Death by Food Pyramid – by Denise Minger
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This one is less about “here’s the perfect way of eating” or even “these specific foods are ontologically evil”, but more about teaching science literacy.
The author explores various health trends from the 70s until time of writing (the book was published in 2014), what rationales originally prompted them, and what social phenomena either helped them to persist, or caused them to get dropped quite quickly.
Of course, even in the case of fads that are societally dropped quite quickly, on an individual level there will always be someone just learning about it for the first time, reading some older material, and thinking “that sounds like just the miracle life-changer I need!”
What she teaches the reader to do is largely what we do a lot of here at 10almonds—examine the claims, go to the actual source material (studies! Not just books about studies!), and see whether the study conclusions actually support the claim, to start with, and then further examine to see if there’s some way (or sometimes, a plurality of ways) in which the study itself is methodologically flawed.
Which does happen sometimes, do actually watch out for that!
The style is quite personal and entertaining for the most part, and yet even moving sometimes (the title is not hyperbole; deaths will be discussed). As one might expect of a book teaching science literacy, it’s very easy to read, with copious footnotes (well, actually they are at the back of the book doubling up as a bibliography, but they are linked-to throughout) for those who wish to delve deeper—something the author, of course, encourages.
Bottom line: if you’d like to be able to sort the real science from the hype yourself, then this book can set you on the right track!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Modern Friendship – by Anna Goldfarb
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s a topic we’ve covered before at 10almonds: Human Connection In An All-Too-Busy World.
Here, however, Goldfarb has an entire book to cover what we had one article to cover, so of course it’s a lot more in-depth.
Importantly, if also covers: what if you seem to be doing everything right, and it’s still not working out? What if you’re already reaching out, suggesting things, doing your part?
Piece by piece, she uncovers what the very many problems are, ranging from availability issues and priorities, to health concerns and financial difficulties, to challenges as diverse as trust issues and exhaustion, and much more.
After all the hard truths about modern friendship, she gets onto equally cheery topics such as why friendships fail, but fear not, solutions are forthcoming too—and indeed, that’s what most of the book is about.
Covering such topics as desire, diligence, and delight, we learn how to not only practise wholehearted friendship, but also, how to matter to others, too. She finishes up with a “14-day friendship cleanse”, which sounds a lot more alarming than it actually is.
The style is interesting, being personal and, well, friendly throughout—but still with scholarly citations as we go along, and actual social science rather than mere conjecture.
Bottom line: if you find that your friendships are facing challenges, this book can help you to get to the bottom of any problems and move forwards (likely doing so together).
Click here to check out Modern Friendship, and learn how to truly nurture and grow your connections!
Share This Post
-
Can You Be Fat AND Fit?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The short answer is “yes“.
And as for what that means for your heart and/or all-cause mortality risk: it’s just as good as being fit at a smaller size, and furthermore, it’s better than being less fit at a smaller size.
Here’s the longer answer:
The science
A research team did a systematic review looking at multiple large cohort studies examining the associations between:
- Cardiorespiratory fitness and cardiovascular disease risk
- Cardiorespiratory fitness and all-cause mortality
- BMI and cardiovascular disease risk
- BMI and all-cause mortality
However, they also took this further, and tabulated the data such that they could also establish the cardiovascular disease mortality risk and all-cause mortality risk of:
- Unfit people with “normal” BMI
- Unfit people with “overweight” BMI
- Unfit people with “obese” BMI
- Fit people with “normal” BMI
- Fit people with “overweight” BMI
- Fit people with “obese” BMI
Before we move on, let’s note for the record that BMI is a woeful system in any case, for enough reasons to fill a whole article:
Now, with that in mind, let’s get to the results:
What they found
For cardiovascular disease mortality risk of unfit people specifically, compared to fit people of “normal” BMI:
- Unfit people with “normal” BMI: 2.04x higher risk.
- Unfit people with “overweight” BMI: 2.58x higher risk.
- Unfit people with “obese” BMI: 3.35x higher risk
So here we can see that if you are unfit, then being heavier will indeed increase your CVD mortality risk.
For all-cause mortality risk of unfit people specifically, compared to fit people of “normal” BMI:
- Unfit people with “normal” BMI: 1.92x higher risk.
- Unfit people with “overweight” BMI: 1.82x higher risk.
- Unfit people with “obese” BMI: 2.04x higher risk
This time we see that if you are unfit, then being heavier or lighter than “overweight” will increase your all-cause mortality risk.
So, what about if you are fit? Then being heavier or lighter made no significant difference to either CVD mortality risk or all-cause mortality risk.
Fit individuals, regardless of weight category (normal, overweight, or obese), had significantly lower mortality risks compared to unfit individuals in any weight category.
Note: not just “compared to unfit individuals in their weight category”, but compared to unfit individuals in any weight category.
In other words, if you are obese and have good cardiorespiratory fitness, you will (on average) live longer than an unfit person with “normal” BMI.
You can find the paper itself here, if you want to examine the data and/or method:
Cardiorespiratory fitness, body mass index and mortality: a systematic review and meta-analysis
Ok, so how do I improve the kind of fitness that they measured?
They based their cardiorespiratory fitness on VO2 Max, which scientific consensus holds to be a good measure of how efficiently your body can use oxygen—thus depending on your heart and lungs being healthy.
If you use a fitness tracker that tracks your exercise and your heart rate, it will estimate your VO2 Max for you—to truly measure the VO2 Max itself directly, you’ll need a lot more equipment; basically, access to a lab that tests this. But the estimates are fairly accurate, and so good enough for most personal purposes that aren’t hard-science research.
Next, you’ll want to do this:
53 Studies Later: The Best Way to Improve VO2 Max
Take care!
Share This Post
-
Montana Eyes $30M Revamp of Mental Health, Developmental Disability Facilities
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
HELENA, Mont. — As part of a proposed revamping of the state’s behavioral health system, Republican Gov. Greg Gianforte’s administration is looking into moving a facility for people with developmental disabilities, beefing up renovations at the Montana State Hospital, and creating a Helena unit of that psychiatric hospital.
The changes, backers say, would fill gaps in services and help people better prepare for life outside of the locked, secure setting of the two state facilities before they reenter their own communities.
“I think part of the theme is responsibly moving people in and out of the state facilities so that we create capacity and have people in the appropriate places,” state Sen. Dave Fern (D-Whitefish) said of the proposed capital projects during a recent interview.
Fern served on the Behavioral Health System for Future Generations Commission, a panel created by a 2023 law to suggest how to spend $300 million to revamp the system. The law set aside the $300 million for improving state services for people with mental illness, substance abuse disorders, and developmental disabilities.
Gianforte’s proposed budget for the next two years would spend about $100 million of that fund on 10 other recommendations from the commission. The capital projects are separate ideas for using up to $32.5 million of the $75 million earmarked within the $300 million pool of funds for building new infrastructure or remodeling existing buildings.
The state Department of Public Health and Human Services and consultants for the behavioral health commission presented commission members with areas for capital investments in October. In December, the commission authorized state health department director Charlie Brereton to recommend the following projects to Gianforte:
- Move the 12-bed Intensive Behavior Center for people with developmental disabilities out of Boulder, possibly to either Helena or Butte, at an estimated cost of up to $13.3 million.
- Establish a “step-down” facility of about 16 beds, possibly on the campus of Shodair Children’s Hospital in Helena, to serve adults who have been committed to the Montana State Hospital but no longer need the hospital’s intensive psychiatric services.
- Invest $19.2 million to upgrade the Montana State Hospital’s infrastructure and buildings at Warm Springs, on top of nearly $16 million appropriated in 2023 for renovations already underway there in an effort to regain federal certification of the facility.
The state Architecture & Engineering Division is reviewing the health department’s cost estimates and developing a timeline for the projects so the information can be sent to the governor. Gianforte ultimately must approve the projects.
Health department officials have said they plan to take the proposals to legislative committees as needed. “With Commission recommendation and approval from the governor, the Department believes that it has the authority to proceed with capital project expenditures but must secure additional authority from the Legislature to fund operations into future biennia,” said department spokesperson Jon Ebelt.
The department outlined its facility plans to the legislature’s health and human services budget subcommittee on Jan. 22 as part of a larger presentation on the commission’s work and the 10 noncapital proposals in the governor’s budget. Time limits prevented in-depth discussion and public comment on the facility-related ideas.
One change the commission didn’t consider: moving the Montana State Hospital to a more populated area from its rural and relatively remote location near Anaconda, in southwestern Montana, in an attempt to alleviate staffing shortages.
“The administration is committed to continuing to invest in MSH as it exists today,” Brereton told the commission in October, referring to the Montana State Hospital.
The hospital provides treatment to people with mental illness who have been committed to the state’s custody through a civil or criminal proceeding. It’s been beset by problems, including the loss of federal Medicaid and Medicare funding due to decertification by the federal government in April 2022, staffing issues that have led to high use of expensive traveling health care providers, and turnover in leadership.
State Sen. Chris Pope (D-Bozeman) was vice chair of a separate committee that met between the 2023 and 2025 legislative sessions and monitored progress toward a 2023 legislative mandate to transition patients with dementia out of the state hospital. He agreed in a recent interview that improving — not moving — MSH is a top priority for the system right now.
“Right now, we have an institution that is failing and needs to be brought back into the modern age, where it is located right now,” he said after ticking off a list of challenges facing the hospital.
State Sen. John Esp (R-Big Timber) also noted at the October commission meeting that moving the hospital was likely to run into resistance in any community considered for a new facility.
Fern, the Whitefish senator, questioned in October whether similar concerns might exist for moving the Intensive Behavior Center out of Boulder. For more than 130 years, the town 30 miles south of Helena has been home, in one form or another, to a state facility for people with developmental disabilities. But Brereton said he believes relocation could succeed with community and stakeholder involvement.
The 12-bed center in Boulder serves people who have been committed by a court because their behaviors pose an immediate risk of serious harm to themselves or others. It’s the last residential building for people with developmental disabilities on the campus of the former Montana Developmental Center, which the legislature voted in 2015 to close.
Drew Smith, a consultant with the firm Alvarez & Marsal, told the commission in October that moving the facility from the town of 1,300 to a bigger city such as Helena or Butte would provide access to a larger labor pool, possibly allow a more homelike setting for residents, and open more opportunities for residents to interact with the community and develop skills for returning to their own communities.
Ideally, Brereton said, the center would be colocated with a new facility included in the governor’s proposed budget, for crisis stabilization services to people with developmental disabilities who are experiencing significant behavioral health issues.
Meanwhile, the proposed subacute facility with up to 16 beds for state hospital patients would provide a still secure but less structured setting for people who no longer need intensive treatment at Warm Springs but aren’t yet ready to be discharged from the hospital’s care. Brereton told the commission in October the facility would essentially serve as a less restrictive “extension” of the state hospital. He also said the agency would like to contract with a company to staff the subacute facility.
Health department officials don’t expect the new facility to involve any construction costs. Brereton has said the agency believes an existing building on the Shodair campus would be a good spot for it.
The state began leasing the building Nov. 1 for use by about 20 state hospital patients displaced by the current remodeling at Warm Springs — a different purpose than the proposed subacute facility.
Shodair CEO Craig Aasved said Shodair hasn’t committed to having the state permanently use the building as the step-down facility envisioned by the agency and the commission.
But Brereton said the option is attractive to the health department now that the building has been set up and licensed to serve adults.
“It seems like a natural place to start,” he told the commission in December, “and we don’t mind that it’s in our backyard here in Helena.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
This article first appeared on KFF Health News and is republished here under a Creative Commons license.
Share This Post
Related Posts
-
Cognitive Enhancement Without Drugs
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Cognitive Enhancement Without Drugs
This is Elizabeth Ricker. She’s a Harvard-and-MIT-trained neuroscientist and researcher, who now runs the “Citizen Science” DIY-neurohacking organization, NeuroEducate.
Sounds fun! What’s it about?
The philosophy that spurs on her research and practice can be summed up as follows:
❝I’m not going to leave my brain up to my doctor or [anyone else]… My brain is my own responsibility, and I’m going to do the best that I can to optimize it❞
Her goal is not just to optimize her own brain though; she wants to make the science accessible to everyone.
What’s this about Citizen Science?
“Citizen Science” is the idea that while there’s definitely an important role in society for career academics, science itself should be accessible to all. And, not just the conclusions, but the process too.
This can take the form of huge experiments, often facilitated these days by apps where we opt-in to allow our health metrics (for example) to be collated with many thousands of others, for science. It can also involve such things as we talked about recently, getting our own raw genetic data and “running the numbers” at home to get far more comprehensive and direct information than the genetic testing company would ever provide us.
For Ricker, her focus is on the neuroscience side of biohacking, thus, neurohacking.
I’m ready to hack my brain! Do I need a drill?
Happily not! Although… Bone drills for the skull are very convenient instruments that make it quite hard to go wrong even with minimal training. The drill bit has a little step/ledge partway down, which means you can only drill through the thickness of the skull itself, before the bone meeting the wider part of the bit stops you from accidentally drilling into the brain. Still, please don’t do this at home.
What you can do at home is a different kind of self-experimentation…
If you want to consider which things are genuinely resulting in cognitive enhancement and which things are not, you need to approach the matter like a scientist. That means going about it in an organized fashion, and recording results.
There are several ways cognitive enhancement can be measured, including:
- Learning and memory
- Executive function
- Emotional regulation
- Creative intelligence
Let’s look at each of them, and what can be done. We don’t have a lot of room here; we’re a newsletter not a book, but we’ll cover one of Ricker’s approaches for each:
Learning and memory
This one’s easy. We’re going to leverage neuroplasticity (neurons that fire together, wire together!) by simple practice, and introduce an extra element to go alongside your recall. Perhaps a scent, or a certain item of clothing. Tell yourself that clinical studies have shown that this will boost your recall. It’s true, but that’s not what’s important; what’s important is that you believe it, and bring the placebo effect to bear on your endeavors.
You can test your memory with word lists, generated randomly by AI, such as this one:
You’ll soon find your memory improving—but don’t take our word for it!
Executive function
Executive function is the aspect of your brain that tells the other parts how to work, when to work, and when to stop working. If you’ve ever spent 30 minutes thinking “I need to get up” but you were stuck in scrolling social media, that was executive dysfunction.
This can be trained using the Stroop Color and Word Test, which shows you words, specifically the names of colors, which will themselves be colored, but not necessarily in the color the word pertains to. So for example, you might be shown the word “red”, colored green. Your task is to declare either the color of the word only, ignoring the word itself, or the meaning of the word only, ignoring its appearance. It can be quite challenging, but you’ll get better quite quickly:
The Stroop Test: Online Version
Emotional Regulation
This is the ability to not blow up angrily at the person with whom you need to be diplomatic, or to refrain from laughing when you thought of something funny in a sombre situation.
It’s an important part of cognitive function, and success or failure can have quite far-reaching consequences in life. And, it can be trained too.
There’s no online widget for this one, but: when and if you’re in a position to safely* do so, think about something that normally triggers a strong unwanted emotional reaction. It doesn’t have to be something life-shattering, but just something that you feel in some way bad about. Hold this in your mind, sit with it, and practice mindfulness. The idea is to be able to hold the unpleasant idea in your mind, without becoming reactive to it, or escaping to more pleasant distractions. Build this up.
*if you perchance have PTSD, C-PTSD, or an emotional regulation disorder, you might want to talk this one through with a qualified professional first.
Creative Intelligence
Another important cognitive skill, and again, one that can be cultivated and grown.
The trick here is volume. A good, repeatable test is to think of a common object (e.g. a rock, a towel, a banana) and, within a time constraint (such as 15 minutes) list how many uses you can think of for that item.
Writer’s storytime: once upon a time, I was sorting through an inventory of medical equipment with a colleague, and suggested throwing out our old arterial clamps, as we had newer, better ones—in abundance. My colleague didn’t want to part with them, so I challenged him “Give me one use for these, something we could in some possible world use them for that the new clamps don’t do better, and we’ll keep them”. He said “Thumbscrews”, and I threw my hands up in defeat, saying “Fine!”, as he had technically fulfilled my condition.
What’s the hack to improve this one? Just more volume. Creativity, as it turns out, isn’t something we can expend—like a muscle, it grows the more we use it. And because the above test is repeatable (with different objects), you can track your progress.
And if you feel like using your grown creative muscle to write/paint/compose/etc your magnum opus, great! Or if you just want to apply it to the problem-solving of everyday life, also great!
In summary…
Our brain is a wonderful organ with many functions. Society expects us to lose these as we get older, but the simple, scientific truth is that we can not only maintain our cognitive function, but also enhance and grow it as we go.
Want to know more from today’s featured expert?
You might enjoy her book, “Smarter Tomorrow”, which we reviewed back in March
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
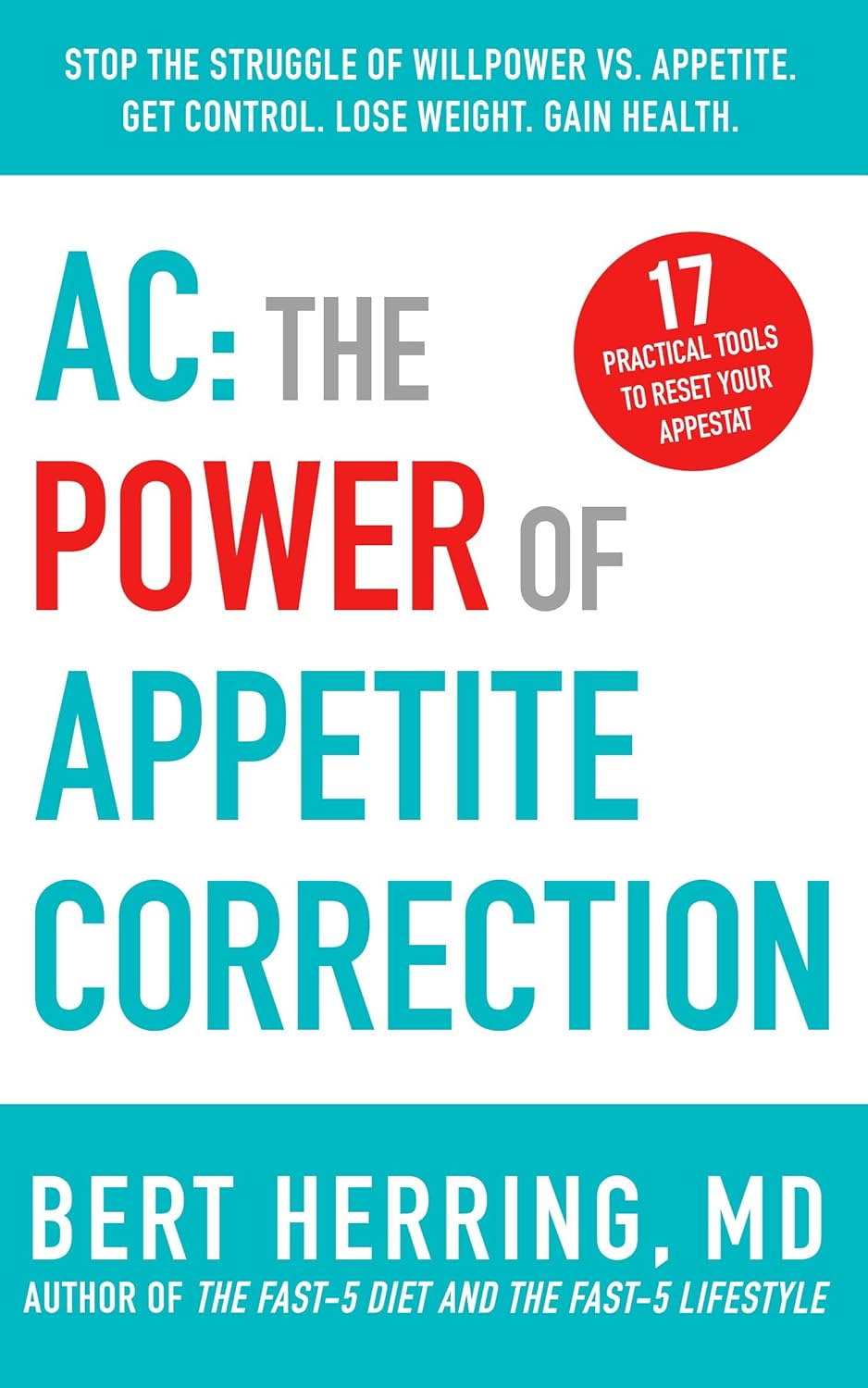
AC: The Power of Appetite Correction – by Dr. Bert Herring
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
“Appetite Correction” is an intriguing concept, and so it intrigued us sufficiently to read this book. So what’s it about?
It’s about modifying our response to hunger, and treating it as a messenger to whom we may say “thank you for your opinion” and then do as we already planned to do. And what is that?
Simply, this book is about intermittent fasting, specifically, 19:5 fasting, i.e., fast for 19 hours and eat during a 5hr window each day (the author proposes 5pm–10pm, but honestly, go with what works for you).
During the fasting period, drinking water, or consuming other non insulin-signalling things (e.g. black coffee, black tea, herbal tea, etc) is fine, but not so much as a bite of anything else (nor calorific drinks, e.g. with milk/cream or sugar in, and certainly not sodas, juices, etc).
During the eating period, the idea is to eat at will without restriction (even unhealthy things, if such is your desire) during those 5 hours, with the exception that one should start with something healthy. In other words, you can line up that take-out if you want, but eat a carrot first to break the fast. Or some nuts. Or whatever, but healthy.
The “appetite correction” part of it comes in with how, after a short adjustment period, you will get used to not suffering from hunger during the fasting period, and during the eating period, you will—paradoxically—be more able to practise moderation in your portions.
Most of the book is given over the dealing with psychological difficulties/objections, as well as some social objections, but he does also explain some of the science at hand too (i.e. how intermittent fasting works, on a physiological level). On which note…
The style is on the very light end of pop-science, and unusually, he doesn’t cite any sources for his claims at all. Now, no science that he claimed struck this reviewer as out of the ordinary, but it would have been nice to see a good few pages of bibliography at the back.
Bottom line: this is a super quick-and-easy read that makes a strong (albeit unsourced) case for intermittent fasting. It’s probably best for someone who would like the benefits and needs some persuading, but who is not very interested in delving into the science beyond being content to understand what is explained and put it into practice.
Click here to check out AC: The Power of Appetite Correction, and get yours where you want it!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Reduce Your Skin Tag Risk
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝As I get older, I seem to be increasingly prone to skin tags, which appear, seemingly out of nowhere, on my face, chest and back. My dermatologist happily burns them off – but is there anything I can do to prevent them?!❞
Not a lot! But, potentially something.
The main risk factor for skin tags is genetic, and you can’t change that in any easy way.
The other main risk factors are connected to each other:
Skin folds, and chafing
Skin tags mostly appear where chafing happens. This can be, for example:
- Inside joint articulations (especially groin and armpits)
- Between fat rolls (if you have them)
So, if you have fat rolls, then losing weight will also reduce the risk of skin tags.
Additionally, obesity and some often-related problems such as diabetes, hypertension, and an atherogenic lipid profile also increase the risk of skin tags (amongst other more serious things):
See: Association of Skin Tag with Metabolic Syndrome and its Components
As for the chafing, this can be reduced in various ways, including:
- losing weight if (and only if) you are carrying excess weight
- dressing against chafing (consider your underwear choices, for example)
- keeping hair in the armpits and groin (it’s part of what it’s there for)
See also: Simply The Pits: These Underarm Myths!
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: