Can you die from long COVID? The answer is not so simple
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Nearly five years into the pandemic, COVID is feeling less central to our daily lives.
But the virus, SARS-CoV-2, is still around, and for many people the effects of an infection can be long-lasting. When symptoms persist for more than three months after the initial COVID infection, this is generally referred to as long COVID.
In September, Grammy-winning Brazilian musician Sérgio Mendes died aged 83 after reportedly having long COVID.
Australian data show 196 deaths were due to the long-term effects of COVID from the beginning of the pandemic up to the end of July 2023.
In the United States, the Centers for Disease Control and Prevention reported 3,544 long-COVID-related deaths from the start of the pandemic up to the end of June 2022.
The symptoms of long COVID – such as fatigue, shortness of breath and “brain fog” – can be debilitating. But can you die from long COVID? The answer is not so simple.

How could long COVID lead to death?
There’s still a lot we don’t understand about what causes long COVID. A popular theory is that “zombie” virus fragments may linger in the body and cause inflammation even after the virus has gone, resulting in long-term health problems. Recent research suggests a reservoir of SARS-CoV-2 proteins in the blood might explain why some people experience ongoing symptoms.
We know a serious COVID infection can damage multiple organs. For example, severe COVID can lead to permanent lung dysfunction, persistent heart inflammation, neurological damage and long-term kidney disease.
These issues can in some cases lead to death, either immediately or months or years down the track. But is death beyond the acute phase of infection from one of these causes the direct result of COVID, long COVID, or something else? Whether long COVID can directly cause death continues to be a topic of debate.
Of the 3,544 deaths related to long COVID in the US up to June 2022, the most commonly recorded underlying cause was COVID itself (67.5%). This could mean they died as a result of one of the long-term effects of a COVID infection, such as those mentioned above.
COVID infection was followed by heart disease (8.6%), cancer (2.9%), Alzheimer’s disease (2.7%), lung disease (2.5%), diabetes (2%) and stroke (1.8%). Adults aged 75–84 had the highest rate of death related to long COVID (28.8%).
These findings suggest many of these people died “with” long COVID, rather than from the condition. In other words, long COVID may not be a direct driver of death, but rather a contributor, likely exacerbating existing conditions.

‘Cause of death’ is difficult to define
Long COVID is a relatively recent phenomenon, so mortality data for people with this condition are limited.
However, we can draw some insights from the experiences of people with post-viral conditions that have been studied for longer, such as myalgic encephalomyelitis or chronic fatigue syndrome (ME/CFS).
Like long COVID, ME/CFS is a complex condition which can have significant and varied effects on a person’s physical fitness, nutritional status, social engagement, mental health and quality of life.
Some research indicates people with ME/CFS are at increased risk of dying from causes including heart conditions, infections and suicide, that may be triggered or compounded by the debilitating nature of the syndrome.
So what is the emerging data on long COVID telling us about the potential increased risk of death?
Research from 2023 has suggested adults in the US with long COVID were at greater risk of developing heart disease, stroke, lung disease and asthma.
Research has also found long COVID is associated with a higher risk of suicidal ideation (thinking about or planning suicide). This may reflect common symptoms and consequences of long COVID such as sleep problems, fatigue, chronic pain and emotional distress.
But long COVID is more likely to occur in people who have existing health conditions. This makes it challenging to accurately determine how much long COVID contributes to a person’s death.
Research has long revealed reliability issues in cause-of-death reporting, particularly for people with chronic illness.

So what can we conclude?
Ultimately, long COVID is a chronic condition that can significantly affect quality of life, mental wellbeing and overall health.
While long COVID is not usually immediately or directly life-threatening, it’s possible it could exacerbate existing conditions, and play a role in a person’s death in this way.
Importantly, many people with long COVID around the world lack access to appropriate support. We need to develop models of care for the optimal management of people with long COVID with a focus on multidisciplinary care.
Dr Natalie Jovanovski, Vice Chancellor’s Senior Research Fellow in the School of Health and Biomedical Sciences at RMIT University, contributed to this article.
Rose (Shiqi) Luo, Postdoctoral Research Fellow, School of Health and Biomedical Sciences, RMIT University; Catherine Itsiopoulos, Professor and Dean, School of Health and Biomedical Sciences, RMIT University; Kate Anderson, Vice Chancellor’s Senior Research Fellow, RMIT University; Magdalena Plebanski, Professor of Immunology, RMIT University, and Zhen Zheng, Associate Professor, STEM | Health and Biomedical Sciences, RMIT University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Navigating the health-care system is not easy, but you’re not alone.
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Hello, dear reader!
This is my first column for Healthy Debate as a Patient Navigator. This column will be devoted to providing patients with information to help them through their journey with the health-care system and answering your questions.
Here’s a bit about me: I have been a patient partner at The Ottawa Hospital and Ottawa Hospital Research Institute since 2017, and have joined a variety of governance boards that work on patient and caregiver engagement such as the Patient Advisors Network, the Ontario Health East Region Patient and Family Advisory Council and the Equity in Health Systems Lab.
My journey as a patient partner started much before 2017 though. When I was a teenager, I was diagnosed with a cholesteatoma, a rare and chronic disease that causes the development of fatty tumors in the middle ear. I have had multiple surgeries to try to fix it but will need regular follow-ups to monitor whether the tumor returns. Because of this, I also live with an invisible disability since I have essentially become functionally deaf in one ear and often rely on a hearing aid when I navigate the world.
Having undergone three surgeries in my adolescent years, it was my experience undergoing surgery for an acute hand and wrist injury following a jet ski accident as an adult that was the catalyst for my decision to become a patient partner. There was an intriguing contrast between how I was cared for at two different health-care institutions, my age being the deciding factor at which hospital I went to (a children’s hospital or an adult one).
The most memorable example was how, as a teenager or child, you were never left alone before surgery, and nurses and staff took all the time necessary to comfort me and answer my (and my family’s) questions. I also remember how right before putting me to sleep, the whole staff initiated a surgical pause and introduced themselves and explained to me what their role was during my surgery.
None of that happened as an adult. I was left in a hallway while the operating theater was prepared, anxious and alone with staff walking by not even batting an eye. My questions felt like an annoyance to the care team; as soon as I was wheeled onto the operating room table, the anesthetist quickly put me to sleep. I didn’t even have the time to see who else was there.
Now don’t get me wrong: I am incredibly appreciative with the quality of care I received, but it was the everyday interactions with the care teams that I felt could be improved. And so, while I was recovering from that surgery, I looked for a way to help other patients and the hospital improve its care. I discovered the hospital’s patient engagement program, applied, and the rest is history!
Since then, I have worked on a host of patient-centered policy and research projects and fervently advocate that surgical teams adopt a more compassionate approach with patients before and after surgery.
I’d be happy to talk a bit more about my journey if you ask, but with that out of the way … Welcome to our first patient navigator column about patient engagement.
Conceptualizing the continuum of Patient Engagement
In the context of Canadian health care, patient engagement is a multifaceted concept that involves active collaboration between patients, caregivers, health-care providers and researchers. It involves patients and caregivers as active contributors in decision-making processes, health-care services and medical research. Though the concept is not new, the paradigm shift toward patient engagement in Canada started around 2010.
I like to conceptualize the different levels of patient engagement as a measure of the strength of the relationship between patients and their interlocutors – whether it’s a healthcare provider, administrator or researcher – charted against the duration of the engagement or the scope of input required from the patient.
Defining different levels of Patient Engagement
Following the continuum, let’s begin by defining different levels of patient engagement. Bear in mind that these definitions can vary from one organization to another but are useful in generally labelling the level of patient engagement a project has achieved (or wishes to achieve).
Patient involvement: If the strength of the relationship between patients and their interlocutors is minimal and not time consuming or too onerous, then perhaps it can be categorized as patient involvement. This applies to many instances of transactional engagement.
Patient advisory/consulting: Right in the middle of our continuum, patients can find themselves engaging in patient advisory or consulting work, where projects are limited in scope and duration or complexity, and the relationship is not as profound as a partnership.
Patient partnership: The stronger the relationship is between the patient and their interlocutor, and the longer the engagement activity lasts or how much input the patient is providing, the more this situation can be categorized as patient partnership. It is the inverse of patient involvement.
Examples of the different levels of Patient Engagement
Let’s pretend you are accompanying a loved one to an appointment to manage a kidney disease, requiring them to undergo dialysis treatment. We’ll use this scenario to exemplify what label could be used to describe the level of engagement.
Patient involvement: In our case, if your loved one – or you – fills out a satisfaction or feedback survey about your experience in the waiting room and all that needed to be done was to hand it back to the clerk or care team, then, at a basic level, you could likely label this interaction as a form of patient involvement. It can also involve open consultations around a design of a new look and feel for a hospital, or the understandability of a survey or communications product. Interactions with the care team, administrators or researchers are minimal and often transactional.
Patient advisory/consulting: If your loved one was asked for more detailed information about survey results over the course of a few meetings, this could represent patient advisory/consulting. This could mean that patients meet with program administrators and care providers and share their insights on how things can be improved. It essentially involves patients providing advice to health-care institutions from the perspective of patients, their family members and caregivers.
Patient advisors or consultants are often appointed by hospitals or academic institutions to offer insights at multiple stages of health-care delivery and research. They can help pilot an initiative based on that feedback or evaluate whether the new solutions are working. Often patient advisors are engaged in smaller-term individual projects and meet with the project team as regularly as required.
Patient partnership: Going above and beyond patient advisory, if patients have built a trusting relationship with their care team or administrators, they could feel comfortable enough to partner with them and initiate a project of their own. This could be for a project in which they study a different form of treatment to improve patient-centered outcomes (like the time it takes to feel “normal” following a session); it could be working together to identify and remove barriers for other patients that need to access that type of care. These projects are not fulfilled overnight, but require a collaborative, longstanding and trusting relationship between patients and health-care providers, administrators or researchers. It ensures that patients, regardless of severity or chronicity of their illness, can meaningfully contribute their experiences to aid in improving patient care, or develop or implement policies, pilots or research projects from start to finish.
It is leveraging that lived and living experience to its full extent and having the patient partner involved as an equal voice in the decision-making process for a project – over many months, usually – that the engagement could be labeled a partnership.
Last words
The point of this column will be to answer or explore issues or questions related to patient engagement, health communications or even provide some thoughts on how to handle a particular situation.
I would be happy to collect your questions and feedback at any time, which will help inform future columns. Just email me at [email protected] or connect with me on social media (Linked In, X / Twitter).
It’s not easy to navigate our health-care systems, but you are not alone.
This article is republished from healthydebate under a Creative Commons license. Read the original article.
Share This Post
-
Generation M – by Dr. Jessica Shepherd
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Menopause is something that very few people are adequately prepared for despite its predictability, and also something that very many people then neglect to take seriously enough.
Dr. Shepherd encourages a more proactive approach throughout all stages of menopause and beyond; she discusses “the preseason, the main event, and the after-party” (perimenopause, menopause, and postmenopause), which is important, because typically people take up an interest in perimenopause, are treating it like a marathon by menopause, and when it comes to postmenopause, it’s easy to think “well, that’s behind me now”, and it’s not, because untreated menopause will continue to have (mostly deleterious) cumulative effects until death.
As for HRT, there’s a chapter on that of course, going into quite some detail. There is also plenty of attention given to popular concerns such as managing weight changes and libido changes, as well as oft-neglected topics such as brain changes, as well as things considered more cosmetic but that can have a big impact on mental health, such as skin and hair.
The style throughout is pop-science; friendly without skimping on detail and including plenty of good science.
Bottom line: if you’d like a fairly comprehensive overview of the changes that occur from perimenopause all the way to menopause and well beyond, then this is a great book for that.
Click here to check out Generation M, and live well at every stage of life!
Share This Post
-
Blood-Brain Barrier Breach Blamed For Brain-Fog
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Move Over, Leaky Gut. Now It’s A Leaky Brain.
…which is not a headline that promises good news, and indeed, the only good news about this currently is “now we know another thing that’s happening, and thus can work towards a treatment for it”.
Back in February (most popular media outlets did not rush to publish this, as it rather goes against the narrative of “remember when COVID was a thing?” as though the numbers haven’t risen since the state of emergency was declared over), a team of Irish researchers made a discovery:
❝For the first time, we have been able to show that leaky blood vessels in the human brain, in tandem with a hyperactive immune system may be the key drivers of brain fog associated with long covid❞
~ Dr. Matthew Campbell (one of the researchers)
Let’s break that down a little, borrowing some context from the paper itself:
- the leaky blood vessels are breaching the blood-brain-barrier
- that’s a big deal, because that barrier is our only filter between our brain and Things That Definitely Should Not Go In The Brain™
- a hyperactive immune system can also be described as chronic inflammation
- in this case, that includes chronic neuroinflammation which, yes, is also a major driver of dementia
You may be wondering what COVID has to do with this, and well:
- these blood-brain-barrier breaches were very significantly associated (in lay terms: correlated, but correlated is only really used as an absolute in write-ups) with either acute COVID infection, or Long Covid.
- checking this in vitro, exposure of brain endothelial cells to serum from patients with Long Covid induced the same expression of inflammatory markers.
How important is this?
As another researcher (not to mention: professor of neurology and head of the school of medicine at Trinity) put it:
❝The findings will now likely change the landscape of how we understand and treat post-viral neurological conditions.
It also confirms that the neurological symptoms of long covid are measurable with real and demonstrable metabolic and vascular changes in the brain.❞
~ Dr. Colin Doherty (see mini-bio above)
You can read a pop-science article about this here:
Irish researchers discover underlying cause of “brain fog” linked with long covid
…and you can read the paper in full here:
Want to stay safe?
Beyond the obvious “get protected when offered boosters/updates” (see also: The Truth About Vaccines), other good practices include the same things most people were doing when the pandemic was big news, especially avoiding enclosed densely-populated places, washing hands frequently, and looking after your immune system. For that latter, see also:
Beyond Supplements: The Real Immune-Boosters!
Take care!
Share This Post
- the leaky blood vessels are breaching the blood-brain-barrier
Related Posts
-
Is Vitamin C Worth The Hype? (Doctorly Investigates)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Double Board-Certified Dermatologists Dr. Muneeb Shah & Dr. Luke Maxfield weigh in on vitamin C; is it worth the hype?
Yes it is, but…
There are some caveats, for example:
- It’s best to apply vitamin C on clean, dry skin and let it set before layering other products.
- Avoid mixing with oxidants like benzoyl peroxide (cancels out antioxidant effects).
- Avoid combining with copper (may negate brightening benefits).
- Do not use with hypochlorous acid (oxidative reactions cancel out benefits).
- Be cautious with retinol due to irritation risks.
However, used correctly, it does give very worthy benefits, and they recommend:
- Morning use: acts as an antioxidant, pairs well with sunscreen for better protection from sun and environmental damage.
- Night use: maximizes functions like improving tone, collagen production, texture, and reducing wrinkles.
That’s not to say that at night it stops being an antioxidant or during the day it isn’t critical for collagen synthesis, but it is to say: because of the different things our bodies typically encounter and/or do during the day or night, those are the best times to get the most out of those benefits.
They also review some popular products; here are some notes on their comments about them:
- Skinceuticals C E Ferulic: research-backed, $180, effective but potentially irritating.
- Skinceuticals Phloretin CF: includes 0.5% salicylic acid, good for acne-prone skin.
- Dermatology Vitamin C E Ferulic: relatively more affordable ($70), fragrance-free, includes peptides and ceramides.
- Drunk Elephant C-Firma: powder-to-serum formula, sued for patent infringement.
- Paula’s Choice C15 Booster: reformulated, fragrance-free, similar to Skinceuticals.
- Neutrogena Vitamin C Capsules: stabilized 20% ascorbic acid, single-use, travel-friendly.
- La Roche-Posay Vitamin C Serum: contains fragrance and alcohol, not ideal for sensitive skin.
- Matter of Fact Vitamin C Serum: includes ascorbic acid and ferulic acid, oily texture for dry skin.
- Medik8 Super C Ferulic: stable 30% ethyl ascorbic acid, lightweight texture.
- Naturium Vitamin C Complex: multi-form Vitamin C with niacinamide, alpha arbutin, and turmeric.
- Timeless Vitamin C Serum: affordable ($20), 20% ascorbic acid with E and ferulic acid.
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like:
More Than Skin-Deep: Six Ways To Eat For Healthier Skin ← this one’s about a lot more than just vitamin C 😎
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Gut-Healthy Tacos
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Full of prebiotics and probiotics, healthy fats, colorful salad boasting vitamins and minerals aplenty, and of course satisfying protein too, these tacos are also boasting generous flavors to keep you coming back for more…
You will need
- 24 sardines—canned is fine (if vegetarian/vegan, substitute tempeh and season generously; marinade if you have time)
- 12 small wholewheat tortillas
- 1 14oz/400g can black beans, drained
- 1 ripe avocado, stoned and cut into small chunks
- 1 red onion, thinly sliced
- 1 little gem lettuce, shredded
- 12 cherry tomatoes, halved
- 1 bulb garlic, crushed
- 1 lemon, sliced
- 4 tbsp plain unsweetened yogurt (your choice what kind, but something with a live culture is best)
- 3oz pickled jalapeños, roughly chopped
- 1oz cilantro (or substitute parsley if you have the cilantro-tastes-like-soap gene), finely chopped
- 1 tbsp extra virgin olive oil
- 2 tsp black pepper
- 1 tsp smoked paprika
- Juice of 1 lime
- Optional: Tabasco sauce, or similar hot sauce
Method
(we suggest you read everything at least once before doing anything)
1) Preheat your oven to a low temperature; 200℉ or just under 100℃ is fine
2) Place the lemon slices on top of the sardines on top of foil on a baking tray; you want the foil to be twice as much as you’d expect to need, because now you’re going to fold it over and make a sort of sealed envelope. You could use a dish with a lid yes, but this way is better because there’s going to be less air inside. Upturn the edges of the envelope slightly so that juices won’t run out, and make sure the foil is imperfectly sealed so a little steam can escape but not much at a time. This will ensure it doesn’t dry out, while also ensuring your house doesn’t smell of fish. Put all this into the oven on a middle shelf.
3) Mix the lime juice with the onion in a bowl, and add the avocado and tomatoes, mixing gently. Add half the cilantro, and set aside.
4) Put the black beans in a sieve and pour boiling water over them to refresh and slightly warm them. Tip them into a bowl and add the olive oil, black pepper, and paprika. Mix thoroughly with a fork, and no need to be gentle this time; in fact, deliberately break the beans a little in this case.
5) Mix the yogurt, jalapeños, garlic, and remaining cilantro in a small bowl.
6) Get the warmed sardines from the oven; discard the lemon slices.
7) Assemble! We recommend the order: tortilla, lettuce, fish (2 per taco), black bean mixture, salad mixture, garlic jalapeño yogurt mixture. You can also add a splash of the hot sauce per your preference, or if catering for more people, let people add their own.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- We Are Such Stuff As Fish Are Made Of
- Level-Up Your Fiber Intake! (Without Difficulty Or Discomfort)
- Making Friends With Your Gut (You Can Thank Us Later)
- Our Top 5 Spices: How Much Is Enough For Benefits?
- Enjoy Pungent Polyphenols For Your Heart & Brain
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
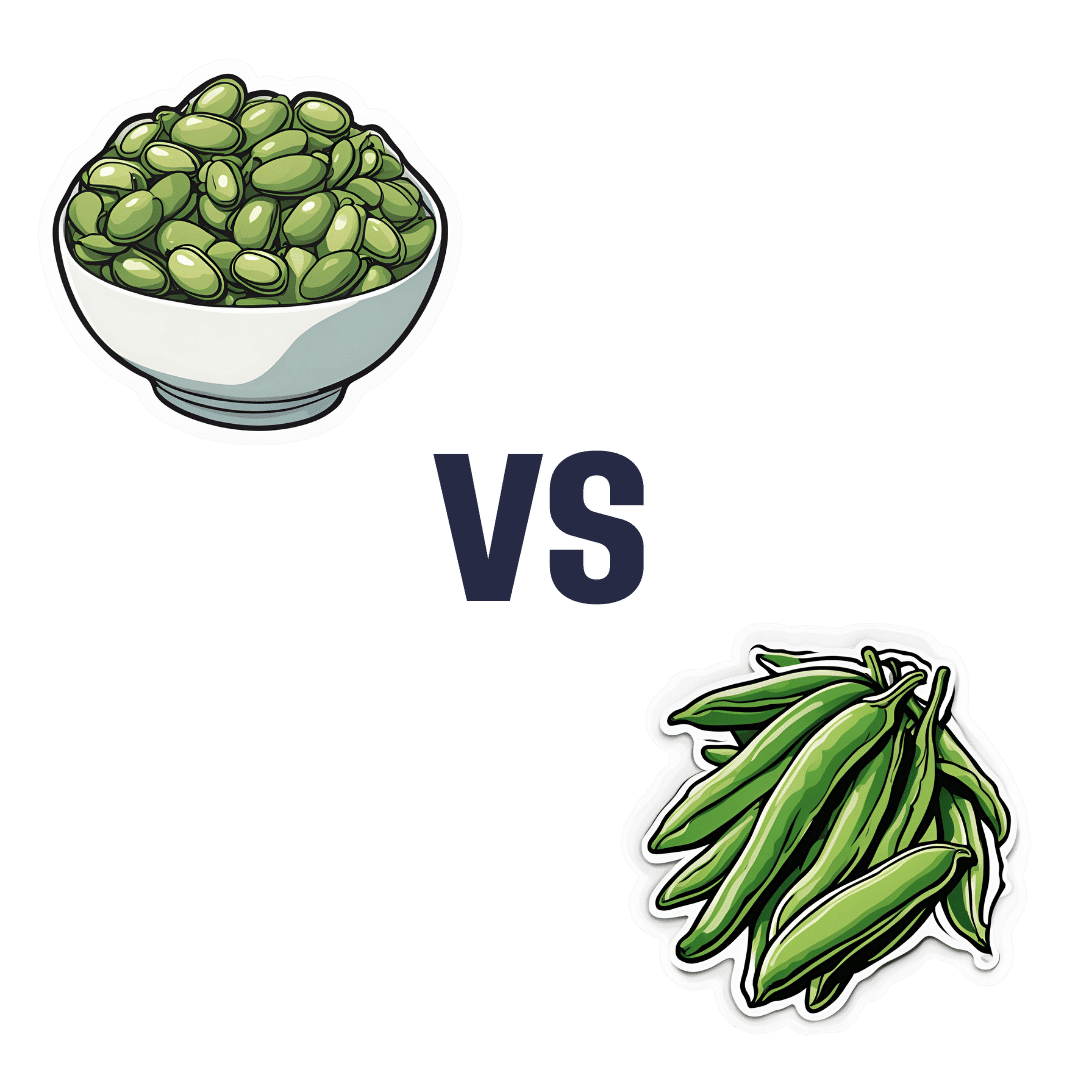
Broad Beans vs Green Beans – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing broad beans to green beans, we picked the broad.
Why?
It’s quite a straightforward one today:
In terms of macros, broad beans have 2.5x the protein, and slightly more fiber and carbs, so we pick the broad beans as the more nutrient-dense option here.
In the category of vitamins, broad beans have more of vitamins B1, B3, B9, and C, while green beans have more of vitamins A and B6 (with comparable margins of difference for both beans’ winning vitamins), so another win for broad beans, based on the 4:2 numerical advantage.
When it comes to minerals, broad beans have more copper, iron, magnesium, phosphorus, potassium, and selenium, while green beans have more calcium and manganese. Again, comparable mostly margins of difference (except for broad beans bing 5x richer in selenium, which is a bit of an outlier, but it’s not because broad beans are an amazing source of selenium, but rather, that green beans have only a tiny amount), so it’s a clear 7:2 win for broad beans.
Adding up the three wins for broad beans makes an overall win for them, but by all means, enjoy either or both; diversity is good!
Want to learn more?
You might like to read:
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: