Could my glasses be making my eyesight worse?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
So, you got your eyesight tested and found out you need your first pair of glasses. Or you found out you need a stronger pair than the ones you have. You put them on and everything looks crystal clear. But after a few weeks things look blurrier without them than they did before your eye test. What’s going on?
Some people start to wear spectacles for the first time and perceive their vision is “bad” when they take their glasses off. They incorrectly interpret this as the glasses making their vision worse. Fear of this might make them less likely to wear their glasses.
But what they are noticing is how much better the world appears through the glasses. They become less tolerant of a blurry world when they remove them.
Here are some other things you might notice about eyesight and wearing glasses.
Lazy eyes?
Some people sense an increasing reliance on glasses and wonder if their eyes have become “lazy”.
Our eyes work in much the same way as an auto-focus camera. A flexible lens inside each eye is controlled by muscles that let us focus on objects in the distance (such as a footy scoreboard) by relaxing the muscle to flatten the lens. When the muscle contracts it makes the lens steeper and more powerful to see things that are much closer to us (such as a text message).
From the age of about 40, the lens in our eye progressively hardens and loses its ability to change shape. Gradually, we lose our capacity to focus on near objects. This is called “presbyopia” and at the moment there are no treatments for this lens hardening.
Optometrists correct this with prescription glasses that take the load of your natural lens. The lenses allow you to see those up-close images clearly by providing extra refractive power.
Once we are used to seeing clearly, our tolerance for blurry vision will be lower and we will reach for the glasses to see well again.
The wrong glasses?
Wearing old glasses, the wrong prescription (or even someone else’s glasses) won’t allow you to see as well as possible for day-to-day tasks. It could also cause eyestrain and headaches.
Incorrectly prescribed or dispensed prescription glasses can lead to vision impairment in children as their visual system is still in development.
But it is more common for kids to develop long-term vision problems as a result of not wearing glasses when they need them.
By the time children are about 10–12 years of age, wearing incorrect spectacles is less likely to cause their eyes to become lazy or damage vision in the long term, but it is likely to result in blurry or uncomfortable vision during daily wear.
Registered optometrists in Australia are trained to assess refractive error (whether the eye focuses light into the retina) as well as the different aspects of ocular function (including how the eyes work together, change focus, move around to see objects). All of these help us see clearly and comfortably.

What about dirty glasses?
Dirty or scratched glasses can give you the impression your vision is worse than it actually is. Just like a window, the dirtier your glasses are, the more difficult it is to see clearly through them. Cleaning glasses regularly with a microfibre lens cloth will help.
While dirty glasses are not commonly associated with eye infections, some research suggests dirty glasses can harbour bacteria with the remote but theoretical potential to cause eye infection.
To ensure best possible vision, people who wear prescription glasses every day should clean their lenses at least every morning and twice a day where required. Cleaning frames with alcohol wipes can reduce bacterial contamination by 96% – but care should be taken as alcohol can damage some frames, depending on what they are made of.
When should I get my eyes checked?
Regular eye exams, starting just before school age, are important for ocular health. Most prescriptions for corrective glasses expire within two years and contact lens prescriptions often expire after a year. So you’ll need an eye check for a new pair every year or so.
Kids with ocular conditions such as progressive myopia (short-sightedness), strabismus (poor eye alignment), or amblyopia (reduced vision in one eye) will need checks at least every year, but likely more often. Likewise, people over 65 or who have known eye conditions, such as glaucoma, will be recommended more frequent checks.

An online prescription estimator is no substitute for a full eye examination. If you have a valid prescription then you can order glasses online, but you miss out on the ability to check the fit of the frame or to have them adjusted properly. This is particularly important for multifocal lenses where even a millimetre or two of misalignment can cause uncomfortable or blurry vision.
Conditions such as diabetes or high blood pressure, can affect the eyes so regular eye checks can also help flag broader health issues. The vast majority of eye conditions can be treated if caught early, highlighting the importance of regular preventative care.
James Andrew Armitage, Professor of Optometry and Course Director, Deakin University and Nick Hockley, Lecturer in Optometric Clinical Skills, Director Deakin Collaborative Eye Care Clinic, Deakin University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Kettlebell Swings Are Not What Most People Think They Are (They’re Better)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Commonly assumed to be mostly a shoulders-and-arms exercise, they’re actually mostly about the hips and core:
From the hips
Correctly executed kettlebell swings primarily strengthens muscles from the hamstrings and glutes the to abs and back; in other words, muscles whose strength is essential for power, posture, and injury prevention.
The core in particular is not to be underestimated, with deep stabilizing muscles supporting posture, balance, and movement. Strengthening these areas can also help reduce lower back pain.
How to do it correctly: start with your feet shoulder-width apart (this is important, if you like having knees) and grip the kettlebell with both hands. Hinge at your hips, lowering the kettlebell between your legs while keeping your back flat and core engaged. Then, drive your hips forward explosively to swing the kettlebell up to shoulder height before allowing it to return down with control. The most common mistake is using the arms to lift the kettlebell, but the real power should come from the hips to maximize benefits and prevent injury.
Example workout: 30 seconds of kettlebell swings followed by 30 seconds of rest, repeated for 10 sets. This 10-minute routine provides a full-body workout that builds strength and endurance. As you progress, you can increase the weight, duration, number of sets, etc.
Timeline of changes: within a few weeks of regular kettlebell swings, you should notice stronger glutes, better endurance, and improved posture. After a month, you may experience reduced lower back pain (if you had lower back pain) and more power in your everyday movements. By two to three months, visible muscle definition and fat loss are likely to become noticeable, along with increased overall strength.
For more on all of this plus visual demonstrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like:
Body Sculpting with Kettlebells for Women – by Lorna Kleidman
Take care!
Share This Post
-
Brave – by Dr. Margie Warrell
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Whether it’s the courage to jump out of a plane or the courage to have a difficult conversation, bravery is an important quality that we often don’t go far out of our way to grow. At least, not as adults.
Rather than viewing bravery as a static attribute—you either have it or you don’t—psychologist Dr. Margie Warrell makes the case for its potential for lifelong development.
The book is divided into five sections:
- Live purposefully
- Speak bravely
- Work passionately
- Dig deep
- Dare boldly
…and each has approximately 10 chapters, each a few pages long, the kind that can easily make this a “chapter-a-day” daily reader.
As a quick clarification: that “speak bravely” section isn’t about public speaking, but is rather about speaking up when it counts. Life is too short for regrets, and our interactions with others tend to be what matters most in the long-run. It makes a huge difference to our life!
Dr. Warrell gives us tools to reframe our challenges and tackle them. Rather than just saying “Feel the fear and do it anyway”, she also delivers the how, in all aspects. This is one of the main values the book brings, as well as a sometimes-needed reminder of how and why being brave is something to which we should always aspire… and hold.
Bottom line: if you’d like to be more brave—in any context—this book can help. We only get one life; might as well live it.
Share This Post
-
Body Language (In The Real World)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Forget What You Think You Know About Body Language
…unless it’s about a specific person whose habits and mannerisms you know intimately, in which case, you probably have enough personal data stored up to actually recognize patterns à la “when my spouse does this, then…”, and probably do know what’s going on.
For everyone else… our body language can be as unique as our idiolect
What’s an idiolect? It’s any one given person’s way of speaking/writing, in their natural state (i.e. without having to adjust their style for some reason, for example in a public-facing role at work, where style often becomes much narrower and more consciously-chosen).
Extreme example first
To give an extreme example of how non-verbal communication can be very different than a person thinks, there’s an anecdote floating around the web of someone whose non-verbal autistic kid would, when he liked someone who was visiting the house, hide their shoes when they were about to leave, to cause them to stay longer. Then one day some relative visited and when she suggested that she “should be going sometime soon”, he hurried to bring her her shoes. She left, happy that the kid liked her (he did not).
The above misunderstanding happened because the visitor had the previous life experience of “a person who brings me things is being helpful, and if they do it of their own free will, it’s because they like me”.
In other words…
Generalizations are often sound… In general
…which does not help us when dealing with individuals, which as it turns out, everyone is.
Clenched fists = tense and angry… Except when it’s just what’s comfortable for someone, or they have circulation issues, or this, or that, or the other.
Pacing = agitated… Except when it’s just someone who finds the body in motion more comfortable
Relaxed arms and hands = at ease and unthreatening… Unless it’s a practitioner of various martial arts for whom that is their default ready-for-action state.
Folded arms = closed-off, cold, distant… Or it was just somewhere to put one’s hands.
Lack of eye contact = deceitful, hiding something… Unless it’s actually for any one of a wide number of reasons, which brings us to our next section:
A liar’s “tells”
Again, if you know someone intimately and know what signs are associated with deceit in them, then great, that’s a thing you know. But for people in general…
A lot of what is repeated about “how to know if someone is lying” has seeped into public consciousness from “what police use to justify their belief that someone is lying”.
This is why many of the traditional “this person is lying” signs are based around behaviors that show up when in fact “this person is afraid, under pressure, and talking to an authority figure who has the power to ruin their life”:
Research on Non-verbal Signs of Lies and Deceit: A Blind Alley
But what about eye-accessing cues? They have science to them, right?
For any unfamiliar: this is about the theory that when we are accessing different parts of our mind (such as memory or creativity, thus truthfulness or lying), our eyes move one way or another according to what faculty we’re accessing.
Does it work? No
But, if you carefully calibrate it for a specific person, such as by asking them questions along the lines of “describe your front door” or “describe your ideal holiday”, to see which ways they look for recall or creativity… Then also no:
The Eyes Don’t Have It: Lie Detection and Neuro-Linguistic Programming
How can we know what non-verbal communication means, then?
With strangers? We can’t, simply. It’s on us to be open-minded, with a healthy balance of optimism and wariness.
With people we know? We can build up a picture over time, learn the person’s patterns. Best of all, we can ask them. In the moment, and in general.
For more on optimizing interpersonal communication, check out:
Save Time With Better Communication
…and the flipside of that:
The Problem With Active Listening (And How To Do It Better)
Take care!
Share This Post
Related Posts
-
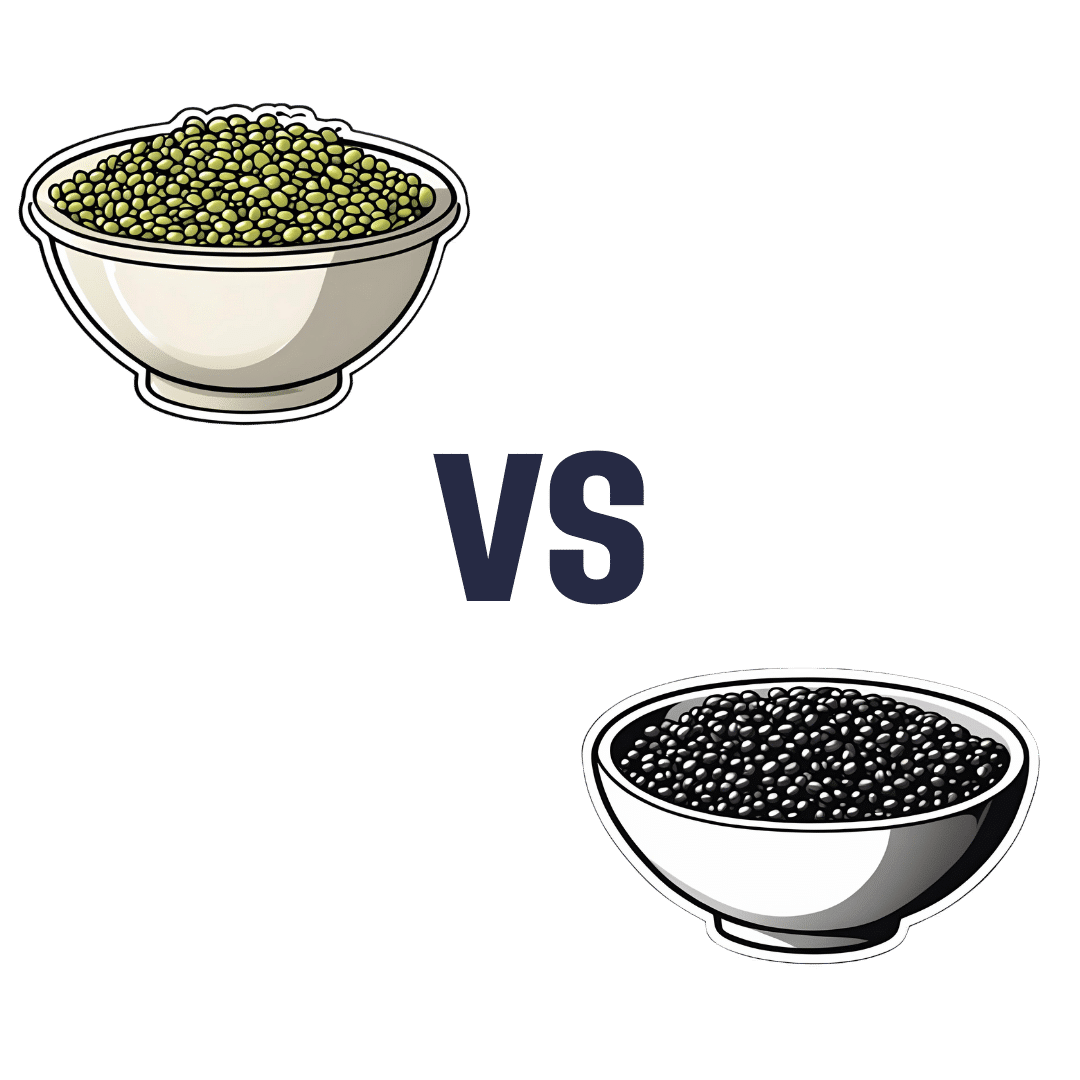
Mung Beans vs Black Gram – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing mung beans to black gram, we picked the black gram.
Why?
Both are great, and it was close!
In terms of macros, the main difference is that mung beans have slightly more fiber, while black gram has slightly more protein. So, it comes down to which we prioritize out of those two, and we’re going to call it fiber and thus hand the win in this category to mung beans—but it’s very close in either case.
In the category of vitamins, mung beans have more of vitamins B1, B6, and B9, while black gram has more of vitamins A, B2, B3, and B5. They’re equal on vitamins C, E, K, and choline. So, a marginal victory by the numbers for black gram here.
When it comes to minerals, mung beans have more copper and potassium, while black gram has more calcium, iron, magnesium, manganese, and phosphorus. They’re equal on selenium and zinc. Another win for black gram.
Adding up the sections makes for an overall win for black gram, but by all means enjoy either or both; diversity is good!
Want to learn more?
You might like to read:
What’s Your Plant Diversity Score?
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Gut Health for Women – by Aurora Bloom
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
First things first: though the title says “For Women”, almost all of it applies to men too—and the things that don’t apply, don’t cause a problem. So if you’re cooking for your family that contains one or more men, this is still great.
Bloom gives us a good, simple, practical introduction to gut health. Her overview also covers gut-related ailments beyond the obvious “tummy hurts”. On which note:
A very valuable section of this book covers dealing with any stomach-upsets that do occur… without harming your trillions of tiny friends (friendly gut microbiota). This alone can make a big difference!
The book does of course also cover the things you’d most expect: things to eat or avoid. But it goes beyond that, looking at optimizing and maintaining your gut health. It’s not just dietary advice here, because the gut affects—and is affected by—other lifestyle factors too. Ranges from mindful eating, to a synchronous sleep schedule, to what kinds of exercise are best to keep your gut ticking over nicely.
There’s also a two-week meal plan, and an extensive appendix of resources, not to mention a lengthy bibliography for sourcing health claims (and suggesting further reading).
In short, a fine and well-written guide to optimizing your gut health and enjoying the benefits.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
10 Healthiest Foods You Should Eat In The Morning
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
For many of us, our creative minds aren’t their absolute best first thing in the morning, and it’s easy to reach for what’s available, if we haven’t planned ahead.
So here’s some inspiration for the coming week! If you’re a regular coffee-and-toast person, at least consider alternating some of these with that:
- Oatmeal with fresh fruit: fiber, energy, protein, vitamins and minerals (10almonds tip: we recommend making it as overnight oats! Same nutrients, lower glycemic index)
- Greek yogurt parfait: probiotic gut benefits, along with all the goodness of fruit
- Avocado toast: so many nutrients; most famous for the healthy fats, but there’s lots more in there too!
- Egg + vegetable scramble: protein, healthy fats, vitamins and minerals, fiber
- Smoothie bowl: many nutrients—But be aware that blending will reduce fiber and make the sugar quicker to enter your bloodstream. Still not bad as an occasional feature for the sake of variety, though!
- Wholegrain pancakes: energy, fiber, and whatever your toppings! Fresh fruit is a top-tier choice; the video suggests maple syrup; we however invite you to try aged balsamic vinegar instead (sounds unlikely, we know, but try it and you’ll see; it is so delicious and your blood sugars will thank you too!)
- Chia pudding: so many nutrients in this one; chia seeds are incredible!
- Quinoa breakfast bowl: the healthy grains are a great start to the day, and contain a fair bit of protein too, and served with nuts, seeds, and diced fruit, many more nutrients get added to the mix. Unclear why the video-makers want to put honey or maple syrup on everything.
- Berries: lots of vitamins, fiber, hydration, and very many polyphenols
For a quick visual overview, and a quick-start preparation guide for the ones that aren’t just “berries” or similar, enjoy this short (3:11) video:
Click Here If The Embedded Video Doesn’t Load Automatically!
PS: They said 10, and we only counted 9. Where is the tenth one? Who would say “10 things” and then ostensibly only have 9? Who would do such a thing?!
About that chia pudding…
It’s a great way to get a healthy dose of protein, healthy fats, antioxidants, and a lot of other benefits for the heart and brain:
The Tiniest Seeds With The Most Value
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: