Simply The Pits: These Underarm Myths!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Are We Taking A Risk To Smell Fresh As A Daisy?
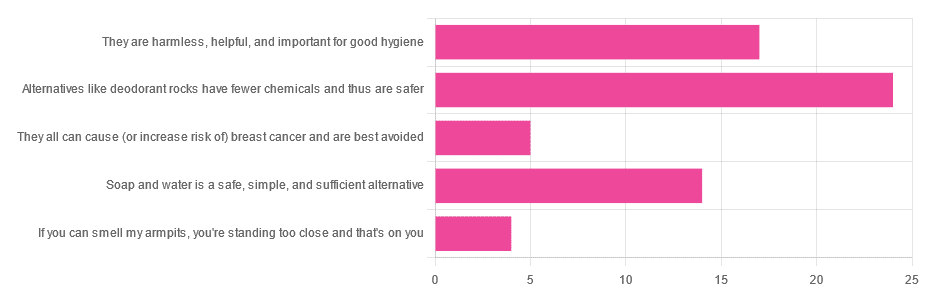
Yesterday, we asked you for your health-related view of underarm deodorants.
So, what does the science say?
They can cause (or increase risk of) cancer: True or False?
False, so far as we know. Obviously it’s very hard to prove a negative, but there is no credible evidence that deodorants cause cancer.
The belief that they do comes from old in vitro studies applying the deodorant directly to the cells in question, like this one with canine kidney tissues in petri dishes:
Antiperspirant Induced DNA Damage in Canine Cells by Comet Assay
Which means that if you’re not a dog and/or if you don’t spray it directly onto your internal organs, this study’s data doesn’t apply to you.
In contrast, more modern systematic safety reviews have found…
❝Neither is there clear evidence to show use of aluminum-containing underarm antiperspirants or cosmetics increases the risk of Alzheimer’s Disease or breast cancer.
Metallic aluminum, its oxides, and common aluminum salts have not been shown to be either genotoxic or carcinogenic.❞
(however, one safety risk it did find is that we should avoid eating it excessively while pregnant or breastfeeding)
Alternatives like deodorant rocks have fewer chemicals and thus are safer: True or False?
True and False, respectively. That is, they do have fewer chemicals, but cannot in scientific terms be qualifiably, let alone quantifiably, described as safer than a product that was already found to be safe.
Deodorant rocks are usually alum crystals, by the way; that is to say, aluminum salts of various kinds. So if it was aluminum you were hoping to avoid, it’s still there.
However, if you’re trying to cut down on extra chemicals, then yes, you will get very few in deodorant rocks, compared to the very many in spray-on or roll-on deodorants!
Soap and water is a safe, simple, and sufficient alternative: True or False?
True or False, depending on what you want as a result!
- If you care that your deodorant also functions as an antiperspirant, then no, soap and water will certainly not have an antiperspirant effect.
- If you care only about washing off bacteria and eliminating odor for the next little while, then yes, soap and water will work just fine.
Bonus myths:
There is no difference between men’s and women’s deodorants, apart from the marketing: True or False?
False! While to judge by the marketing, the only difference is that one smells of “evening lily” and the other smells of “chainsaw barbecue” or something, the real difference is…
- The “men’s” kind is designed to get past armpit hair and reach the skin without clogging the hair up.
- The “women’s” kind is designed to apply a light coating to the skin that helps avoid chafing and irritation.
In other words… If you are a woman with armpit hair or a man without, you might want to ignore the marketing and choose according to your grooming preferences.
Hopefully you can still find a fragrance that suits!
Shaving (or otherwise depilating) armpits is better for hygiene: True or False?
True or False, depending on what you consider “hygiene”.
Consistent with popular belief, shaving means there is less surface area for bacteria to live. And empirically speaking, that means a reduction in body odor:
However, shaving typically causes microabrasions, and while there’s no longer hair for the bacteria to enjoy, they now have access to the inside of your skin, something they didn’t have before. This can cause much more unpleasant problems in the long-run, for example:
❝Hidradenitis suppurativa is a chronic and debilitating skin disease, whose lesions can range from inflammatory nodules to abscesses and fistulas in the armpits, groin, perineum, inframammary region❞
Read more: Hidradenitis suppurativa: Basic considerations for its approach: A narrative review
And more: Hidradenitis suppurativa: Epidemiology, clinical presentation, and pathogenesis
If this seems a bit “damned if you do; damned if you don’t”, this writer’s preferred way of dodging both is to use electric clippers (the buzzy kind, as used for cutting short hair) to trim hers down low, and thus leave just a little soft fuzz.
What you do with yours is obviously up to you; our job here is just to give the information for everyone to make informed decisions whatever you choose 🙂
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How To Keep Warm (Without Sweat Patches!)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝I saw an advert on the subway for a pillow spray that guarantees a perfect night’s sleep. What does the science say about smells/sleep?❞
That is certainly a bold claim! Unless it’s contingent, e.g. “…or your money back”. Because otherwise, it absolutely cannot guarantee that.
There is some merit:
❝Odors can modulate the latency to sleep onset, as well as the quality and duration of sleep. Olfactory modulation of sleep may be mediated by direct synaptic interaction between the olfactory system and sleep control nuclei, and/or indirectly through odor modulation of arousal and respiration.
Such modulation appears most heavily influenced by past associations and expectations about the odor, beyond any potential direct physicochemical effect❞
Source: Reciprocal relationships between sleep and smell
Translating that from sciencese:
Sometimes we find pleasant smells relaxing, and placebo effect also helps.
That “any potential direct physiochemical effect”, though, when it does occur, is things like this…
Read: Odor blocking of stress hormone responses
…but that’s a mouse study, and those odors may only work to block three specific mouse stress responses to three specific stressors: physical restraint, predator odor, and male–male confrontation.
In other words: if, perchance, those three things are not what’s stressing you in bed at night (we won’t make assumptions), and/or you are not a mouse, it may not help.
(and this, dear readers, is why we must read articles, and not just headlines!)
But! If you are going to go for a pillow fragrance, something well-associated with being relaxing and soporific, such as lavender, is the way to go:
- Effects of aromatherapy on sleep quality and anxiety of patients
- Effects of Aromatherapy on the Anxiety, Vital Signs, and Sleep Quality of Percutaneous Coronary Intervention Patients in Intensive Care Units
- Effect of lavender aromatherapy on vital signs and perceived quality of sleep in the intermediate care unit: a pilot study
tl;dr = patients found lavender fragrances relaxing, experienced less anxiety, got better sleep (significantly or insignificantly, depending on the study) and enjoyed lower blood pressure (significantly or insignificantly, depending on the study).
PS: this writer uses a pillow spray like this one
Enjoy!
Share This Post
-
Marathons in Mid- and Later-Life
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
We had several requests pertaining to veganism, meatless mondays, and substitutions in recipes—so we’re going to cover those on a different day!
As for questions we’re answering today…
Q: Is there any data on immediate and long term effects of running marathons in one’s forties?
An interesting and very specific question! We didn’t find an overabundance of studies specifically for the short- and long-term effects of marathon-running in one’s 40s, but we did find a couple of relevant ones:
The first looked at marathon-runners of various ages, and found that…
- there are virtually no relevant running time differences (p<0.01) per age in marathon finishers from 20 to 55 years
- the majority of middle-aged and elderly athletes have training histories of less than seven years of running
From which they concluded:
❝The present findings strengthen the concept that considers aging as a biological process that can be considerably speeded up or slowed down by multiple lifestyle related factors.❞
See the study: Performance, training and lifestyle parameters of marathon runners aged 20–80 years: results of the PACE-study
The other looked specifically at the impact of running on cartilage, controlled for age (45 and under vs 46 and older) and activity level (marathon-runners vs sedentary people).
The study had the people, of various ages and habitual activity levels, run for 30 minutes, and measured their knee cartilage thickness (using MRI) before and after running.
They found that regardless of age or habitual activity level, running compressed the cartilage tissue to a similar extent. From this, it can be concluded that neither age nor marathon-running result in long-term changes to cartilage response to running.
Or in lay terms: there’s no reason that marathon-running at 40 should ruin your knees (unless you are doing something wrong).
That may or may not have been a concern you have, but it’s what the study looked at, so hey, it’s information.
Here’s the study: Functional cartilage MRI T2 mapping: evaluating the effect of age and training on knee cartilage response to running
Q: Information on [e-word] dysfunction for those who have negative reactions to [the most common medications]?
When it comes to that particular issue, one or more of these three factors are often involved:
- Hormones
- Circulation
- Psychology
The most common drugs (that we can’t name here) work on the circulation side of things—specifically, by increasing the localized blood pressure. The exact mechanism of this drug action is interesting, albeit beyond the scope of a quick answer here today. On the other hand, the way that they work can cause adverse blood-pressure-related side effects for some people; perhaps you’re one of them.
To take matters into your own hands, so to speak, you can address each of those three things we just mentioned:
Hormones
Ask your doctor (or a reputable phlebotomy service) for a hormone test. If your free/serum testosterone levels are low (which becomes increasingly common in men over the age of 45), they may prescribe something—such as testosterone shots—specifically for that.
This way, it treats the underlying cause, rather than offering a workaround like those common pills whose names we can’t mention here.
Circulation
Look after your heart health; eat for your heart health, and exercise regularly!
Cold showers/baths also work wonders for vascular tone—which is precisely what you need in this matter. By rapidly changing temperatures (such as by turning off the hot water for the last couple of minutes of your shower, or by plunging into a cold bath), your blood vessels will get practice at constricting and maintaining that constriction as necessary.
Psychology
[E-word] dysfunction can also have a psychological basis. Unfortunately, this can also then be self-reinforcing, if recalling previous difficulties causes you to get distracted/insecure and lose the moment. One of the best things you can do to get out of this catch-22 situation is to not worry about it in the moment. Depending on what you and your partner(s) like to do in bed, there are plenty of other equally respectable options, so just switch track!
Having a conversation about this in advance will probably be helpful, so that everyone’s on the same page of the script in that eventuality, and it becomes “no big deal”. Without that conversation, misunderstandings and insecurities could arise for your partner(s) as well as yourself (“aren’t I desirable enough?” etc).
So, to recap, we recommend:
- Have your hormones checked
- Look after your circulation
- Make the decision to have fun!
Share This Post
-
The Mental Health First-Aid That You’ll Hopefully Never Need
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Take Your Mental Health As Seriously As General Health!
Sometimes, health and productivity means excelling—sometimes, it means avoiding illness and unproductivity. Both are essential, and today we’re going to tackle some ground-up stuff. If you don’t need it right now, great; we suggest to read it for when and if you do. But how likely is it that you will?
- One in four of us are affected by serious mental health issues in any given year.
- One in five of us have suicidal thoughts at some point in our lifetime.
- One in six of us are affected to at least some extent by the most commonly-reported mental health issues, anxiety and depression, in any given week.
…and that’s just what’s reported, of course. These stats are from a UK-based source but can be considered indicative generally. Jokes aside, the UK is not a special case and is not measurably worse for people’s mental health than, say, the US or Canada.
While this is not an inherently cheery topic, we think it’s an important one.
Depression, which we’re going to focus on today, is very very much a killer to both health and productivity, after all.
One of the most commonly-used measures of depression is known by the snappy name of “PHQ9”. It stands for “Patient Health Questionnaire Nine”, and you can take it anonymously online for free (without signing up for anything; it’s right there on the page already):
Take The PHQ9 Test Here! (under 2 minutes, immediate results)
There’s a chance you took that test and your score was, well, depressing. There’s also a chance you’re doing just peachy, or maybe somewhere in between. PHQ9 scores can fluctuate over time (because they focus on the past two weeks, and also rely on self-reports in the moment), so you might want to bookmark it to test again periodically. It can be interesting to track over time.
In the event that you’re struggling (or: in case one day you find yourself struggling, or want to be able to support a loved one who is struggling), some top tips that are useful:
Accept that it’s a medical condition like any other
Which means some important things:
- You/they are not lazy or otherwise being a bad person by being depressed
- You/they will probably get better at some point, especially if help is available
- You/they cannot, however, “just snap out of it”; illness doesn’t work that way
- Medication might help (it also might not)
Do what you can, how you can, when you can
Everyone knows the advice to exercise as a remedy for depression, and indeed, exercise helps many. Unfortunately, it’s not always that easy.
Did you ever see the 80s kids’ movie “The Neverending Story”? There’s a scene in which the young hero Atreyu must traverse the “Swamp of Sadness”, and while he has a magical talisman that protects him, his beloved horse Artax is not so lucky; he slows down, and eventually stops still, sinking slowly into the swamp. Atreyu pulls at him and begs him to keep going, but—despite being many times bigger and stronger than Atreyu, the horse just sinks into the swamp, literally drowning in despair.
See the scene: The Neverending Story movie clip – Artax and the Swamp of Sadness (1984)
Wow, they really don’t make kids’ movies like they used to, do they?
But, depression is very much like that, and advice “exercise to feel less depressed!” falls short of actually being helpful, when one is too depressed to do it.
If you’re in the position of supporting someone who’s depressed, the best tool in your toolbox will be not “here’s why you should do this” (they don’t care; not because they’re an uncaring person by nature, but because they are physiologically impeded from caring about themself at this time), but rather:
“please do this with me”
The reason this has a better chance of working is because the depressed person will in all likelihood be unable to care enough to raise and/or maintain an objection, and while they can’t remember why they should care about themself, they’re more likely to remember that they should care about you, and so will go with your want/need more easily than with their own. It’s not a magic bullet, but it’s worth a shot.
What if I’m the depressed person, though?
Honestly, the same, if there’s someone around you that you do care about; do what you can to look after you, for them, if that means you can find some extra motivation.
But I’m all alone… what now?
Firstly, you don’t have to be alone. There are free services that you can access, for example:
- US: https://nami.org/help
- Canada: https://www.wellnesstogether.ca/en-CA
- UK: https://www.samaritans.org/
…which varyingly offer advice, free phone services, webchats, and the like.
But also, there are ways you can look after yourself a little bit; do the things you’d advise someone else to do, even if you’re sure they won’t work:
- Take a little walk around the block
- Put the lights on when you’re not sleeping
- For that matter, get out of bed when you’re not sleeping. Literally lie on the floor if necessary, but change your location.
- Change your bedding, or at least your clothes
- If changing the bedding is too much, change just the pillowcase
- If changing your clothes is too much, change just one item of clothing
- Drink some water; it won’t magically cure you, but you’ll be in slightly better order
- On the topic of water, splash some on your face, if showering/bathing is too much right now
- Do something creative (that’s not self-harm). You may scoff at the notion of “art therapy” helping, but this is a way to get at least some of the lights on in areas of your brain that are a little dark right now. Worst case scenario is it’ll be a distraction from your problems, so give it a try.
- Find a connection to community—whatever that means to you—even if you don’t feel you can join it right now. Discover that there are people out there who would welcome you if you were able to go join them. Maybe one day you will!
- Hiding from the world? That’s probably not healthy, but while you’re hiding, take the time to read those books (write those books, if you’re so inclined), learn that new language, take up chess, take up baking, whatever. If you can find something that means anything to you, go with that for now, ride that wave. Motivation’s hard to come by during depression and you might let many things slide; you might as well get something out of this period if you can.
If you’re not depressed right now but you know you’re predisposed to such / can slip that way?
Write yourself instructions now. Copy the above list if you like.
Most of all: have a “things to do when I don’t feel like doing anything” list.
If you only take one piece of advice from today’s newsletter, let that one be it!
Share This Post
Related Posts
-
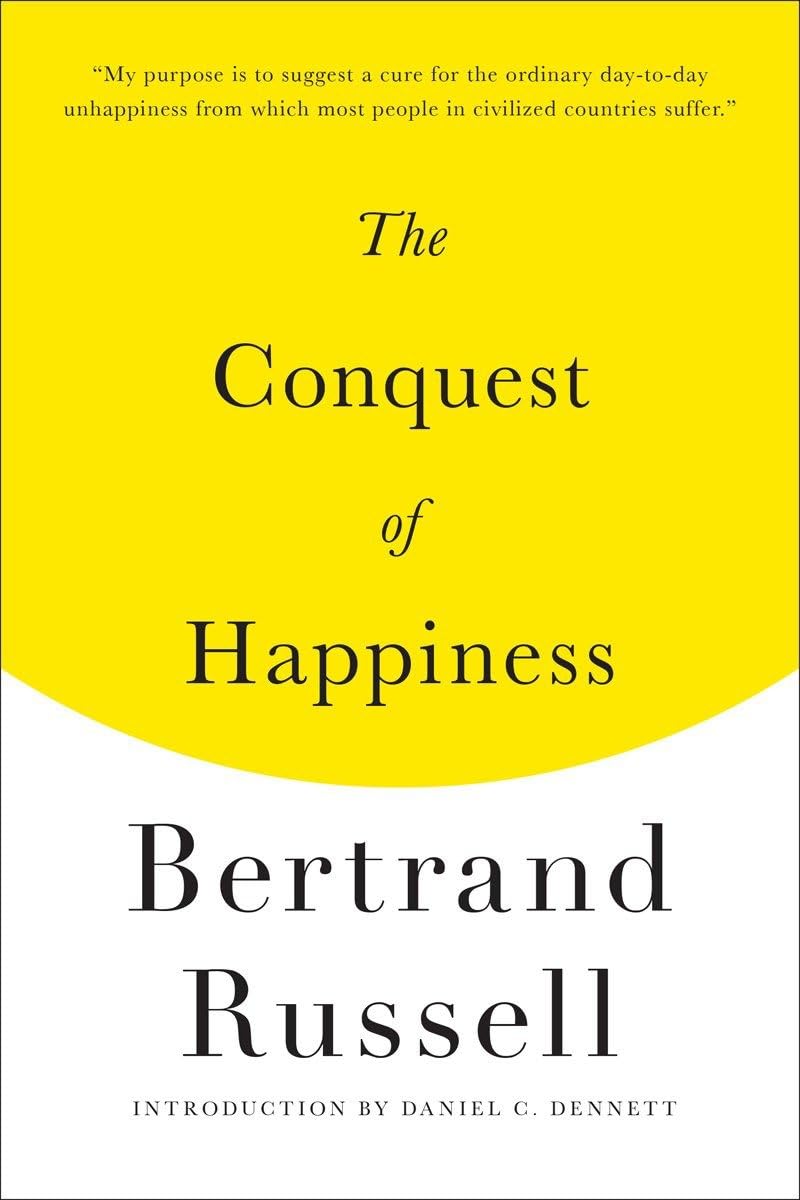
The Conquest of Happiness – by Bertrand Russell
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When we have all our physical needs taken care of, why are we often still not happy, and what can we do about that?
Mathematician, philosopher, and Nobel prizewinner Bertrand Russell has answers. And, unlike many of “the great philosophers”, his writing style is very clear and accessible.
His ideas are simple and practical, yet practised by few. Rather than taking a “be happy with whatever you have” approach, he does argue that we should strive to find more happiness in some areas and ways—and lays out guidelines for doing so.
Areas to expand, areas to pull back on, areas to walk a “virtuous mean”. Things to be optimistic about; things to not get our hopes up about.
Applying Russell’s model, there’s no more “should I…?” moments of wondering which way to jump.
Bottom line: if you’ve heard enough about “how to be happy” from wishy-washier sources, you might find the work of this famous logician refreshing.
Click here to check out The Conquest of Happiness, and see how much happier you might become!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Many Health Benefits Of Garlic
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Many Health Benefits of Garlic
We’re quite confident you already know what garlic is, so we’re going to leap straight in there with some science today:
First, let’s talk about allicin
Allicin is a compound in garlic that gives most of its health benefits. A downside of allicin is that it’s not very stable, so what this means is:
- Garlic is best fresh—allicin breaks down soon after garlic is cut/crushed
- So while doing the paperwork isn’t fun, buying it as bulbs is better than buying it as granules or similar
- Allicin also breaks down somewhat in cooking, so raw garlic is best
- Our philosophy is: still use it in cooking as well; just use more!
- Supplements (capsule form etc) use typically use extracts and potency varies (from not great to actually very good)
Read more about that:
- Short-term heating reduces the anti-inflammatory effects of fresh raw garlic extracts
- Allicin Bioavailability and Bioequivalence from Garlic Supplements and Garlic Foods
Now, let’s talk benefits…
Benefits to heart health
Garlic has been found to be as effective as the drug Atenolol at reducing blood pressure:
It also lowers LDL (bad cholesterol):
Benefits to the gut
We weren’t even looking for this, but as it turns out, as an add-on to the heart benefits…
Benefits to the immune system
Whether against the common cold or bringing out the heavy guns, garlic is a booster:
- Preventing the common cold with a garlic supplement: a double-blind, placebo-controlled survey
- Supplementation with aged garlic extract improves both NK and γδ-T cell function and reduces the severity of cold and flu symptoms: a randomized, double-blind, placebo-controlled nutrition intervention
Benefits to the youthfulness of body and brain
Garlic is high in antioxidants that, by virtue of reducing oxidative stress, help slow aging. This effect, combined with the cholesterol and blood pressure benefits, means it may also reduce the risk of Alzheimer’s and other forms of dementia:
- Antioxidant health effects of aged garlic extract
- Effects of garlic consumption on plasma and erythrocyte antioxidant parameters in elderly subjects
- Garlic reduces heart disease and dementia risk
There are more benefits too…
That’s all we have time to dive into study-wise today, but for the visually-inclined, here are yet more benefits to garlic (at a rate of 3–4 cloves per day):
An incredible awesome recipe using lots of garlic:
- Take small potatoes (still in their skins), cut in half
- Add enough peeled cloves of garlic so that you have perhaps a 1:10 ratio of garlic to potato by mass
- Boil (pressure-cooking is ideal) until soft, and drain
- Keeping them in the pan, add a lashing of olive oil, and any additional seasonings per your preference (consider black pepper, rosemary, thyme, parsley)
- Put a lid on the pan, and holding it closed, shake the pan vigorously
- Note: if you didn’t leave the skins on, or you chopped much larger potatoes smaller instead of cutting in half, the potatoes will break up into a rough mash now. This is actually also fine and still tastes (and honestly, looks) great, but it is different, so just be aware, so that you get the outcome you want.
- The garlic, which—unlike the potatoes—didn’t have a skin to hold it together, will now have melted over the potatoes like butter
You can serve like this (it’s delicious already) or finish up in the oven or air-fryer or under the grill, if you prefer a roasted style dish (an amazing option too).
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
- Garlic is best fresh—allicin breaks down soon after garlic is cut/crushed
-
Black Cohosh vs The Menopause
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Black Cohosh, By Any Other Name…
Black cohosh is a flowering plant whose extracts are popularly used to relieve menopausal (and postmenopausal) symptoms.
Note on terms: we’ll use “black cohosh” in this article, but if you see the botanical names in studies, the reason it sometimes appears as Actaea racemosa and sometimes as Cimicfuga racemosa, is because it got changed and changed back on account of some disagreements between botanists. It’s the same plant, in any case!
Read: Reclassification of Actaea to include Cimicifuga and Souliea (Ranunculaceae)
Does it work?
In few words: it works for physical symptoms, but not emotional ones, based on this large (n=2,310) meta-analysis of studies:
❝Black cohosh extracts were associated with significant improvements in overall menopausal symptoms (Hedges’ g = 0.575, 95% CI = 0.283 to 0.867, P < 0.001), as well as in hot flashes (Hedges’ g = 0.315, 95% CIs = 0.107 to 0.524, P = 0.003), and somatic symptoms (Hedges’ g = 0.418, 95% CI = 0.165 to 0.670, P = 0.001), compared with placebo.
However, black cohosh did not significantly improve anxiety (Hedges’ g = 0.194, 95% CI = -0.296 to 0.684, P = 0.438) or depressive symptoms (Hedges’ g = 0.406, 95% CI = -0.121 to 0.932, P = 0.131)❞
~ Dr. Ryochi Sadahiro et al., 2023
Source: Black cohosh extracts in women with menopausal symptoms: an updated pairwise meta-analysis
Here’s an even larger (n=43,759) one that found similarly, and also noted on safety:
❝Treatment with iCR/iCR+HP was well tolerated with few minor adverse events, with a frequency comparable to placebo. The clinical data did not reveal any evidence of hepatotoxicity.
Hormone levels remained unchanged and estrogen-sensitive tissues (e.g. breast, endometrium) were unaffected by iCR treatment.
As benefits clearly outweigh risks, iCR/iCR+HP should be recommended as an evidence-based treatment option for natural climacteric symptoms.
With its good safety profile in general and at estrogen-sensitive organs, iCR as a non-hormonal herbal therapy can also be used in patients with hormone-dependent diseases who suffer from iatrogenic climacteric symptoms.❞
~ Dr. Castelo-Branco et al., 2020
(iCR = isopropanolic Cimicifuga racemosa)
So, is this estrogenic or not?
This is the question many scientists were asking, about 20 or so years ago. There are many papers from around 2000–2005, but here’s a good one that’s quite representative:
❝These new data dispute the estrogenic theory and demonstrate that extracts of black cohosh do not bind to the estrogen receptor in vitro, up-regulate estrogen-dependent genes, or stimulate the growth of estrogen-dependent tumors❞
Source: Is Black Cohosh Estrogenic?
(the abstract is a little vague, but if you click on the PDF icon, you can read the full paper, which is a lot clearer and more detailed)
The short answer: no, black cohosh is not estrogenic
Is it safe?
As ever, check with your doctor as everyone’s situation can vary, but broadly speaking, yes, it has a very good safety profile—including for breast cancer patients, at that. See for example:
- Black cohosh efficacy and safety for menopausal symptoms: the Spanish Menopause Society statement
- Black cohosh (Cimicifuga racemosa): safety and efficacy for cancer patients
- The safety of black cohosh (Actaea racemosa, Cimicifuga racemosa)
Where can I get some?
We don’t sell it, but here for your convenience is an example product on Amazon
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: