Complete Guide To Fasting – By Dr. Jason Fung
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When it comes to intermittent fasting, the plethora of options can be daunting at first, as can such questions as what fluids are ok to take vs what will break the fast, what to expect in terms of your first fasting experience, and how not to accidentally self-sabotage.
Practised well, intermittent fasting can be a very freeing experience, and not at all uncomfortable. Practised badly, it can be absolutely miserable, and this is one of those things where knowledge makes the difference.
Dr. Fung (yes, the same Dr. Fung we’ve featured before as an expert on metabolic health) shares this knowledge over the course of 304 pages, with lots of scientific information and insider tips. He covers the different kinds of fasting, how each of them work and what they do for the body and brain, hunger/satiety hacks, lots of “frequently asked questions”, and even a range of recipes to help smooth your journey along its way.
The style is very well-written pop-science; it’s engaging and straightforward without skimping on science at all.
Bottom line: if you’re thinking of trying intermittent fasting but aren’t sure where/how to best get started, this book can set you off on the right foot and keep you on the right track thereafter.
Click here to check out The Complete Guide to Fasting, and enjoy the process as well as the results!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Owning Your Weight – by Henri Marcoux
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A lot of diet books—which this isn’t—presuppose that the reader wants to lose weight, and varyingly encourage and shame the reader into trying to do so.
Dr. Henri Marcoux takes a completely different approach.
He starts by assuming we are—whether consciously or not—the weight we want to be, and looks at the various physical and psychological factors that influence us to such. Ranging from food poverty to eating our feelings to social factors and more, he bids us examine our relationship with food and eating—not just in the sense of mindful eating, but from multiple scientific angles too.
From this, Dr. Marcoux gives us questions and suggestions to ensure that our relationship with food and eating is what we want it to be, for us.
Much of the latter part of the book covers not just how to go about the requisite lifestyle changes… But also how to implement things in a way that sticks, and is a genuine pleasure to implement. If this sounds over-the-top, the truth is that it’s just because it honestly is a lower-stress way of living.
Bottom line: if you want to gain or lose weight, there’s a good chance this book will help you. If you want to be happier and healthier at the weight you are, there’s a good chance this book will help you with that, too.
Click here to check out Owning Your Weight, and take control of yours!
Share This Post
-
How To Make Drinking Less Harmful
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Making Drinking Less Harmful
We often talk of the many ways alcohol harms our health, and we advocate for reducing (or eliminating) its consumption. However, it’s not necessarily as easy as all that, and it might not even be a goal that everyone has. So, if you’re going to imbibe, what can you do to mitigate the harmful effects of alcohol?
There is no magical solution
Sadly. If you drink alcohol, there will be some harmful effects, and nothing will completely undo that. But there are some things that can at least help—read on to learn more!
Coffee
It’s not the magical sober-upperer that some would like it to be, but it is good against the symptoms of alcohol intoxication, and slightly reduces the harm to your body, because it is:
- Hydrating (whereas alcohol is dehydrating)
- A source of antioxidants (whereas alcohol causes oxidative stress, which has nothing to do with psychological stress, and is a kind of cellular damage)
- A stimulant, assuming it is not decaffeinated (it’s worth noting that its stimulant effects work partly by triggering vasoconstriction, which is the opposite of the vasodilation caused by alcohol)
To this end, the best coffee for anti-alcohol effects should be:
- Caffeinated, and strong
- Long (we love espresso, but we need hydration here and that comes from volume!)
- Without sugar (you don’t want to create an adverse osmotic gradient to leech water from your body)
As for milk/cream/whatever, have it or don’t, per your usual preference. It won’t make any difference to the alcohol in your system.
Antioxidants, polyphenols, flavonoids, and things with similar mechanisms
We mentioned that coffee contains antioxidants, but if you want to really bring out the heavy guns, taking more powerful antioxidants can help a lot. If you don’t have the luxury of enjoying berries and cacao nibs by the handful, supplements that have some similar benefits are a perfectly respectable choice.
For example, you might want to consider green tea extract:
L-theanine 200mg (available on Amazon)
Specialist anti-alcohol drugs
These are somewhat new and the research is still ongoing, but for example:
Dihydromyricetin (DHM) as a novel anti-alcohol intoxication medication
In short, DHM is a flavonoid (protects against the oxidative stress caused by alcohol, and has been found to reduce liver damage—see the above link) and also works on GABA-receptors (reduces alcohol withdrawal symptoms after cessation of drinking, and thus also reduces hangovers).
Once again: the marketing claims of such drugs may be bold, but there’s a lot that’s not known and they’re not a magic pill. They do NOT mean you can take them alongside drinking and drink what you like with impunity. However, they may help mitigate some of the harmful effects of alcohol. If you wish to try them, these can be purchased at pharmacies or online, for example:
Alcohol Defense Capsules (available on Amazon)
Bottom line
Alcohol is bad for your health and none of the above will eliminate the health risks. But, if you’re going to have alcohol, then having the above things as well may at least somewhat reduce the harm done.
Share This Post
-
World Menopause Day Health News Round-Up
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In order to provide variety in this week’s round-up, not all of this is menopause-related, but it is all important:
Menopause & CVD
Untreated menopause is associated with higher incidence of heart disease, and higher mortality. People often forget about how much estrogen does for us (well, for those of us with a physiology running on estrogen, anyway; gentlemen, your testosterone is fine for you), and think it is “just” a sex hormone, but it’s a lot more.
Read in full: Menopause transition linked to increased heart disease risk
Related: What Menopause Does To The Heart
Extraterrestrial medical technology
The much lower gravity in Earth orbit has allowed for tissue engineering techniques that Earth’s normal gravity imposes limitations on. This is big news, because it means that rather than replacing a whole liver, tissue implants could be grafted, allowing the extant liver to repair itself (something livers are famously good at, but they need enough undamaged base material to work with).
Read in full: How liver tissue from the International Space Station may transform tissue engineering
Related: How To Unfatty A Fatty Liver
One thing and then another
As if endometriosis weren’t unpleasant enough in and of itself, the endothelial dysfunction inherent to it also raises cardiovascular disease risk. This is important, because while endometriosis has (like many maladies predominantly affecting women) generally been shrugged off by the medical world as an unhappy inconvenience but not life-threatening, now we know it comes with extra existential risks too:
Read in full: Understanding cardiovascular risks in endometriosis patients
Related: What You Need To Know About Endometriosis
Push-button meditation
Unlike mindfulness meditation, listening to music is a very passive experience, and thus requires less effort from the user. And yet, it has been associated with lower perceived pain levels, lower self-reported anxiety levels, less opioid use, and measurably lower heart-rate.
Read in full: Listening to music may speed up recovery from surgery, research suggests
Related: Nobody Likes Surgery, But Here’s How To Make It Much Less Bad
Cholesterol in menopause: quality over quantity
Much like previous research has shown that the quantity of LDL is not nearly so predictive of health outcomes in women as it is in men, this study into HDL and menopausal women shows that quantity of HDL does not matter nearly so much as the quality of it.
Read in full: HDL quality, not quantity, contribute to the first sign of Alzheimer’s disease in women
Related: Statins: His & Hers? ← consistent with the above, statins (to lower LDL cholesterol) generally help more for men and produce more adverse side effects for women. So again, a case of “the actual amount of cholesterol isn’t so important for women as for men”.
Take care!
Share This Post
Related Posts
-
Yes, blue light from your phone can harm your skin. A dermatologist explains
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Social media is full of claims that everyday habits can harm your skin. It’s also full of recommendations or advertisements for products that can protect you.
Now social media has blue light from our devices in its sights.
So can scrolling on our phones really damage your skin? And will applying creams or lotions help?
Here’s what the evidence says and what we should really be focusing on.
Max kegfire/Shutterstock Remind me, what actually is blue light?
Blue light is part of the visible light spectrum. Sunlight is the strongest source. But our electronic devices – such as our phones, laptops and TVs – also emit it, albeit at levels 100-1,000 times lower.
Seeing as we spend so much time using these devices, there has been some concern about the impact of blue light on our health, including on our eyes and sleep.
Now, we’re learning more about the impact of blue light on our skin.
How does blue light affect the skin?
The evidence for blue light’s impact on skin is still emerging. But there are some interesting findings.
1. Blue light can increase pigmentation
Studies suggest exposure to blue light can stimulate production of melanin, the natural skin pigment that gives skin its colour.
So too much blue light can potentially worsen hyperpigmentation – overproduction of melanin leading to dark spots on the skin – especially in people with darker skin.
Blue light can worsen dark spots on the skin caused by overproduction of melanin. DUANGJAN J/Shutterstock 2. Blue light can give you wrinkles
Some research suggests blue light might damage collagen, a protein essential for skin structure, potentially accelerating the formation of wrinkles.
A laboratory study suggests this can happen if you hold your device one centimetre from your skin for as little as an hour.
However, for most people, if you hold your device more than 10cm away from your skin, that would reduce your exposure 100-fold. So this is much less likely to be significant.
3. Blue light can disrupt your sleep, affecting your skin
If the skin around your eyes looks dull or puffy, it’s easy to blame this directly on blue light. But as we know blue light affects sleep, what you’re probably seeing are some of the visible signs of sleep deprivation.
We know blue light is particularly good at suppressing production of melatonin. This natural hormone normally signals to our bodies when it’s time for sleep and helps regulate our sleep-wake cycle.
By suppressing melatonin, blue light exposure before bed disrupts this natural process, making it harder to fall asleep and potentially reducing the quality of your sleep.
The stimulating nature of screen content further disrupts sleep. Social media feeds, news articles, video games, or even work emails can keep our brains active and alert, hindering the transition into a sleep state.
Long-term sleep problems can also worsen existing skin conditions, such as acne, eczema and rosacea.
Sleep deprivation can elevate cortisol levels, a stress hormone that breaks down collagen, the protein responsible for skin’s firmness. Lack of sleep can also weaken the skin’s natural barrier, making it more susceptible to environmental damage and dryness.
Can skincare protect me?
The beauty industry has capitalised on concerns about blue light and offers a range of protective products such as mists, serums and lip glosses.
From a practical perspective, probably only those with the more troublesome hyperpigmentation known as melasma need to be concerned about blue light from devices.
This condition requires the skin to be well protected from all visible light at all times. The only products that are totally effective are those that block all light, namely mineral-based suncreens or some cosmetics. If you can’t see the skin through them they are going to be effective.
But there is a lack of rigorous testing for non-opaque products outside laboratories. This makes it difficult to assess if they work and if it’s worth adding them to your skincare routine.
What can I do to minimise blue light then?
Here are some simple steps you can take to minimise your exposure to blue light, especially at night when it can disrupt your sleep:
- use the “night mode” setting on your device or use a blue-light filter app to reduce your exposure to blue light in the evening
- minimise screen time before bed and create a relaxing bedtime routine to avoid the types of sleep disturbances that can affect the health of your skin
- hold your phone or device away from your skin to minimise exposure to blue light
- use sunscreen. Mineral and physical sunscreens containing titanium dioxide and iron oxides offer broad protection, including from blue light.
In a nutshell
Blue light exposure has been linked with some skin concerns, particularly pigmentation for people with darker skin. However, research is ongoing.
While skincare to protect against blue light shows promise, more testing is needed to determine if it works.
For now, prioritise good sun protection with a broad-spectrum sunscreen, which not only protects against UV, but also light.
Michael Freeman, Associate Professor of Dermatology, Bond University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
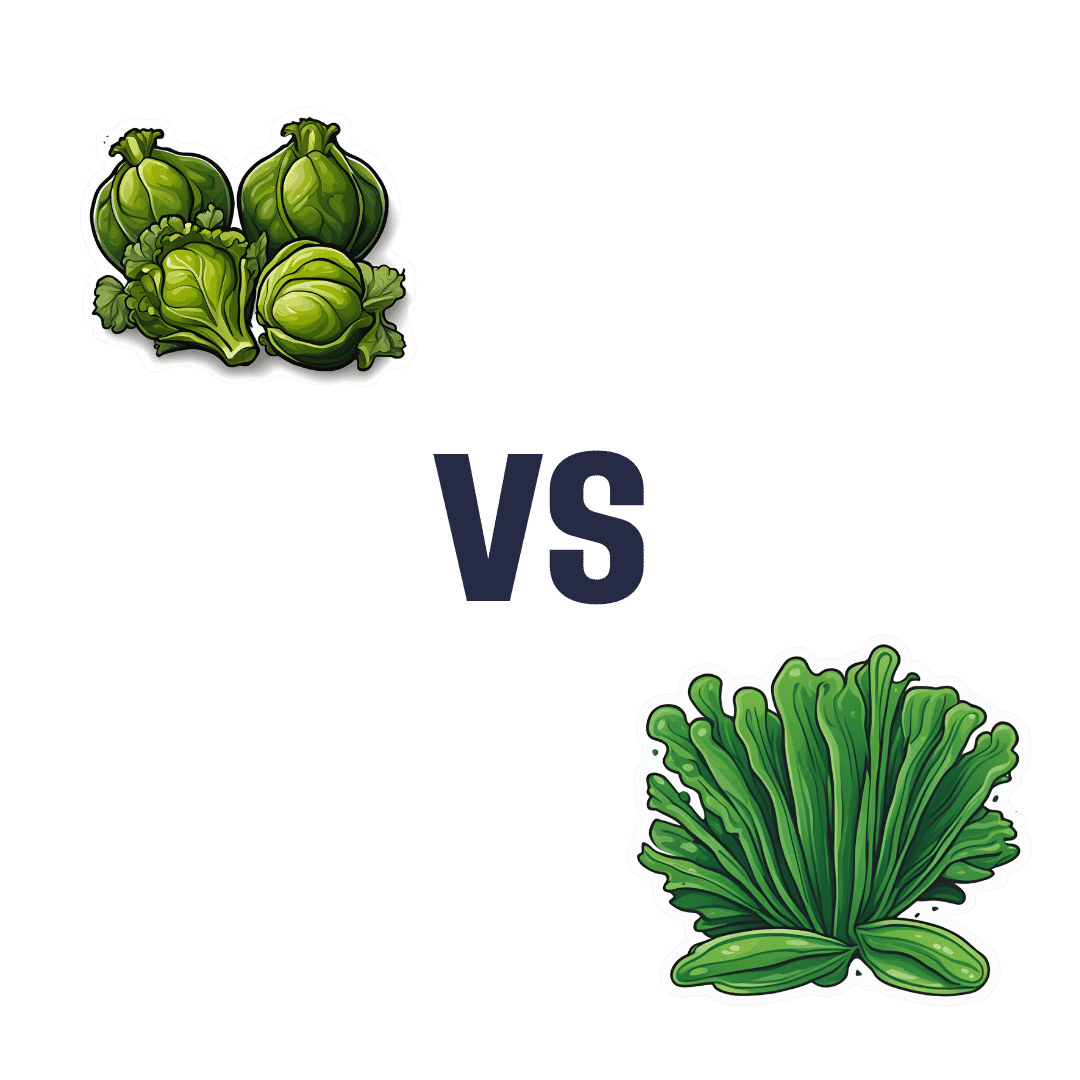
Brussels Sprouts vs Spirulina – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing Brussels sprouts to spirulina, we picked the sprouts.
Why?
Pitting these two well-known superfoods against each other, we get the following:
Looking at the macros first, spirulina has a little more protein, while sprouts have more carbs and nearly 10x the fiber. So, we call this a win for sprouts.
In terms of vitamins, sprouts have a lot more of vitamins A, B6, B9, C, E, K, and choline, while spirulina has a little more of vitamins B1, B2, and B3. An easy win for sprouts.
In the category of minerals, sprouts have more calcium, magnesium, manganese, phosphorus, potassium, selenium, and zinc, while spirulina has more copper and iron. Another clear win for sprouts.
Adding up the sections makes the winner very clear: Brussels sprouts enjoy a well-earned victory.
Want to learn more?
You might like to read:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Doctors Are as Vulnerable to Addiction as Anyone. California Grapples With a Response
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
BEVERLY HILLS, Calif. — Ariella Morrow, an internal medicine doctor, gradually slid from healthy self-esteem and professional success into the depths of depression.
Beginning in 2015, she suffered a string of personal troubles, including a shattering family trauma, marital strife, and a major professional setback. At first, sheer grit and determination kept her going, but eventually she was unable to keep her troubles at bay and took refuge in heavy drinking. By late 2020, Morrow could barely get out of bed and didn’t shower or brush her teeth for weeks on end. She was up to two bottles of wine a day, alternating it with Scotch whisky.
Sitting in her well-appointed home on a recent autumn afternoon, adorned in a bright lavender dress, matching lipstick, and a large pearl necklace, Morrow traced the arc of her surrender to alcohol: “I’m not going to drink before 5 p.m. I’m not going to drink before 2. I’m not going to drink while the kids are home. And then, it was 10 o’clock, 9 o’clock, wake up and drink.”
As addiction and overdose deaths command headlines across the nation, the Medical Board of California, which licenses MDs, is developing a new program to treat and monitor doctors with alcohol and drug problems. But a fault line has appeared over whether those who join the new program without being ordered to by the board should be subject to public disclosure.
Patient advocates note that the medical board’s primary mission is “to protect healthcare consumers and prevent harm,” which they say trumps physician privacy.
The names of those required by the board to undergo treatment and monitoring under a disciplinary order are already made public. But addiction medicine professionals say that if the state wants troubled doctors to come forward without a board order, confidentiality is crucial.
Public disclosure would be “a powerful disincentive for anybody to get help” and would impede early intervention, which is key to avoiding impairment on the job that could harm patients, said Scott Hambleton, president of the Federation of State Physician Health Programs, whose core members help arrange care and monitoring of doctors for substance use disorders and mental health conditions as an alternative to discipline.
But consumer advocates argue that patients have a right to know if their doctor has an addiction. “Doctors are supposed to talk to their patients about all the risks and benefits of any treatment or procedure, yet the risk of an addicted doctor is expected to remain a secret?” Marian Hollingsworth, a volunteer advocate with the Patient Safety Action Network, told the medical board at a Nov. 14 hearing on the new program.
Doctors are as vulnerable to addiction as anyone else. People who work to help rehabilitate physicians say the rate of substance use disorders among them is at least as high as the rate for the general public, which the federal Substance Abuse and Mental Health Services Administration put at 17.3% in a Nov. 13 report.
Alcohol is a very common drug of choice among doctors, but their ready access to pain meds is also a particular risk.
“If you have an opioid use disorder and are working in an operating room with medications like fentanyl staring you down, it’s a challenge and can be a trigger,” said Chwen-Yuen Angie Chen, an addiction medicine doctor who chairs the Well-Being of Physicians and Physicians-in-Training Committee at Stanford Health Care. “It’s like someone with an alcohol use disorder working at a bar.”
From Pioneer to Lagger
California was once at the forefront of physician treatment and monitoring. In 1981, the medical board launched a program for the evaluation, treatment, and monitoring of physicians with mental illness or substance use problems. Participants were often required to take random drug tests, attend multiple group meetings a week, submit to work-site surveillance by colleagues, and stay in the program for at least five years. Doctors who voluntarily entered the program generally enjoyed confidentiality, but those ordered into it by the board as part of a disciplinary action were on the public record.
The program was terminated in 2008 after several audits found serious flaws. One such audit, conducted by Julianne D’Angelo Fellmeth, a consumer interest lawyer who was chosen as an outside monitor for the board, found that doctors in the program were often able to evade the random drug tests, attendance at mandatory group therapy sessions was not accurately tracked, and participants were not properly monitored at work sites.
Today, MDs who want help with addiction can seek private treatment on their own or in many cases are referred by hospitals and other health care employers to third parties that organize treatment and surveillance. The medical board can order a doctor on probation to get treatment.
In contrast, the California licensing boards of eight other health-related professions, including osteopathic physicians, registered nurses, dentists, and pharmacists, have treatment and monitoring programs administered under one master contract by a publicly traded company called Maximus Inc. California paid Maximus about $1.6 million last fiscal year to administer those programs.
When and if the final medical board regulations are adopted, the next step would be for the board to open bidding to find a program administrator.
Fall From Grace
Morrow’s troubles started long after the original California program had been shut down.
The daughter of a prominent cosmetic surgeon, Morrow grew up in Palm Springs in circumstances she describes as “beyond privileged.” Her father, David Morrow, later became her most trusted mentor.
But her charmed life began to fall apart in 2015, when her father and mother, Linda Morrow, were indicted on federal insurance fraud charges in a well-publicized case. In 2017, the couple fled to Israel in an attempt to escape criminal prosecution, but later they were both arrested and returned to the United States to face prison sentences.
The legal woes of Morrow’s parents, later compounded by marital problems related to the failure of her husband’s business, took a heavy toll on Morrow. She was in her early 30s when the trouble with her parents started, and she was working 16-hour days to build a private medical practice, with two small children at home. By the end of 2019, she was severely depressed and turning increasingly to alcohol. Then, the loss of her admitting privileges at a large Los Angeles hospital due to inadequate medical record-keeping shattered what remained of her self-confidence.
Morrow, reflecting on her experience, said the very strengths that propel doctors through medical school and keep them going in their careers can foster a sense of denial. “We are so strong that our strength is our greatest threat. Our power is our powerlessness,” she said. Morrow ignored all the flashing yellow lights and even the red light beyond which serious trouble lay: “I blew through all of it, and I fell off the cliff.”
By late 2020, no longer working, bedridden by depression, and drinking to excess, she realized she could no longer will her way through: “I finally said to my husband, ‘I need help.’ He said, ‘I know you do.’”
Ultimately, she packed herself off to a private residential treatment center in Texas. Now sober for 21 months, Morrow said the privacy of the addiction treatment she chose was invaluable because it shielded her from professional scrutiny.
“I didn’t have to feel naked and judged,” she said.
Morrow said her privacy concerns would make her reluctant to join a state program like the one being considered by the medical board.
Physician Privacy vs. Patient Protection
The proposed regulations would spare doctors in the program who were not under board discipline from public disclosure as long as they stayed sober and complied with all the requirements, generally including random drug tests, attendance at group sessions, and work-site monitoring. If the program put a restriction on a doctor’s medical license, it would be posted on the medical board’s website, but without mentioning the doctor’s participation in the program.
Yet even that might compromise a doctor’s career since “having a restricted license for unspecified reasons could have many enduring personal and professional implications, none positive,” said Tracy Zemansky, a clinical psychologist and president of the Southern California division of Pacific Assistance Group, which provides support and monitoring for physicians.
Zemansky and others say doctors, just like anyone else, are entitled to medical privacy under federal law, as long as they haven’t caused harm.
Many who work in addiction medicine also criticized the proposed new program for not including mental health problems, which often go hand in hand with addiction and are covered by physician health programs in other states.
“To forgo mental health treatment, I think, is a grave mistake,” Morrow said. For her, depression and alcoholism were inseparable, and the residential program she attended treated her for both.
Another point of contention is money. Under the current proposal, doctors would bear all the costs of the program.
The initial clinical evaluation, plus the regular random drug tests, group sessions, and monitoring at their work sites could cost participants over $27,000 a year on average, according to estimates posted by the medical board. And if they were required to go for 30-day inpatient treatment, that would add an additional $40,000 — plus nearly $36,000 in lost wages.
People who work in the field of addiction medicine believe that is an unfair burden. They note that most programs for physicians in other states have outside funding to reduce the cost to participants.
“The cost should not be fully borne by the doctors, because there are many other people that are benefiting from this, including the board, malpractice insurers, hospitals, the medical association,” said Greg Skipper, a semi-retired addiction medicine doctor who ran Alabama’s state physician health program for 12 years. In Alabama, he said, those institutions contribute to the program, significantly cutting the amount doctors have to pay.
The treatment program that Morrow attended in spring of 2021, at The Menninger Clinic in Houston, cost $80,000 for a six-week stay, which was covered by a concerned family member. “It saved my life,” she said.
Though Morrow had difficulty maintaining her sobriety in the first year after treatment, she has now been sober since April 2, 2022. These days, Morrow regularly attends therapy and Alcoholics Anonymous and has pivoted to become an addiction medicine doctor.
“I am a better doctor today because of my experience — no question,” Morrow said. “I am proud to be a doctor who’s an alcoholic in recovery.”
This article was produced by KFF Health News, which publishes California Healthline, an editorially independent service of the California Health Care Foundation.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: