The Art of Being Unflappable (Tricks For Daily Life)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Art of Being Unflappable
From Stoicism to CBT, thinkers through the ages have sought the unflappable life.
Today, in true 10almonds fashion, we’re going to distil it down to some concentrated essentials that we can all apply in our daily lives:
Most Common/Impactful Cognitive Distortions To Catch (And Thus Avoid)
These are like the rhetorical fallacies with which you might be familiar (ad hominem, no true Scotsman, begging the question, tu quoque, straw man, etc), but are about what goes on between your own ears, pertaining to your own life.
If we learn about them and how to recognize them, however, we can catch them before they sabotage us, and remain “unflappable” in situations that could otherwise turn disastrous.
Let’s take a look at a few:
Catastrophizing / Crystal Ball
- Distortion: not just blowing something out of proportion, but taking an idea and running with it to its worst possible conclusion. For example, we cook one meal that’s a “miss” and conclude we are a terrible cook, and in fact for this reason a terrible housewife/mother/friend/etc, and for this reason everyone will probably abandon us and would be right to do so
- Reality: by tomorrow, you’ll probably be the only one who even remembers it happened
Mind Reading
- Distortion: attributing motivations that may or may not be there, and making assumptions about other people’s thoughts/feelings. An example is the joke about two partners’ diary entries; one is long and full of feelings about how the other is surely dissatisfied in their marriage, has been acting “off” with them all day, is closed and distant, probably wants to divorce, may be having an affair and is wondering which way to jump, and/or is just wondering how to break the news—the other partner’s diary entry is short, and reads “motorcycle won’t start; can’t figure out why”
- Reality: sometimes, asking open questions is better than guessing, and much better than assuming!
All-or-Nothing Thinking / Disqualifying the Positive / Magnifying the Negative
- Distortion: having a negative bias that not only finds a cloud in every silver lining, but stretches it out so that it’s all that we can see. In a relationship, this might mean that one argument makes us feel like our relationship is nothing but strife. In life in general, it may lead us to feel like we are “naturally unlucky”.
- Reality: those negative things wouldn’t even register as negative to us if there weren’t a commensurate positive we’ve experienced to hold them in contrast against. So, find and remember that positive too.
For brevity, we put a spotlight on (and in some cases, clumped together) the ones we think have the most bang-for-buck to know about, but there are many more.
So for the curious, here’s some further reading:
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
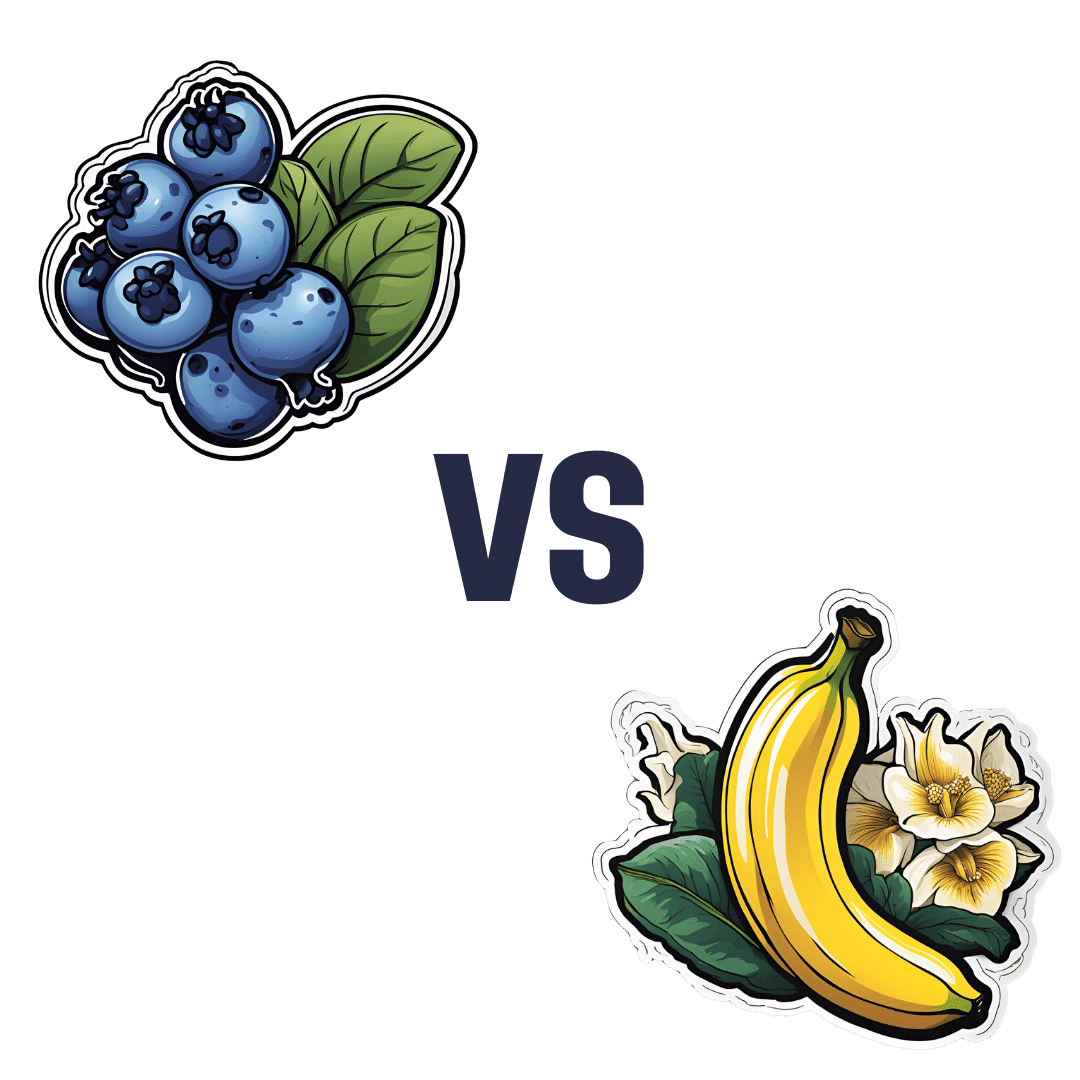
Blueberries vs Banana – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing blueberries to banana, we picked the banana.
Why?
Surprise, that which is more expensive is not always commensurately more healthy! A lot of the price difference between bananas and blueberries comes down to:
- ease of transport (unripe bananas can be transported quite easily without too much risk of bruising; unripe blueberries can’t even be usefully picked)
- shelf-life (unripe bananas will take their time to ripen; the already-ripe blueberries will often go bad very quickly)
For this reason, frozen blueberries are a great option for budget-friendly berries. But, onto the comparisons:
In terms of macros, bananas have slightly more protein, carbs, and fiber, and the slightly lower glycemic index. Really, both are good, but by the numbers, bananas win.
When it comes to vitamins, blueberries have more of vitamins B1, C, E, and K, while bananas have more of vitamins A, B2, B3, B5, B6, B9, and choline. Another win for bananas, though of course we could quibble which vitamins are most likely to be not found in sufficient abundance in the rest of one’s diet, but as it is, we just compared the nutrients head-to-head without trying to guess the rest of someone’s diet.
In the category of minerals, blueberries have more calcium and manganese, while bananas have more copper, magnesium, phosphorus, potassium, and selenium. Another win for bananas.
As for polyphenols, this is where blueberries shine, with a lot more than bananas (difficult to calculate exactly due to variations, but, in the order of hundreds of times more). A win for blueberries this time.
Adding up the section gives us an overall win for bananas, but by all means enjoy either or both; perhaps even together!
Want to learn more?
You might like to read:
Blueberry & Banana Collagen Baked Oats ← You will love this recipe! And… Good news for vegans/vegetarians: while we include an optional tablespoon of collagen powder in this recipe, the whole recipe is already geared around collagen synthesis, so it’s very collagen-boosting even with just the plants, providing collagen’s building blocks of protein, zinc, and vitamins C and D (your miraculous body will use these to assemble the collagen inside you).
Enjoy!
Share This Post
-
Cranberries vs Goji Berries – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing cranberries to goji berries, we picked the cranberries.
Why?
Both are great! And your priorities may differ. Here’s how they stack up:
In terms of macros, goji berries have more protein, carbs, and fiber. This is consistent with them generally being eaten very dried, whereas cranberries are more often eaten fresh or from frozen, or partially rehydrated. In any case, goji berries are the “more food per food” option, so it wins this category. The glycemic indices are both low, by the way, though goji berries are the lower.
When it comes to vitamins, cranberries have more of vitamins B1, B2, B3, B5, B6, B9, E, K, and choline, while goji berries have more of vitamins A and C. Admittedly it’s a lot more, but still, on strength of overall vitamin coverage, the clear winner here is cranberries.
We see a similar story when it comes to minerals: cranberries have more copper, magnesium, manganese, phosphorus, potassium, selenium, and zinc, while goji berries have (a lot) more calcium and iron. Again, by strength of overall mineral coverage, the clear winner here is cranberries.
Cranberries do also have some extra phytochemical benefits, including their prevention/cure status when it comes to UTIs—see our link below for more on that.
At any rate, enjoy either or both, but those are the strengths and weaknesses of these two berries!
Want to learn more?
You might like to read:
- Health Benefits Of Cranberries (But: You’d Better Watch Out)
- Goji Berries: Which Benefits Do They Really Have?
- The Sugary Food That Lowers Blood Sugars ← this is also about goji berries
Take care!
Share This Post
-
The Exercises That Help Keep Breast Cancer At Bay
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
For women, our lifetime risk of being diagnosed with breast cancer is about 1 in 7, before we take into account any added risk or protective factors.
For men, it’s more like 1 in 556, which again, is before taking into account any added risk or protective factors.
Here’s a good place to start on improving those odds: How To Triple Your Breast Cancer Survival Chances
And for that matter, check out: 8 Signs On Your Breast You Shouldn’t Ignore
And for those concerned (or even just curious) about the pros and cons of menopausal HRT when it comes to breast cancer:
The Hormone Therapy That Reduces Breast Cancer Risk & More ← this is actually very important to understand, as otherwise it’s easy to accidentally self-sabotage and increase one’s overall mortality risk
So, what’s this about exercise and breast cancer?
There are two things to focus on
No, not those.
Well, yes, those, but also: aerobic exercise and resistance training.
A research team (Dr. Alice Avancini et al.) analysed data from 22 randomized controlled trials (total n=968 participants) that investigated the effects of exercise on various pro-inflammatory biomarkers (mostly interleukin variants, but also c-reactive proteins) that are known to increase breast cancer reoccurrence risk.
What they found was:
❝Exercise induced small to large significant reductions in IL-6 (SMD = -0.85; 95% CI = -1.68 to -0.02; p = .05) and TNF-α (SMD = -0.40; 95% CI = -0.81 to 0.01; p = .05) and a trend for a decrease in CRP.
When stratifying by exercise mode, trends toward reduction in IL-6 and TNF-α were observed for combined exercise, whilst changes were not generally affected by exercise program duration❞
The “combined exercise” mentioned?
Aerobic exercise and resistance training.
This is important, because as regular 10almonds readers may remember…
What Your Metabolism Says About How Aggressive Breast Cancer Is Likely To Be For You ← this makes a huge difference to survival chances
So, this study’s findings are very consistent with that, because:
- Aerobic training increases cardiovascular fitness, improving metabolism
- Resistance training increases muscle mass, improving metabolism*
*because muscle “costs” calories to maintain, prompting an increase in metabolism, whereas fat prompts our metabolism to slow, to conserve energy to face the obvious food shortage that must be coming
See also: Stop Cancer 20 Years Ago
Want to learn more?
Here’s the best book we’ve read on breast cancer survival:
The Smart Woman’s Guide to Breast Cancer – by Dr. Jenn Simmons
Take care!
Share This Post
Related Posts
-
Eat Better, Feel Better – by Giada de Laurentis
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In yesterday’s edition of 10almonds, we reviewed Dr. Aujla’s “The Doctor’s Kitchen“; today we’re reviewing a different book about healing through food—in this case, with a special focus on maintaining energy and good health as we get older.
De Laurentis may not be a medical doctor, but she is a TV chef, and not only holds a lot of influence, but also has access to a lot of celebrity doctors and such; that’s reflected a lot in her style and approach here.
The recipes are clear and easy to follow; well-illustrated and nicely laid-out.
This cookbook’s style is less “enjoy this hearty dish of rice and beans with these herbs and spices” and more “you can serve your steak salad with white beans and sweet shallot dressing on a bed of organic quinoa if you haven’t already had your day’s serving of grains, of course”.
It’s a little fancier, in short, and more focused on what to cut out, than what to include. On account of that, this could make it a good contrast to yesterday’s book, which had the opposite focus.
She also recommends assorted adjuvant practices; some that are evidence-based, like intermittent fasting and meditation, and some that are not, like extreme detox-dieting, and acupuncture (which has no bearing on gut health).
Bottom line: if you like the idea of eating for good health, and prefer a touch of celebrity lifestyle to your meals, this one’s a good book for you.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Dentists Debunk 15 Teeth Myths
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dentists Dr. John Yoo and Dr. Jason Lin leave no gaps in the truth:
The tooth, the whole tooth, and nothing but the tooth
Not only is there no tooth fairy (we are shocked), but also…
- “Baby teeth aren’t important.”
False! Baby teeth act as space holders for permanent teeth, affect speech development, and influence a child’s psychological well-being. - “Acidic fruits will whiten your smile.”
False! In any practical sense, anyway: acidic fruits may temporarily make teeth appear whiter by dispersing stains but cause enamel erosion and weaken teeth over time. - “Fillings last forever.”
False! Fillings can wear down, fail, or develop cavities underneath if oral hygiene isn’t maintained, requiring replacement over time. - “Cavities are irreversible.”
False! Cavities in the enamel can be reversed with fluoride and good oral hygiene, but cavities that reach the dentin are typically irreversible. - “Braces are just for crooked teeth.”
False! Braces also correct functional issues like overbites, underbites, crossbites, and prevent future complications like tooth impaction. - “A knocked-out tooth is gone for good.”
False! A knocked-out tooth can be reimplanted if done quickly (ideally within an hour); storing it in whole milk or saliva helps preserve it. - “Diet sodas won’t give you cavities.”
False! Diet sodas can still cause cavities due to their acidic pH, which erodes enamel, even without sugar. - “Dental cleanings aren’t necessary.”
False! Dental cleanings help remove plaque and tartar that regular brushing can’t, and allow for regular oral health checkups. - “Retainers aren’t for life.”
False! To maintain teeth alignment after braces, retainers should be worn long-term as teeth can shift even years later. - “You should floss before brushing.”
False! The order doesn’t matter, but do floss regularly. - “Everyone has wisdom teeth.”
False! Not everyone is born with wisdom teeth; they are the most commonly missing teeth, and not everyone needs them removed. - “Hydrogen peroxide and baking soda are good toothpaste replacements.”
False! While they are common components in toothpaste, they lack fluoride, which is essential for remineralizing and protecting enamel. - “You’re too old to get braces.”
False! There’s no age limit for braces or aligners; adults often seek them for both aesthetic and functional reasons. - “Teeth that have had root canals can’t feel.”
False! Teeth with root canals can’t feel pain from nerves, but you can still sense pressure due to surrounding ligaments. - “You’ll inevitably lose all your teeth when you’re old.”
False! Good oral hygiene and regular dental care can preserve natural teeth into old age, though genetics also play a role.
For more on each of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
- “Baby teeth aren’t important.”
-
Longevity for the Lazy – by Dr. Richard Malish
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
There are some people who devote all their resources to longevity, which can become a full-time occupation, not to mention a very expensive endeavor. This book’s for those who want to get the best possible “bang for buck” by doing the things that have the most favorable cost:worth ratio.
Dr. Malish covers what can be done easily for personal longevity, as well as what technological advances can be enjoyed that those before us didn’t have as options. He also discusses the diseases that are most likely to kill us, and how to avoid those.
He preaches a proactive approach, but one that is simple and consistent and based in good science, and good statistics. Indeed, while he’s served 20 years as an army doctor and a cardiologist, he now works as a healthcare policy consultant, so he is well-placed to advise.
The style of the book is halfway between regular pop-science and a textbook; you can either read it cover-to-cover, or skim first though the key points, highlight boxes, summaries, and the like. He also provides a time-phased task list, for those who like things to be laid out like that.
Bottom line: this is a very good, methodical guide to living longer without making it a full-time occupation.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: