Eat To Beat Chronic Fatigue!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How To Eat To Beat Chronic Fatigue
Chronic fatigue is on the rise, and it can make life a living Hell. Days blur into one, and you try to take each day as it comes, but sometimes several days gang up on you at once.
You probably know some lifestyle changes that might help—if only you had the energy to implement them.
You’d like to eat well, but you need to…
- Buy the fresh produce (and take a little rest after)
- Put the groceries away (and take a little rest after)
- Wash the vegetables (and take a little rest after)
- Chop the things as necessary (and take a little rest after)
- Cook dinner (and take a little rest after)
…and now you’re too exhausted to eat it.
So, what can be done?
First, avoid things that cause inflammation, as this is a major contributor to chronic fatigue. You might like our previous main feature:
Next up, really do stay hydrated. It’s less about quantity, and more about ubiquity. Hydrate often.
Best is if you always have some (hydrating) drink on the go.
Do experiment with your diet, and/but keep a food journal of what you eat and how you feel 30–60 minutes after eating it. Only make one change at a time, otherwise you won’t know which change made the difference.
Notice what patterns emerge over time, and adjust your ingredients accordingly.
Limit your caffeine intake. We know that sometimes it seems like the only way to get through the day, but you will always crash later, because it was only ever taxing your adrenal system (thus: making you more tired in the long run) and pulling the wool over the eyes of your adenosine receptors (blocking you from feeling how tired you are, but not actually reducing your body’s tiredness).
Put simply, caffeine is the “payday loan” of energy.
Eat more non-starchy vegetables, and enjoy healthy fats. Those healthy fats can come from nuts and seeds, avocado, or fish (not fried, though!).
The non-starchy vegetables will boost your vitamins and fiber while being easy on your beleaguered metabolism, while the healthy fats will perk up your energy levels without spiking insulin like sugars would.
Pay the fatigue tax up front. What this means is… Instead of throwing away vegetables that didn’t get used because it would take too much effort and you just need an easier dinner today, buy ready-chopped vegetables, for example.
And if you buy vegetables frozen, they’re also often not only cheaper, but also (counterintuitively) contain more nutrients.
A note of distinction:
Many more people have chronic fatigue (the symptom: being exhausted all the time) than have chronic fatigue syndrome (the illness: myalgic encephalomyelitis).
This is because fatigue can be a symptom of many, many other conditions, and can be heavily influenced by lifestyle factors too.
A lot of the advice for dealing with chronic fatigue is often the same in both cases, but some will be different, because for example:
- If your fatigue is from some other condition, that condition probably impacts what lifestyle factors you are (and are not) able to change, too
- If your fatigue is from lifestyle factors, that hopefully means you can change those and enjoy less fatigue…
- But if it’s not from lifestyle factors, as in ME/CFS, then advice to “exercise more” etc is not going to help so much.
There are ways to know the difference though:
Check out: Do You Have Chronic Fatigue Syndrome?
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Delicious Quinoa Avocado Bread
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
They’re gluten-free, full of protein and healthy fats, generous with the fiber, easy to make, and tasty too! What’s not to love? Keep this recipe (and its ingredients) handy for next time you want healthy burger buns or similar:
You will need
- 2½ cups quinoa flour
- 2 cups almond flour (if allergic, just substitute more quinoa flour)
- 1 avocado, peeled, pitted, and mashed
- zest and juice of 1 lime
- 2 tbsp ground flaxseed
- 1 tsp baking powder
- ½ tsp MSG or 1 tsp low-sodium salt
- Optional: seeds, oats, or similar for topping the buns
Method
(we suggest you read everything at least once before doing anything)
1) Preheat the oven to 350℉/175℃.
2) Mix the flaxseed with ⅓ cup warm water and set aside.
3) Mix, in a large bowl, the quinoa flour and almond flour with the baking powder and the MSG or salt.
4) Mix, in a separate smaller bowl, the avocado and lime.
5) Add the wet ingredients to the dry, slowly, adding an extra ½ cup water as you do, and knead into a dough.
6) Divide the dough into 4 equal portions, each shaped into a ball and then slightly flattened, to create a burger bun shape. If you’re going to add any seeds or similar as a topping, add those now.
7) Bake them in the oven (on a baking sheet lined with baking paper) for 20–25 minutes. You can check whether they’re done the same way you would a cake, by piercing them to the center with a toothpick and seeing whether it comes out clean.
8) Serve when sufficiently cooled.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Gluten: What’s The Truth?
- Why You Should Diversify Your Nuts!
- Monosodium Glutamate: Sinless Flavor-Enhancer Or Terrible Health Risk?
Take care!
Share This Post
-
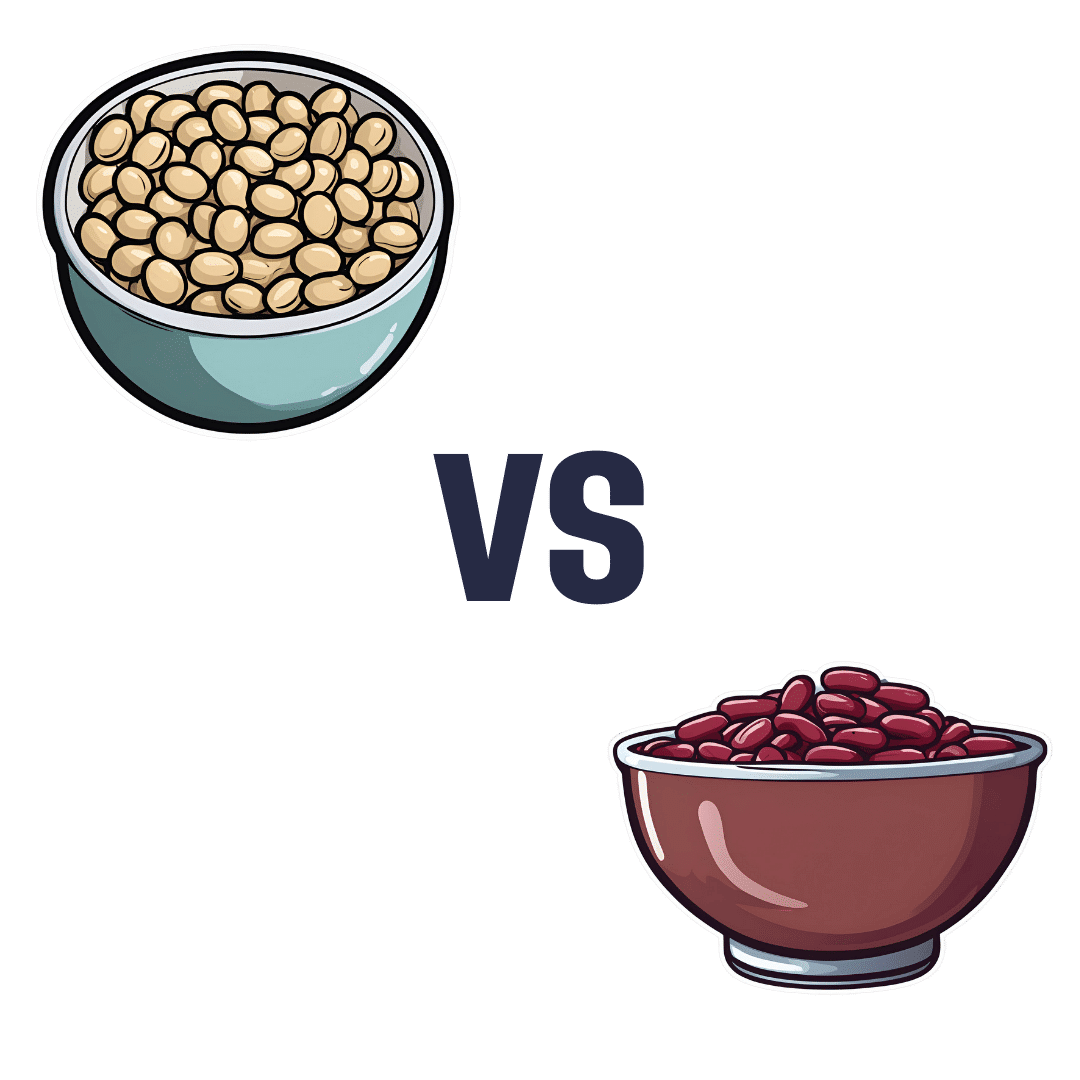
Soy Beans vs Kidney Beans – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing soy beans to kidney beans, we picked the soy.
Why?
In terms of macros, soy has 2x the protein, while kidney beans have nearly 3x the carbs and very slightly more fiber. Ratio-wise, the “very slightly more fiber” does not offset the “nearly 3x the carbs” when it comes to glycemic index (though both are still good, really, but this is a head-to-head so the comparison is relevant), and 2x the protein is also quite a bonus, so this category’s an easy win for soy.
In the category of vitamins, soy beans have more of vitamins A, B2, B6, C, E, K, and choline, while kidney beans have more of vitamins B3, B5, and B9, thus making for a 7:3 win for soy.
When it comes to minerals, soy beans have more calcium, copper, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc, while kidney beans are not higher in any mineral. Another clear win for soy.
Adding up the three strong wins for soy, makes for an overall easy win for soy. Still, enjoy either or both; diversity is good!
Want to learn more?
You might like to read:
Plant vs Animal Protein: Head to Head
Take care!
Share This Post
-
Radical CBT
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Radical Acceptance!
A common criticism of Cognitive Behavioral Therapy (CBT) is that much of it hinges on the following process:
- You are having bad feelings
- Which were caused by negative automatic thoughts
- Which can be taken apart logically
- Thus diffusing the feelings
- And then feeling better
For example:
- I feel like I’m an unwanted burden to my friend
- Because he canceled on me today
- But a reasonable explanation is that he indeed accidentally double-booked himself and the other thing wasn’t re-arrangeable
- My friend is trusting me to be an understanding friend myself, and greatly values my friendship
- I feel better and look forward to our next time together
But what if the negative automatic thoughts are, upon examination, reasonable?
Does CBT argue that we should just “keep the faith” and go on looking at a cruel indifferent world through rose-tinted spectacles?
Nope, there’s a back-up tool.
This is more talked-about in Dialectic Behavior Therapy (DBT), and is called radical acceptance:
Click Here If The Embedded Video Doesn’t Load automatically!
Radical acceptance here means accepting the root of things as true, and taking the next step from there. It follows a bad conclusion with “alright, and now what?”
“But all evidence points to the fact that my friend has been avoiding me for months; I really can’t ignore it or explain it away any longer”
“Alright. Now what?”- Maybe there’s something troubling your friend that you don’t know about (have you asked?)
- Maybe that something is nothing to do with you (or maybe it really is about you!)
- Maybe there’s a way you and he can address it together (how important is it to you?)
- Maybe it’s just time to draw a line under it and move on (with or without him)
Whatever the circumstances, there’s always a way to move forwards.
Feelings are messengers, and once you’ve received and processed the message, the only reason to keep feeling the same thing, is if you want to.
Note that this is true even when you know with 100% certainty that the Bad Thing™ is real and exactly as-imagined. It’s still possible for you to accept, for example:
“Alright, so this person really truly hates me. Damn, that sucks; I think I’ve been nothing but nice to them. Oh well. Shit happens.”
Feel all the feelings you need to about it, and then decide for yourself where you want to go from there.
Get: 25 CBT Worksheets To Help You Find Solutions To A Wide Variety of Problems
Recognizing Emotions
We talked in a previous edition of 10almonds’ Psychology Sunday about how an important part of dealing with difficult emotions is recognizing them as something that you experience, rather than something that’s intrinsically “you”.
But… How?
One trick is to just mentally (or out loud, if your current environment allows for such) greet them when you notice them:
- Hello again, Depression
- Oh, hi there Anxiety, it’s you
- Nice of you to join us, Anger
Not only does this help recognize and delineate the emotion, but also, it de-tooths it and recognizes it for what it is—something that doesn’t actually mean you any harm, but that does need handling.
Share This Post
Related Posts
-
How Processed Is The Food You Buy, Really?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Ultraprocessed foods are a) ubiquitous in industrialized nations b) generally not fabulous for the health. See for example:
- Eat To Beat Cancer ← skipping the ultraprocessed foods is one main point
- What To Leave Off Your Table (To Stay Off This Surgeon’s) ← have a guess
Abstaining from ultraprocessed food can also be difficult psychologically, because they are generally engineered specifically to trigger certain physiological responses, often with their combination of sweet and/or salty flavors with simple carbohydrates that will zip straight into one’s veins and feel immediately rewarding, even if there is a health price to pay later.
And worse, being habituated to ultraprocessed food can make unprocessed or minimally-processed food seem less appealing:
What causes food cravings? And what can we do about them?
Fortunately, we can reverse this, and once we get habituated to unprocessed or minimally-processed food, the ultraprocessed will start to seem like not-food to us. You will wonder: how did I ever eat that crap?
Now, one other thing to bear in mind:
There is a scale of “badness”
You might recall this article:
Not all ultra-processed foods are bad for your health, whatever you might have heard
For example, Reese’s confectionary and Huel nutrition powder are both ultra-processed, but one is definitely better than the other.
See also: Are plant-based burgers really bad for your heart? Here’s what’s behind the scary headlines
Some comparisons are obvious; others, not so much. So, how to tell the difference?
The “True Food” Scale
A large study analyzed ingredient lists, nutrition facts, and prices of over 50,000 food items from Target, Whole Foods, and Walmart. Using a rigorous statistical method, they assigned processing scores and compiled data into a giant database, with results published publicly.
You can find the study here:
Prevalence of processed foods in major US grocery stores
That in and of itself doesn’t tell a lot that’s useful to the consumer, because the paper itself does not have all of the data from all 50,000 food items, just the aggregate results, trends, implications for public health, and suggestions for public health policy.
However, what does tell a lot, is the public face of the database itself, which you can browse for free, and look up your regular shopping items, if you are wondering “are these textured soy pieces basically a step away from soy beans, or a frankenfood that will murder me in my sleep?”
How it works: it examines each food, its listed ingredients, and what is known about the processedness of such ingredients. It also draws a distinction between ingredients and additives, rendering the entire process of the production of the food into an “ingredient tree”, showing what was added to what along the way. Minimally-processed foods will have barely an ingredient sapling, while ultraprocessed foods will have an ingredient tree whose branches can barely be counted, they are so numerous. It’s not just about the number of ingredients though; it’s about the processes that each underwent.
How it represents this data: you can look at the food in the database, and it’ll tell you the ingredients and nutritional facts (which you probably knew already; it’s written on the packaging), and then show you how processed it is, and then ranking that against all other foods in the database of the same kind.
So for example, if you are looking at a pizza (have you ever noticed how some are marketed with bright flashy colors, and others in natural tones to suggest minimal processing? This is marketing, not reliable information! Sometimes the product that looks healthier, isn’t!), then it’ll give it a score reflecting how it ranks compared to all other pizze in the database. This number is out of a hundred, and it reflects the percentile into which it falls.
So for example, if the score your pizza gets is 47, then that means that if you looked at it next to 99 others, on average your pizza would would rank better than 46 of them and worse than 53 of them.
In other words, the lower the score, the less processed it is on the whole.
Here’s a side-by-side example of two cakes, one of which got a score of 3, and the other got a score of 61:
Mini No Sugar Added Cheesecake vs EDWARDS Desserts Original Whipped Cheesecake
And here is the main menu of the database, in which you can use the search function to look up the food you want to check, or else browse by category:
The TrueFood Database: Search or Browse (it’s free!)
Enjoy!
Want to know more?
You might like this book that we reviewed a little while back:
Ultra-Processed People: The Science Behind Food That Isn’t Food – by Dr. Chris van Tulleken
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Pegan Diet – by Dr. Mark Hyman
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
First things first: the title of the book is a little misleading. “Pegan” is a portmanteau of “paleo” and “vegan”, making it sound like it will be appropriate for both of those dietary practices. Instead:
- Dr. Hyman offers advice about eating the right grains and legumes (inappropriate for a paleo diet)
- He also offers such advice as “be picky about poultry, eggs, and fish”, and “avoid dairy—mostly” (inappropriate for a vegan diet).
So, since his paleo vegan diet is neither paleo nor vegan, what actually is it?
It’s a whole foods diet that encourages the enjoyment of a lot of plants, and discretion with regard to the quality of animal products.
It’s a very respectable approach to eating, even if it didn’t live up to the title.
The style is somewhat sensationalist, while nevertheless including plenty of actual science in there too—so the content is good, even if the presentation isn’t what this reviewer would prefer.
He has recipes; they can be a little fancy (e.g. “matcha poppy bread with rose water glaze”) which may not be to everyone’s taste, but they are healthy.
Bottom line: the content is good; the style you may love or hate, and again, don’t be misled by the title.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Intelligence Trap – by David Robson
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’re including this one under the umbrella of “general wellness”, because it happens that a lot of very intelligent people make stunningly unfortunate choices sometimes, for reasons that may baffle others.
The author outlines for us the various reasons that this happens, and how. From the famous trope of “specialized intelligence in one area”, to the tendency of people who are better at acquiring knowledge and understanding to also be better at acquiring biases along the way, to the hubris of “I am intelligent and therefore right as a matter of principle” thinking, and many other reasons.
Perhaps the greatest value of the book is the focus on how we can avoid these traps, narrow our bias blind spots, and play to our strengths while paying full attention to our weaknesses.
The style is very readable, despite having a lot of complex ideas discussed along the way. This is entirely to be expected of this author, an award-winning science writer.
Bottom line: if you’d like to better understand the array of traps that disproportionately catch out the most intelligent people (and how to spot such), then this is a great book for you.
Click here to check out The Intelligence Trap, and be more wary!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: