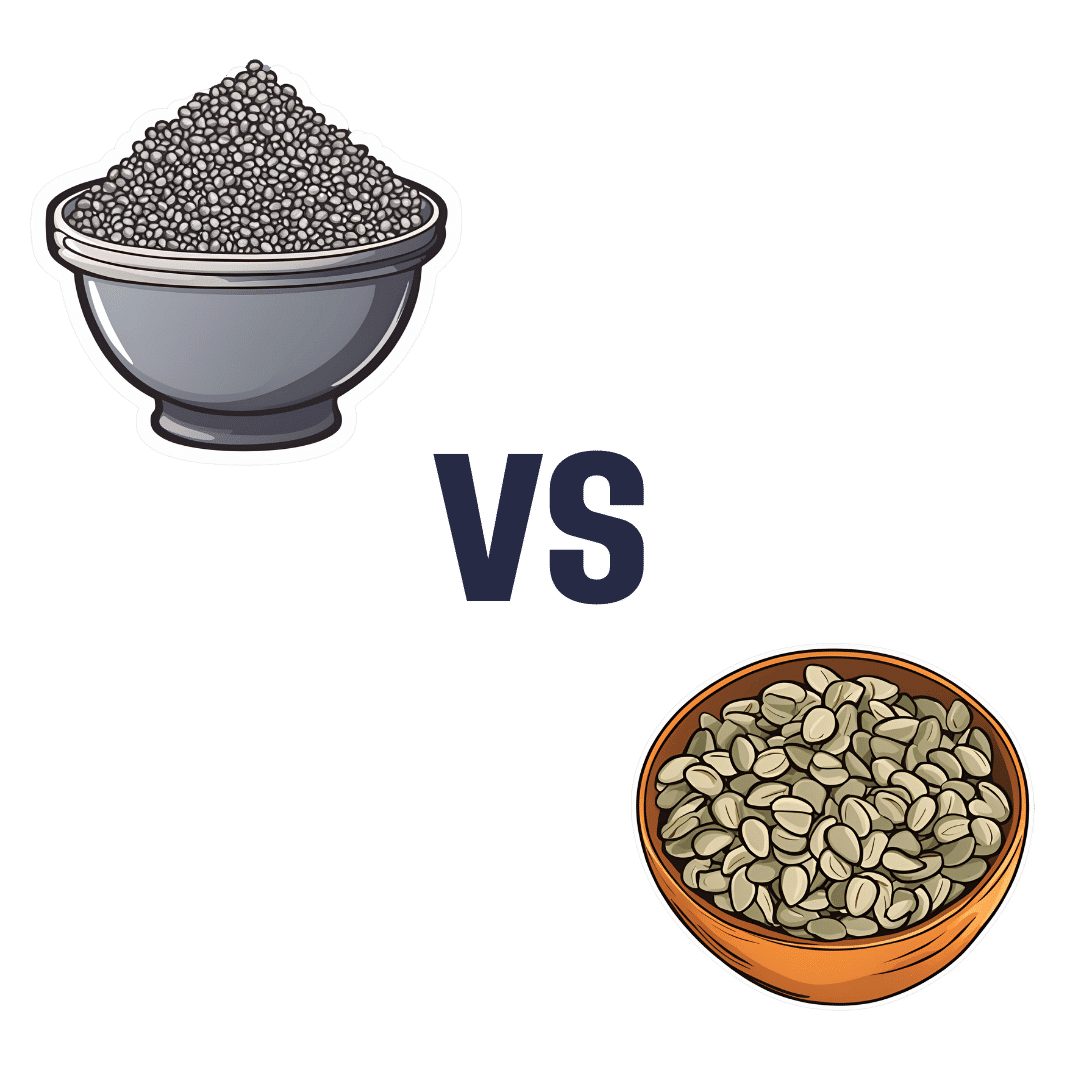
Chia Seeds vs Pumpkin Seeds – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing chia seeds to pumpkin seeds, we picked the chia.
Why?
Both are great! But chia is best.
Note: we’re going to abbreviate them both to “chia” and “pumpkin”, respectively, but we’ll still be referring to the seeds throughout.
In terms of macros, pumpkin has a little more protein and notably higher carbs, whereas chia has nearly 2x the fiber, as well as more fat, and/but they are famously healthy fats. We’ll call this category a subjective win for chia, though you might disagree if you want to prioritize an extra 2g of protein per 100g (for pumpkin) over an extra 16g of fiber per 100g (for chia). Chia is also vastly preferable for omega-3.
When it comes to vitamins, pumpkin is marginally higher in vitamin A, while chia is a lot higher in vitamins B1, B2, B3, B9, C, and E. An easy win for chia.
In the category of minerals, for which pumpkin seeds are so famously a good source, chia has a lot more calcium, copper, iron, magnesium, manganese, phosphorus, and selenium. On the other hand, pumpkin has more potassium and zinc. Still, that’s a 7:2 win for chia.
Adding up the categories makes for a very compelling win for the humble chia seed.
Want to learn more?
You might like to read:
If You’re Not Taking Chia, You’re Missing Out: The Tiniest Seeds With The Most Value
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Is stress turning my hair grey?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When we start to go grey depends a lot on genetics.
Your first grey hairs usually appear anywhere between your twenties and fifties. For men, grey hairs normally start at the temples and sideburns. Women tend to start greying on the hairline, especially at the front.
The most rapid greying usually happens between ages 50 and 60. But does anything we do speed up the process? And is there anything we can do to slow it down?
You’ve probably heard that plucking, dyeing and stress can make your hair go grey – and that redheads don’t. Here’s what the science says.
Oksana Klymenko/Shutterstock What gives hair its colour?
Each strand of hair is produced by a hair follicle, a tunnel-like opening in your skin. Follicles contain two different kinds of stem cells:
- keratinocytes, which produce keratin, the protein that makes and regenerates hair strands
- melanocytes, which produce melanin, the pigment that colours your hair and skin.
There are two main types of melanin that determine hair colour. Eumelanin is a black-brown pigment and pheomelanin is a red-yellow pigment.
The amount of the different pigments determines hair colour. Black and brown hair has mostly eumelanin, red hair has the most pheomelanin, and blonde hair has just a small amount of both.
So what makes our hair turn grey?
As we age, it’s normal for cells to become less active. In the hair follicle, this means stem cells produce less melanin – turning our hair grey – and less keratin, causing hair thinning and loss.
As less melanin is produced, there is less pigment to give the hair its colour. Grey hair has very little melanin, while white hair has none left.
Unpigmented hair looks grey, white or silver because light reflects off the keratin, which is pale yellow.
Grey hair is thicker, coarser and stiffer than hair with pigment. This is because the shape of the hair follicle becomes irregular as the stem cells change with age.
Interestingly, grey hair also grows faster than pigmented hair, but it uses more energy in the process.
Can stress turn our hair grey?
Yes, stress can cause your hair to turn grey. This happens when oxidative stress damages hair follicles and stem cells and stops them producing melanin.
Oxidative stress is an imbalance of too many damaging free radical chemicals and not enough protective antioxidant chemicals in the body. It can be caused by psychological or emotional stress as well as autoimmune diseases.
Environmental factors such as exposure to UV and pollution, as well as smoking and some drugs, can also play a role.
Melanocytes are more susceptible to damage than keratinocytes because of the complex steps in melanin production. This explains why ageing and stress usually cause hair greying before hair loss.
Scientists have been able to link less pigmented sections of a hair strand to stressful events in a person’s life. In younger people, whose stems cells still produced melanin, colour returned to the hair after the stressful event passed.
4 popular ideas about grey hair – and what science says
1. Does plucking a grey hair make more grow back in its place?
No. When you pluck a hair, you might notice a small bulb at the end that was attached to your scalp. This is the root. It grows from the hair follicle.
Plucking a hair pulls the root out of the follicle. But the follicle itself is the opening in your skin and can’t be plucked out. Each hair follicle can only grow a single hair.
It’s possible frequent plucking could make your hair grey earlier, if the cells that produce melanin are damaged or exhausted from too much regrowth.
2. Can my hair can turn grey overnight?
Legend says Marie Antoinette’s hair went completely white the night before the French queen faced the guillotine – but this is a myth.
It is not possible for hair to turn grey overnight, as in the legend about Marie Antoinette. Yann Caradec/Wikimedia, CC BY-NC-SA Melanin in hair strands is chemically stable, meaning it can’t transform instantly.
Acute psychological stress does rapidly deplete melanocyte stem cells in mice. But the effect doesn’t show up immediately. Instead, grey hair becomes visible as the strand grows – at a rate of about 1 cm per month.
Not all hair is in the growing phase at any one time, meaning it can’t all go grey at the same time.
3. Will dyeing make my hair go grey faster?
This depends on the dye.
Temporary and semi-permanent dyes should not cause early greying because they just coat the hair strand without changing its structure. But permanent products cause a chemical reaction with the hair, using an oxidising agent such as hydrogen peroxide.
Accumulation of hydrogen peroxide and other hair dye chemicals in the hair follicle can damage melanocytes and keratinocytes, which can cause greying and hair loss.
4. Is it true redheads don’t go grey?
People with red hair also lose melanin as they age, but differently to those with black or brown hair.
This is because the red-yellow and black-brown pigments are chemically different.
Producing the brown-black pigment eumelanin is more complex and takes more energy, making it more susceptible to damage.
Producing the red-yellow pigment (pheomelanin) causes less oxidative stress, and is more simple. This means it is easier for stem cells to continue to produce pheomelanin, even as they reduce their activity with ageing.
With ageing, red hair tends to fade into strawberry blonde and silvery-white. Grey colour is due to less eumelanin activity, so is more common in those with black and brown hair.
Your genetics determine when you’ll start going grey. But you may be able to avoid premature greying by staying healthy, reducing stress and avoiding smoking, too much alcohol and UV exposure.
Eating a healthy diet may also help because vitamin B12, copper, iron, calcium and zinc all influence melanin production and hair pigmentation.
Theresa Larkin, Associate Professor of Medical Sciences, University of Wollongong
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Okra vs Asparagus – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing okra to asparagus, we picked the okra.
Why?
Both are great! But…
In terms of macros, okra has more fiber and carbs, making it the more nutrient dense option, for a similar glycemic index.
In the category of vitamins, okra has more of vitamins B1, B3, B6, B9, and C, while asparagus has more of vitamins B2, B5, E, K, and choline, making for a 5:5 tie, with similar margins of difference too. Thus, definitely a tie on vitamins.
When it comes to minerals, okra has more calcium, magnesium, manganese, phosphorus, potassium, and zinc, while asparagus has more copper, iron, and selenium. An easy 6:3 win for okra.
Both of these on-the-cusp-of-being-pungent vegetables have beneficial antioxidant polyphenols (especially various forms of quercetin), but okra has more.
Adding up the sections makes for an overall win for okra, but by all means enjoy either both; diversity is good!
Want to learn more?
You might like to read:
Enjoy Bitter/Astringent/Pungent Foods For Your Heart & Brain
Enjoy!
Share This Post
-
Sweet Dreams Are Made Of Cheese (Or Are They?)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝In order to lose a little weight I have cut out cheese from my diet – and am finding that I am sleeping better. Would be interested in your views on cheese and sleep, and whether some types of cheese are worse for sleep than others. I don’t want to give up cheese entirely!❞
In principle, there’s nothing in cheese that, biochemically, should impair sleep. If anything, its tryptophan content could aid good sleep.
Tryptophan is found in many foods, including cheese, which (of common foods, anyway), for example cheddar cheese ranks second only to pumpkin seeds in tryptophan content.
Tryptophan can be converted by the body into 5-HTP, which you’ve maybe seen sold as a supplement. Its full name is 5-hydroxytryptophan.
5-HTP can, in turn, be used to make melatonin and/or serotonin. Which of those you will get more of, depends on what your body is being cued to do by ambient light/darkness, and other environmental cues.
If you are having cheese and then checking your phone, for instance, or otherwise hanging out where there are white/blue lights, then your body may dutifully convert the tryptophan into serotonin (calm wakefulness) instead of melatonin (drowsiness and sleep).
In short: the cheese will (in terms of this biochemical pathway, anyway) augment some sleep-inducing or wakefulness-inducing cues, depending on which are available.
You may be wondering: what about casein?
Casein is oft-touted as producing deep sleep, or disturbed sleep, or vivid dreams, or bad dreams. There’s no science to back any of this up, though the following research review is fascinating:
Dreams of the Rarebit Fiend: food and diet as instigators of bizarre and disturbing dreams
(it largely supports the null hypothesis of “not a causal factor” but does look at the many more likely alternative explanations, ranging from associated actually casual factors (such as alcohol and caffeine) and placebo/nocebo effect)
Finally, simple digestive issues may be the real thing at hand:
Worth noting that around two thirds of all people, including those who regularly enjoy dairy products, have some degree of lactose intolerance:
Lactose Intolerance in Adults: Biological Mechanism and Dietary Management
So, in terms of what cheese may be better/worse for you in this context, you might try experimenting with lactose-free cheese, which will help you identify whether that was the issue!
Share This Post
Related Posts
-
Can a child legally take puberty blockers? What if their parents disagree?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Young people’s access to gender-affirming medical care has been making headlines this week.
Today, federal Health Minister Mark Butler announced a review into health care for trans and gender-diverse children and adolescents. The National Health and Medical Research Council will conduct the review.
Yesterday, The Australian published an open letter to Prime Minister Anthony Albanese calling for a federal inquiry, and a nationwide pause on puberty blockers and hormone therapy for minors.
This followed Queensland Health Minister Tim Nicholls earlier this week announcing an immediate pause on access to puberty blockers and hormone therapies for new patients under 18 in the state’s public health system, pending a review.
In the United States, President Donald Trump signed an executive order this week directing federal agencies to restrict access to gender-affirming care for anyone under 19.
This recent wave of political attention might imply gender-affirming care for young people is risky, controversial, perhaps even new.
But Australian courts have already extensively tested questions about its legitimacy, the conditions under which it can be provided, and the scope and limits of parental powers to authorise it.
MirasWonderland/Shutterstock What are puberty blockers?
Puberty blockers suppress the release of oestrogen and testosterone, which are primarily responsible for the physical changes associated with puberty. They are generally safe and used in paediatric medicine for various conditions, including precocious (early) puberty, hormone disorders and some hormone-sensitive cancers.
International and domestic standards of care state that puberty blockers are reversible, non-harmful, and can prevent young people from experiencing the distress of undergoing a puberty that does not align with their gender identity. They also give young people time to develop the maturity needed to make informed decisions about more permanent medical interventions further down the line.
Puberty blockers are one type of gender-affirming care. This care includes medical, psychological and social interventions to support transgender, gender-diverse and, in some cases, intersex people.
Young people in Australia need a medical diagnosis of gender dysphoria to receive this care. Gender dysphoria is defined as the psychological distress that can arise when a person’s gender identity does not align with their sex assigned at birth. This diagnosis is only granted after an exhaustive and often onerous medical assessment.
After a diagnosis, treatment may involve hormones such as oestrogen or testosterone and/or puberty-blocking medications.
Hormone therapies involving oestrogen and testosterone are only prescribed in Australia once a young person has been deemed capable of giving informed consent, usually around the age of 16. For puberty blockers, parents can consent at a younger age.
Gender dysphoria comes with considerable psychological distress. slexp880/Shutterstock Can a child legally access puberty blockers?
Gender-affirming care has been the subject of extensive debate in the Family Court of Australia (now the Federal Circuit and Family Court).
Between 2004 and 2017, every minor who wanted to access gender-affirming care had to apply for a judge to approve it. However, medical professionals, human rights organisations and some judges condemned this process.
In research for my forthcoming book, I found the Family Court has heard at least 99 cases about a young person’s gender-affirming care since 2004. Across these cases, the court examined the potential risks of gender-affirming treatment and considered whether parents should have the authority to consent on their child’s behalf.
When determining whether parents can consent to a particular medical procedure for their child, the court must consider whether the treatment is “therapeutic” and whether there is a significant risk of a wrong decision being made.
However, in a landmark 2017 case, the court ruled that judicial oversight was not required because gender-affirming treatments meet the standards of normal medical care.
It reasoned that because these therapies address an internationally recognised medical condition, are supported by leading professional medical organisations, and are backed by robust clinical research, there is no justification for treating them differently from any other standard medical intervention. These principles still stand today.
What if parents disagree?
Sometimes parents disagree with decisions about gender-affirming care made by their child, or each other.
As with all forms of health care, under Australian law, parents and legal guardians are responsible for making medical decisions on behalf of their children. That responsibility usually shifts once those children reach a sufficient age and level of maturity to make their own decisions.
However, in another landmark case in 2020, the court ruled gender-affirming treatments cannot be given to minors without consent from both parents, even if the child is capable of providing their own consent. This means that if there is any disagreement among parents and the young person about either their capacity to consent or the legitimacy of the treatment, only a judge can authorise it.
In such instances, the court must assess whether the proposed treatment is in the child’s best interests and make a determination accordingly. Again, these principals apply today.
If a parent disagrees with their child, the matter can go to court. PeopleImages.com – Yuri A/Shutterstock Have the courts ever denied care?
Across the at least 99 cases the court has heard about gender-affirming care since 2004, 17 have involved a parent opposing the treatment and one has involved neither parent supporting it.
Regardless of parental support, in every case, the court has been responsible for determining whether gender-affirming treatment was in the child’s best interests. These decisions were based on medical evidence, expert testimony, and the specific circumstances of the young person involved.
In all cases bar one, the court has found overwhelming evidence to support gender-affirming care, and approved it.
Supporting transgender young people
The history of Australia’s legal debates about gender-affirming care shows it has already been the subject of intense legal and medical scrutiny.
Gender-affirming care is already difficult for young people to access, with many lacking the parental support required or facing other barriers to care.
Gender-affirming care is potentially life-saving, or at the very least life-affirming. It almost invariably leads to better social and emotional outcomes. Further restricting access is not the “protection” its opponents claim.
If this article has raised issues for you, or if you’re concerned about someone you know, call Lifeline on 13 11 14. For LGBTQIA+ peer support and resources, you can also contact Switchboard, QLife (call 1800 184 527), Queerspace, Transcend Australia (support for trans, gender-diverse, and non-binary young people and their families) or Minus18 (resources and community support for LGBTQIA+ young people).
Matthew Mitchell, Lecturer in Criminology, Deakin University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
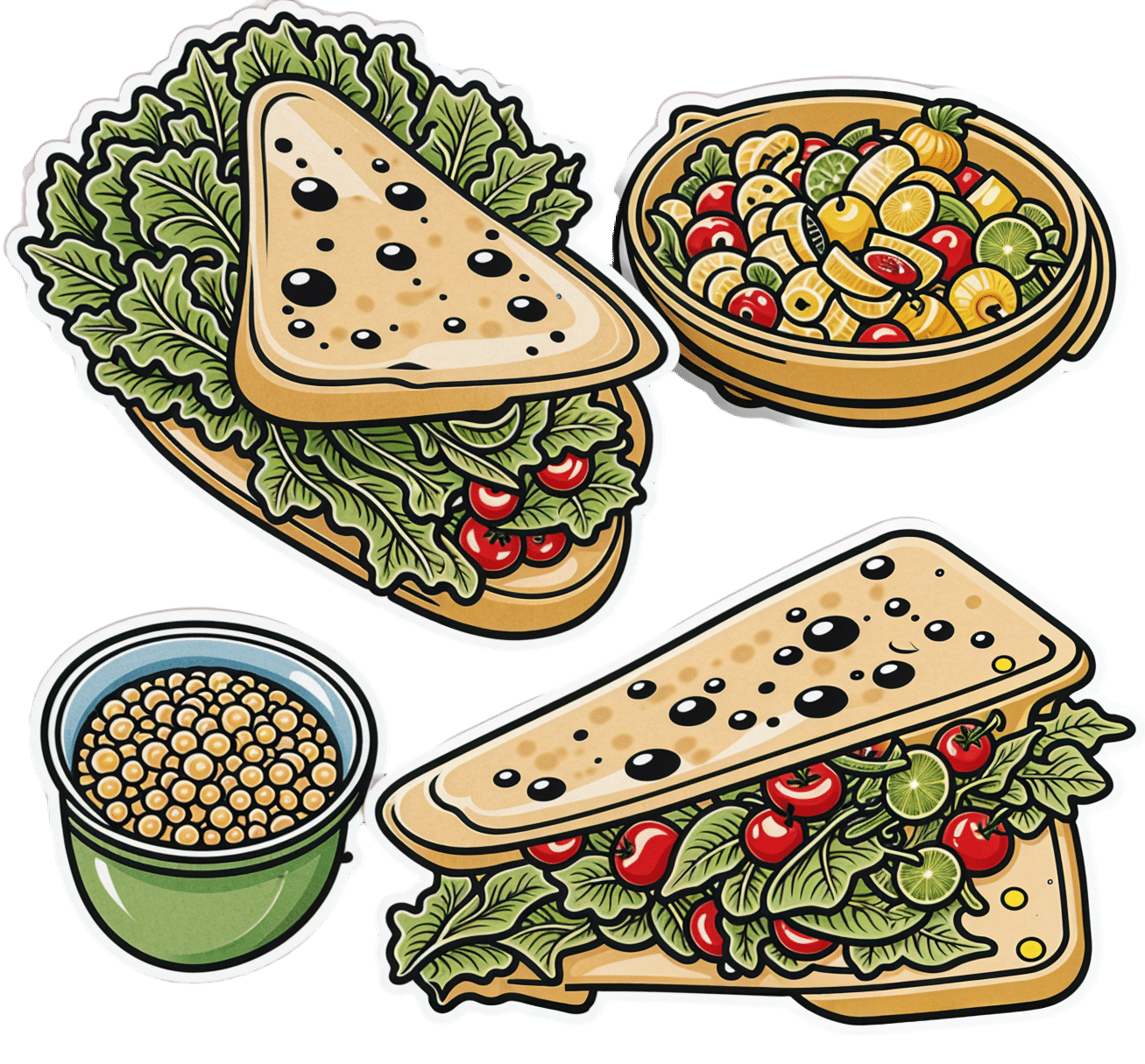
Green Paneer Flatbreads
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
These are versatile little snacks that can be eaten alone or served as part of a buffet; great for warm summer nights!
You will need
- 1 lb block of paneer (you can also use our plant-based high-protein paneer recipe)
- 7 oz unsweetened yogurt (your choice what kind; plant-based is fine; live cultured is best)
- 1 tomato, thinly sliced
- ½ red onion, thinly sliced
- 2 oz spinach leaves
- 1 tbsp lime juice
- 1 tsp red chili powder
- 4 wholewheat flatbreads
And then the marinade:
- 3 oz spinach
- ½ bulb garlic
- 1 tsp cumin seeds
- 1 tsp coriander seeds
- 1 tsp chili flakes
- ½ tsp MSG or 1 tsp low-sodium salt (MSG being the preferable and healthier option)
- 2 tbsp extra virgin olive oil
- Juice of ½ lime
Method
(we suggest you read everything at least once before doing anything)
1) Blend the marinade ingredients in a blender.
2) Cut the paneer into long cuboid chapes (similar to fish fingers) and put them in a bowl. Pour ⅔ of the marinade over them, and gently mix to coat evenly.
3) Heat a ridged griddle pan, and when hot, add the paneer and cook for 1–2 minutes each side without stirring, jiggling, or doing anything other than turning once per uncooked side.
4) Combine the onion, tomato, spinach leaves, lime choice, and chili powder to make the salad.
5) Add the remaining marinade to the yogurt to make a green dip.
6) Toast your flatbreads under the grill.
5) Assemble, putting the paneer and salad with a spoonful of the dip on the flatbread, and serve:
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- High-Protein Plant-Based Paneer
- Why You’re Probably Not Getting Enough Fiber (And How To Fix It)
- Our Top 5 Spices: How Much Is Enough For Benefits?
- Monosodium Glutamate: Sinless Flavor-Enhancer Or Terrible Health Risk?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
It’s Not A Bloody Trend – by Kat Brown
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This one’s not a clinical book, and the author is not a clinician. However, it’s not just a personal account, either. Kat Brown is an award-winning journalist (with ADHD) and has approached this journalistically.
Not just in terms of investigative journalism, either. Rather, also with her knowledge and understanding of the industry, doing for us some meta-journalism and explaining why the press have gone for many misleading headlines.
Which in this case means for example it’s not newsworthy to say that people have gone undiagnosed and untreated for years and that many continue to go unseen; we know this also about such things as endometriosis, adenomyosis, and PCOS. But some more reactionary headlines will always get attention, e.g. “look at these malingering attention-seekers”.
She also digs into the common comorbidities of various conditions, the differences it makes to friendships, families, relationships, work, self-esteem, parenting, and more.
This isn’t a “how to” book, but there’s a lot of value here if a) you have ADHD, and/or b) you spend any amount of time with someone who does.
Bottom line: if you’d like to understand “what all the fuss is about” in one book, this is the one for ADHD.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: