Stop Pain Spreading
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Put Your Back Into It (Or Don’t)!
We’ve written before about Managing Chronic Pain (Realistically!), and today we’re going to tackle a particular aspect of chronic pain management.
- It’s a thing where the advice is going to be “don’t do this”
- And if you have chronic pain, you will probably respond “yep, I do that”
However, it’s definitely a case of “when knowing isn’t the problem”, or at the very least, it’s not the whole problem.
Stop overcompensating and address the thing directly
We all do it, whether in chronic pain, or just a transient injury. But we all need to do less of it, because it causes a lot of harm.
Example: you have pain in your right knee, so you sit, stand, walk slightly differently to try to ease that pain. It works, albeit marginally, at least for a while, but now you also have pain in your left hip and your lumbar vertebrae, because of how you leaned a certain way. You adjust how you sit, stand, walk, to try to ease both sets of pain, and before you know it, now your neck also hurts, you have a headache, and you’re sure your digestion isn’t doing what it should and you feel dizzy when you stand. The process continues, and before long, what started off as a pain in one knee has now turned your whole body into a twisted aching wreck.
What has happened: the overcompensation due to the original pain has unduly stressed a connected part of the body, which we then overcompensate for somewhere else, bringing down the whole body like a set of dominoes.
For more on this: Understanding How Pain Can Spread
“Ok, but how? I can’t walk normally on that knee!”
We’re keeping the knee as an example here, but please bear in mind it could be any chronic pain and resultant disability.
Note: if you found the word “disability” offputting, please remember: if it adversely affects your abilities, it is a disability. Disabilities are not something that only happen to other people! They will happen to most of us at some point!
Ask yourself: what can you do, and what can’t you do?
For example:
- maybe you can walk, but not normally
- maybe you can walk normally, but not without great pain
- maybe you can walk normally, but not at your usual walking pace
First challenge: accept your limitations. If you can’t walk at your usual walking pace without great pain and/or throwing your posture to the dogs, then walk more slowly. To Hell with societal expectations that it shouldn’t take so long to walk from A to B. Take the time you need.
Second challenge: accept help. It doesn’t have to be help from another person (although it could be). It might be accepting the help of a cane, or maybe even a wheelchair for “flare-up” days. Society, especially American society which is built on ideas of self-sufficiency, has framed a lot of such options as “giving up”, but if they help you get about your day while minimizing doing further harm to your body, then they can be good and even health-preserving things. Same goes for painkillers if they help you from doing more harm to your body by balling up tension in a part of your body in a way that ends up spreading out and laying ruin to your whole body.
Speaking of which:
How Much Does It Hurt? Get The Right Help For Your Pain
After which, you might want to check out:
The 7 Approaches To Pain Management
and
Science-Based Alternative Pain Relief
Third challenge: deserves its own section, so…
Do what you can
If you have chronic pain (or any chronic illness, really), you are probably fed up of hearing how this latest diet will fix you, or yoga will fix you, and so on. But, while these things may not be miracle cures…
- A generally better diet really will lessen symptoms and avoid flare-ups (a low-inflammation diet is a great start for lessening the symptoms of a lot of chronic illnesses)
- Doing what exercise you can, being mindful of your limitations yes but still keeping moving as much as possible, will also prevent (or at least slow) deterioration. Consider consulting a physiotherapist for guidance (a doctor will more likely just say “rest, take it easy”, whereas a physiotherapist will be able to give more practical advice).
- Getting good sleep may be a nightmare in the case of chronic pain (or other chronic illnesses! Here’s to those late night hyperglycemia incidents for Type 1 Diabetics that then need monitoring for the next few hours while taking insulin and hoping it goes back down) but whatever you can do to prioritize it, do it.
Want to read more?
We reviewed a little while ago a great book about this; the title sounds like a lot of woo, but we promise the content is extremely well-referenced science:
…and if your issue is back pain specifically, we highly recommend:
Healing Back Pain: The Mind-Body Connection – by Dr. John Sarno
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
F*ck You Chaos – by Dominika Choroszko
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve all read decluttering books. Some may even have decluttering books cluttering bookshelves. This one’s a little different, though:
Dominika Choroszko looks at assessing, decluttering, and subsequently organizing:
- Your home
- Your mind
- Your finances
In other words
- she starts off like Marie Kondo, and…
- phases through doing the jobs of Queer Eye’s “Fab Five”, before…
- sitting us down with some CBT worksheets, and…
- finally going through finances à la Martin Lewis.
By the time we’ve read the book, it’s as though Mary Poppins has breezed through our house, head, and bank account, leaving everything “practically perfect in every way”.
Of course, it’s on us to actually do the work, but as many of us struggle with “how” and the ever-dreaded “but where to begin”, Choroszko’s whirlwind impetus and precision guidance (many very direct practical steps to take) really grease the wheels of progress.
In short, this could be the book that kickstarts your next big “getting everything into better order” drive, with a clear step-by-step this-then-this-then-this linear process.
Share This Post
-
Chia Seeds vs Sunflower Seeds – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing chia seeds to sunflower, we picked the chia.
Why?
It was close, and they both have their merits!
In terms of macros, chia has more carbs and a lot more fiber, while sunflower has a little more protein and a lot more fat. While the fat (in the seeds, not processed seed oils!) is mostly healthy polyunsaturated fat in both cases, chia has a lot more omega-3. All in all, we’re calling it a win for chia on macros.
In the category of vitamins, chia has more of vitmains B3 and C, while sunflower has ore of vitamins B1, B2, B9, and E. Thus, a win for sunflower seeds this time.
When it comes to minerals, chia has more calcium, iron, magnesium, manganese, phosphorus, and selenium, while sunflower has more copper, potassium, and zinc. A 6:3 win for chia here.
Adding up the sections makes for an overall win for chia, but by all means enjoy either or both; diversity is good!
Want to learn more?
You might like to read:
The Tiniest Seeds With The Most Value: If You’re Not Taking Chia, You’re Missing Out!
Take care!
Share This Post
-
Gut-Healthy Labneh Orecchiette
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Labneh (a sort of yogurt-cheese made from strained yogurt) is a great probiotic, and there’s plenty of resistant starch in this dish too, from how we cook, cool, and reheat the pasta. Add to this the lycopene from the tomatoes, the ergothioneine from the mushrooms, and the healthful properties of the garlic, black pepper, and red chili, and we have a very healthy dish!
You will need
- 10 oz labneh (if you can’t buy it locally, you can make your own by straining Greek yogurt through a muslin cloth, suspended over a bowl to catch the water that drips out, overnight—and yes, plant-based is also fine if you are vegan, and the gut benefits are similar because unlike vegan cheese, vegan yogurt is still fermented)
- 6 oz wholegrain orecchiette (or other pasta, but this shape works well for this sauce)
- ¼ bulb garlic, grated
- Juice of ½ lemon
- Large handful chopped parsley
- Large handful chopped dill
- 9 oz cherry tomatoes, halved
- 9 oz mushrooms (your choice what kind), sliced (unless you went for shiitake or similar, which don’t need it due to already being very thin)
- 2 tsp black pepper, coarse ground
- 1 tsp red chili flakes
- ¼ tsp MSG or ½ tsp low-sodium salt
- Extra virgin olive oil
Method
(we suggest you read everything at least once before doing anything)
1) Cook the pasta as you normally would. Drain, and rinse with cold water. Set aside.
2) Combine the labneh with the garlic, black pepper, dill, parsley, and lemon juice, in a large bowl. Set aside.
3) Heat a little olive oil in a skillet; add the chili flakes, followed by the mushrooms. Cook until soft and browned, then add the tomatoes and fry for a further 1 minute—we want the tomatoes to be blistered, but not broken down. Stir in the MSG/salt, and take off the heat.
4) Refresh the pasta by passing a kettle of boiling water through it in a colander, then add the hot pasta to the bowl of labneh sauce, stirring to coat thoroughly.
5) Serve, spooning the mushrooms and tomatoes over the labneh pasta.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Making Friends With Your Gut (You Can Thank Us Later)
- Lycopene’s Benefits For The Gut, Heart, Brain, & More
- “The Longevity Vitamin” (That’s Not A Vitamin)
Take care!
Share This Post
Related Posts
-
How Does One Test Acupuncture Against Placebo Anyway?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Pinpointing The Usefulness Of Acupuncture
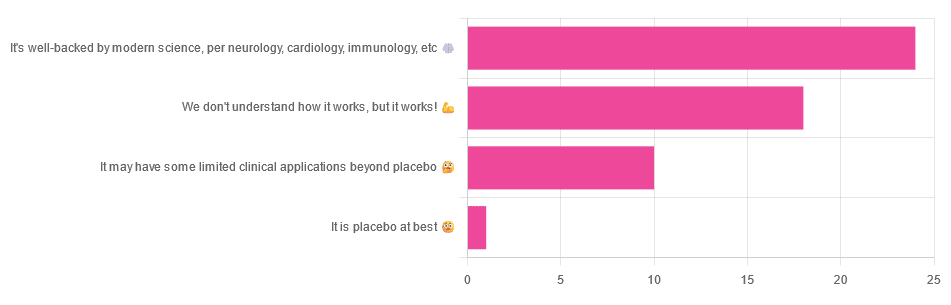
We asked you for your opinions on acupuncture, and got the above-depicted, below-described, set of answers:
- A little under half of all respondents voted for “It’s well-backed by modern science, per neurology, cardiology, immunology, etc”
- Slightly fewer respondents voted for “We don’t understand how it works, but it works!”
- A little under a fifth of respondents voted for “It may have some limited clinical applications beyond placebo”
- One (1) respondent voted for for “It’s placebo at best”
When we did a main feature about homeopathy, a couple of subscribers wrote to say that they were confused as to what homeopathy was, so this time, we’ll start with a quick definition first.
First, what is acupuncture? For the convenience of a quick definition so that we can move on to the science, let’s borrow from Wikipedia:
❝Acupuncture is a form of alternative medicine and a component of traditional Chinese medicine in which thin needles are inserted into the body.
Acupuncture is a pseudoscience; the theories and practices of TCM are not based on scientific knowledge, and it has been characterized as quackery.❞
Now, that’s not a promising start, but we will not be deterred! We will instead examine the science itself, rather than relying on tertiary sources like Wikipedia.
It’s worth noting before we move on, however, that there is vigorous debate behind the scenes of that article. The gist of the argument is:
- On one side: “Acupuncture is not pseudoscience/quackery! This has long been disproved and there are peer-reviewed research papers on the subject.”
- On the other: “Yes, but only in disreputable quack journals created specifically for that purpose”
The latter counterclaim is a) potentially a “no true Scotsman” rhetorical ploy b) potentially true regardless
Some counterclaims exhibit specific sinophobia, per “if the source is Chinese, don’t believe it”. That’s not helpful either.
Well, the waters sure are muddy. Where to begin? Let’s start with a relatively easy one:
It may have some clinical applications beyond placebo: True or False?
True! Admittedly, “may” is doing some of the heavy lifting here, but we’ll take what we can get to get us going.
One of the least controversial uses of acupuncture is to alleviate chronic pain. Dr. Vickers et al, in a study published under the auspices of JAMA (a very respectable journal, and based in the US, not China), found:
❝Acupuncture is effective for the treatment of chronic pain and is therefore a reasonable referral option. Significant differences between true and sham acupuncture indicate that acupuncture is more than a placebo.
However, these differences are relatively modest, suggesting that factors in addition to the specific effects of needling are important contributors to the therapeutic effects of acupuncture❞
Source: Acupuncture for Chronic Pain: Individual Patient Data Meta-analysis
If you’re feeling sharp today, you may be wondering how the differences are described as “significant” and “relatively modest” in the same text. That’s because these words have different meanings in academic literature:
- Significant = p<0.05, where p is the probability of the achieved results occurring randomly
- Modest = the differences between the test group and the control group were small
In other words, “significant modest differences” means “the sample sizes were large, and the test group reliably got slightly better results than placebo”
We don’t understand how it works, but it works: True or False
Broadly False. When it works, we generally have an idea how.
Placebo is, of course, the main explanation. And even in examples such as the above, how is placebo acupuncture given?
By inserting acupuncture needles off-target rather than in accord with established meridians and points (the lines and dots that, per Traditional Chinese Medicine, indicate the flow of qi, our body’s vital energy, and welling-points of such).
So, if a patient feels that needles are being inserted randomly, they may no longer have the same confidence that they aren’t in the control group receiving placebo, which could explain the “modest” difference, without there being anything “to” acupuncture beyond placebo. After all, placebo works less well if you believe you are only receiving placebo!
Indeed, a (Korean, for the record) group of researchers wrote about this—and how this confounding factor cuts both ways:
❝Given the current research evidence that sham acupuncture can exert not only the originally expected non-specific effects but also sham acupuncture-specific effects, it would be misleading to simply regard sham acupuncture as the same as placebo.
Therefore, researchers should be cautious when using the term sham acupuncture in clinical investigations.❞
Source: Sham Acupuncture Is Not Just a Placebo
It’s well-backed by modern science, per neurology, cardiology, immunology, etc: True or False?
False, for the most part.
While yes, the meridians and points of acupuncture charts broadly correspond to nerves and vasculature, there is no evidence that inserting needles into those points does anything for one’s qi, itself a concept that has not made it into Western science—as a unified concept, anyway…
Note that our bodies are indeed full of energy. Electrical energy in our nerves, chemical energy in every living cell, kinetic energy in all our moving parts. Even, to stretch the point a bit, gravitational potential energy based on our mass.
All of these things could broadly be described as qi, if we so wish. Indeed, the ki in the Japanese martial art of aikido is the latter kinds; kinetic energy and gravitational potential energy based on our mass. Same goes, therefore for the ki in kiatsu, a kind of Japanese massage, while the ki in reiki, a Japanese spiritual healing practice, is rather more mystical.
The qi in Chinese qigong is mostly about oxygen, thus indirectly chemical energy, and the electrical energy of the nerves that are receiving oxygenated blood at higher or lower levels.
On the other hand, the efficacy of the use of acupuncture for various kinds of pain is well-enough evidenced. Indeed, even the UK’s famously thrifty NHS (that certainly would not spend money on something it did not find to work) offers it as a complementary therapy for some kinds of pain:
❝Western medical acupuncture (dry needling) is the use of acupuncture following a medical diagnosis. It involves stimulating sensory nerves under the skin and in the muscles.
This results in the body producing natural substances, such as pain-relieving endorphins. It’s likely that these naturally released substances are responsible for the beneficial effects experienced with acupuncture.❞
Source: NHS | Acupuncture
Meanwhile, the NIH’s National Cancer Institute recommends it… But not as a cancer treatment.
Rather, they recommend it as a complementary therapy for pain management, and also against nausea, for which there is also evidence that it can help.
Frustratingly, while they mention that there is lots of evidence for this, they don’t actually link the studies they’re citing, or give enough information to find them. Instead, they say things like “seven randomized clinical trials found that…” and provide links that look reassuring until one finds, upon clicking on them, that it’s just a link to the definition of “randomized clinical trial”:
Source: NIH | Nactional Cancer Institute | Acupuncture (PDQ®)–Patient Version
However, doing our own searches finds many studies (mostly in specialized, potentially biased, journals such as the Journal of Acupuncture and Meridian Studies) finding significant modest outperformance of [what passes for] placebo.
Sometimes, the existence of papers with promising titles, and statements of how acupuncture might work for things other than relief of pain and nausea, hides the fact that the papers themselves do not, in fact, contain any evidence to support the hypothesis. Here’s an example:
❝The underlying mechanisms behind the benefits of acupuncture may be linked with the regulation of the hypothalamic-pituitary-gonadal (adrenal) axis and activation of the Wnt/β-catenin and OPG/RANKL/RANK signaling pathways.
In summary, strong evidence may still come from prospective and well-designed clinical trials to shed light on the potential role of acupuncture in preserving bone loss❞
Source: Acupuncture for Osteoporosis: a Review of Its Clinical and Preclinical Studies
So, here they offered a very sciencey hypothesis, and to support that hypothesis, “strong evidence may still come”.
“We must keep faith” is not usually considered evidence worthy of inclusion in a paper!
PS: the above link is just to the abstract, because the “Full Text” link offered in that abstract leads to a completely unrelated article about HIV/AIDS-related cryptococcosis, in a completely different journal, nothing to do with acupuncture or osteoporosis).
Again, this is not the kind of professionalism we expect from peer-reviewed academic journals.
Bottom line:
Acupuncture reliably performs slightly better than sham acupuncture for the management of pain, and may also help against nausea.
Beyond placebo and the stimulation of endorphin release, there is no consistently reliable evidence that is has any other discernible medical effect by any mechanism known to Western science—though there are plenty of hypotheses.
That said, absence of evidence is not evidence of absence, and the logistical difficulty of testing acupuncture against placebo makes for slow research. Maybe one day we’ll know more.
For now:
- If you find it helps you: great! Enjoy
- If you think it might help you: try it! By a licensed professional with a good reputation, please.
- If you are not inclined to having needles put in you unnecessarily: skip it! Extant science suggests that at worst, you’ll be missing out on slight relief of pain/nausea.
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Six Ways To Eat For Healthier Skin
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Sadia Badiei, the nutritionist-chef of “Pick Up Limes” fame, has advice:
More than skin-deep:
We’ll not keep them a mystery; here are the six points of focus:
1. Collagen and skin elasticity
Collagen is the structural protein that provides firmness and elasticity to the skin, but its production decreases with age, resulting in about a 1% annual loss starting at age 20. To support collagen, a diet rich in protein is essential, including foods like beans, lentils, tofu, tempeh, nuts, and seeds. They can’t do their work alone though; vitamins C and E play a critical role in collagen production and repair, protecting against damage from sun exposure, pollution, and free radicals. Vitamin E can be found in almonds, sunflower seeds, leafy greens, peanuts, and avocados, while vitamin C is abundant in citrus fruits, bell peppers, and broccoli.
2. Skin healing and zinc
Zinc is critical for wound healing and reducing inflammation, making it particularly helpful in managing skin conditions such as acne, eczema, psoriasis, and rosacea. Great dietary sources of zinc include nutritional yeast, pumpkin, sesame, and hemp seeds, as well as legumes and whole grains. However, zinc absorption can be hindered by phytate levels in some foods. Soaking, sprouting, or fermenting foods where possible can correct for that and improve zinc absorption.
3. Dry skin and hydration
Dry skin can result from many things, including dry air, hot water, abrasive soaps, and certain medications. While moisturizers provide external hydration, dietary omega-3 fats are essential for improving the skin’s barrier function, helping it retain moisture. Plant-based sources of omega-3s include walnuts, hemp seeds, chia seeds, flax seeds, and algae-based supplements. Staying adequately hydrated also supports overall health of course (everything runs on water in one way or another, after all), which indirectly benefits skin hydration, although drinking additional water only helps if dehydration is present.
4. Sebum regulation
Sebum, an oily substance that lubricates the skin, can cause issues like acne and blackheads when overproduced. Hormonal fluctuations and diet both influence sebum levels (in either direction). High glycemic index foods, such as sweetened beverages, refined grains, and sugary snacks, can lead to spikes in insulin, which in turn stimulates excess sebum production. In contrast, low glycemic index foods like vegetables, whole grains, tofu, nuts, and seeds regulate blood sugar and help manage sebum production, promoting clearer skin without an excess or a shortage of sebum.
5. Gut health and skin
The gut-skin connection means that imbalances in gut bacteria can contribute to skin issues like acne, eczema, and psoriasis. Supporting gut health involves increasing the diversity of beneficial bacteria through probiotic-rich foods. Fermented options like plant-based yogurts, kimchi, miso, sauerkraut, and kombucha not only improve gut microbiome health but also positively impact skin health by reducing inflammation and improving overall skin conditions.
6. Inflammation and skin health
Chronic inflammation is associated with so many health issues, and when it comes to skin, that includes acne, rosacea, and even wrinkles. Anti-inflammatory foods, especially those rich in antioxidants, can mitigate these effects and improve skin elasticity, smoothness, and color. Diets centered around fruits, vegetables, and other plant-based foods provide the necessary nutrients to combat inflammation, showcasing the significant role of nutrition in promoting radiant, healthy skin.
For more on each of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Undo The Sun’s Damage To Your Skin
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Black Pepper’s Impressive Anti-Cancer Arsenal
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Black Pepper’s Impressive Anti-Cancer Arsenal (And More)
Piperine, a compound found in Piper nigrum (black pepper, to its friends), has many health benefits. It’s included as a minor ingredient in some other supplements, because it boosts bioavailability. In its form as a kitchen spice, it’s definitely a superfood.
What does it do?
First, three things that generally go together:
These things often go together for the simple reason that oxidative stress, inflammation, and cancer often go together. In each case, it’s a matter of cellular wear-and-tear, and what can mitigate that.
For what it’s worth, there’s generally a fourth pillar: anti-aging. This is again for the same reason. That said, black pepper hasn’t (so far as we could find) been studied specifically for its anti-aging properties, so we can’t cite that here as an evidence-based claim.
Nevertheless, it’s a reasonable inference that something that fights oxidation, inflammation, and cancer, will often also slow aging.
Special note on the anti-cancer properties
We noticed two very interesting things while researching piperine’s anti-cancer properties. It’s not just that it reduces cancer risk and slows tumor growth in extant cancers (as we might expect from the above-discussed properties). Let’s spotlight some studies:
It is selectively cytotoxic (that’s a good thing)
Piperine was found to be selectively cytotoxic to cancerous cells, while not being cytotoxic to non-cancerous cells. To this end, it’s a very promising cancer-sniper:
Piperine as a Potential Anti-cancer Agent: A Review on Preclinical Studies
It can reverse multi-drug resistance in cancer cells
P-glycoprotein, found in our body, is a drug-transporter that is known for “washing out” chemotherapeutic drugs from cancer cells. To date, no drug has been approved to inhibit P-glycoprotein, but piperine has been found to do the job:
Targeting P-glycoprotein: Investigation of piperine analogs for overcoming drug resistance in cancer
What’s this about piperine analogs, though? Basically the researchers found a way to “tweak” piperine to make it even more effective. They called this tweaked version “Pip1”, because calling it by its chemical name,
((2E,4E)-5-(benzo[d][1,3]dioxol-5-yl)-1-(6,7-dimethoxy-3,4-dihydroisoquinolin-2(1 H)-yl)penta-2,4-dien-1-one)
…got a bit unwieldy.
The upshot is: Pip1 is better, but piperine itself is also good.
Other benefits
Piperine does have other benefits too, but the above is what we were most excited to talk about today. Its other benefits include:
- Neuroprotective effects (against Alzheimer’s, Parkinson’s, and more)
- Blood-sugar balancing / antidiabetic effect
- Good for gut microbiome diversity
- Heart health benefits, including cholesterol-balancing
- Boosts bioavailability of other nutrients/drugs
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: