and quality of life for adults of all ages. Including sexual wellbeing as a policy priority would enable a focus on safe and respectful sex and relationships across the adult life course.
Without this priority, we have limited knowledge about what supports sexual wellbeing as people age and limited funding for initiatives to engage with midlife or older adults on these issues.
Midlife and older adults may have limited knowledge about STIs. Southworks/Shutterstock How can we support sexual health and wellbeing for older adults?
Most STIs are easily treatable. Serious complications can occur, however, when STIs are undiagnosed and untreated over a long period. Untreated STIs can also be passed on to others.
Late diagnosis is not uncommon as some STIs can have no symptoms and many people don’t routinely screen for STIs. Older, heterosexual adults are, in general, less likely than other groups to seek regular STI screening.
For midlife or older adults, STIs may also be diagnosed late because some doctors do not initiate testing due to concerns they will cause offence or because they assume STI risk among older people is negligible.
Many doctors are reluctant to discuss sexual health with their older patients unless the patient explicitly raises the topic. However, older people can be embarrassed or feel awkward raising matters of sex.
Resources for health-care providers and patients to facilitate conversations about sexual health and STI screening with older patients would be a good first step.
To address rising rates of STIs among midlife and older adults, we also need to ensure sexual health promotion is targeted toward these age groups and improve accessibility of clinical services.
More broadly, it’s important to consider ways to ensure sexual wellbeing is prioritised in policy and practice related to midlife and older adulthood.
A comprehensive approach to older people’s sexual health, that explicitly places value on the significance of sex and intimacy in people’s lives, will enhance our ability to more effectively respond to sexual health and STI prevention across the life course.
Jennifer Power, Associate Professor and Principal Research Fellow, Australian Research Centre in Sex, Health and Society, La Trobe University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
JoyFull – by Radhi Devlukia-Shetty
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We haven’t done a recipe book in a little while, so here’s a good one!
The focus of this book is getting more plants and spices into your diet, and doing it deliciously.
Healthwise, there is nothing controversial here: the recipes are all plant-based, mostly whole-foods, and the items that aren’t whole foods are things like “vanilla extract”.
The recipes themselves (of which there are 125) are presented clearly and simply, one to a double-page (although sometimes there will be a suggested variation on the same double-page), ideal for use in a kitchen bookstand. For each recipe, there’s a clear photo of the end result, so you know what you’re working towards.
The ingredients are not too obscure, and can be acquired from more or less any large supermarket.
Bottom line: if you’re looking to expand your plant-based cooking repertoire in a way that’s not just substitutions, then this book provides an excellent variety.
Click here to check out JoyFull, and get a taste of Ayurvedic cooking!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Total Recovery – by Dr. Gary Kaplan
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
First, know: Dr. Kaplan is an osteopath, and as such, will be mostly approaching things from that angle. That said, he is also board certified in other things too, including family medicine, so he’s by no means a “one-trick pony”, nor are there “when your only tool is a hammer, everything starts to look like a nail” problems to be found here. Instead, the scope of the book is quite broad.
Dr. Kaplan talks us through the diagnostic process that a doctor goes through when presented with a patient, what questions need to be asked and answered—and by this we mean the deeper technical questions, e.g. “what do these symptoms have in common”, and “what mechanism was at work when the pain become chronic”, not the very basic questions asked in the initial debriefing with the patient.
He also asks such questions (and questions like these get chapters devoted to them) as “what if physical traumas build up”, and “what if physical and emotional pain influence each other”, and then examines how to interrupt the vicious cycles that lead to deterioration of one’s condition.
The style of the book is very pop-science and often narrative in its presentation, giving lots of anecdotes to illustrate the principles. It’s a “sit down and read it cover-to-cover” book—or a chapter a day, whatever your preferred pace; the point is, it’s not a “dip directly to the part that answers your immediate question” book; it’s not a textbook or manual.
Bottom line: a lot of this work is about prompting the reader to ask the right questions to get to where we need to be, but there are many illustrative possible conclusions and practical advices to be found and given too, making this a useful read if you and/or a loved one suffers from chronic pain.
Click here to check out Total Recovery, and solve your own mysteries!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: