Buffed-Up Buffalo Cauliflower
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is a tasty snack that also more protein than you’d think, because of the garbanzo bean flour. It also has plenty of health-giving spices, as well as blood-sugar-balancing vinegar, no added sugar, and very little salt.
You will need
- 1 medium head of cauliflower, cut into florets
- ½ cup garbanzo bean flour
- ½ cup water
- ⅓ cup hot sauce (we recommend a low-sugar kind; Nando’s hot sauce is good for this if available where you are, as it has no added sugar and its main ingredient by volume is vinegar, which is good for balancing blood sugars)
- 2 tbsp extra virgin olive oil, plus more for the pan
- 2 tsp garlic powder
- 2 tsp nutritional yeast
- 2 tsp black pepper, freshly ground
- 1 tsp smoked paprika
- ½ tsp MSG, or 1 tsp low sodium salt
For the ranch sauce:
- ½ cup raw sunflower seeds
- ⅓ cup water
- ⅓ cup milk (plant milk being healthiest if you choose one that’s unsweetened)
- 2 tbsp apple cider vinegar
- 2 tbsp extra virgin olive oil
- 1 tsp onion powder
- 1 tsp dried thyme
- 1 tsp dried oregano
- 1 tsp dried dill
- ½ tsp MSG, or 1 tsp low sodium salt
Method
(we suggest you read everything at least once before doing anything)
1) Preheat the oven to 400℉/200℃.
2) Blend the ranch sauce ingredients until smooth, and set aside.
3) Mix the buffalo cauliflower ingredients except for the cauliflower, in a big bowl.
4) Add the cauliflower to the big bowl, mixing well to coat evenly.
5) Bake the buffalo cauliflower florets on a baking tray lined with baking paper, for about 25 minutes, turning gently if it seems they are at risk of cooking unevenly.
6) Serve hot, with the sunflower ranch on the side!

Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- An Apple (Cider Vinegar) A Day…
- 10 Ways To Balance Blood Sugars
- Our Top 5 Spices: How Much Is Enough For Benefits?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Thinner Leaner Stronger – by Michael Matthews
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
First, the elephant in the training room: this book does assume that you want to be thinner, leaner, and stronger. This is the companion book, written for women, to “Bigger, Stronger, Leaner”, which was written for men. Statistically, these assumptions are reasonable, even if the generalizations are imperfect. Also, this reviewer has a gripe with anything selling “thinner”. Leaner was already sufficient, and “stronger” is the key element here, so “thinner” is just marketing, and marketing something that’s often not unhealthy, to sell a book that’s actually full of good advice for building a healthy body.
In other words: don’t judge a book by the cover, however eyeroll-worthy it may be.
The book is broadly aimed at middle-aged readers, but boasts equal worth for young and old alike. If there’s something Matthews knows how to do well in his writing, it’s hedging his bets.
As for what’s in the book: it’s diet and exercise advice, aimed at long-term implementation (i.e. not a crash course, but a lifestyle change), for maximum body composition change results while not doing anything silly (like many extreme short-term courses do) and not compromising other aspects of one’s health, while also not taking up an inordinate amount of time.
The dietary advice is sensible, broadly consistent with what we’d advise here, and/but if you want to maximise your body composition change results, you’re going to need a pocket calculator (or be better than this writer is at mental arithmetic).
The exercise advice is detailed, and a lot more specific than “lift things”; there are programs of specifically how many sets and reps and so forth, and when to increase the weights and when not to.
A strength of this book is that it explains why all those numbers are what they are, instead of just expecting the reader to take on faith that the best for a given exercise is (for example) 3 sets of 8–10 reps of 70–75% of one’s single-rep max for that exercise. Because without the explanation, those numbers would seem very arbitrary indeed, and that wouldn’t help anyone stick with the program. And so on, for any advice he gives.
The style is… A little flashy for this reader’s taste, a little salesy (and yes he does try to upsell to his personal coaching, but really, anything you need is in the book already), but when it comes down to it, all that gym-boy bravado doesn’t take away from the fact his advice is sound and helpful.
Bottom line: if you would like your body to be the three things mentioned in the title, this book can certainly help you get there.
Click here to check out Thinner Leaner Stronger, and become thinner, leaner, stronger!
Share This Post
-
Paris in spring, Bali in winter. How ‘bucket lists’ help cancer patients handle life and death
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In the 2007 film The Bucket List Jack Nicholson and Morgan Freeman play two main characters who respond to their terminal cancer diagnoses by rejecting experimental treatment. Instead, they go on a range of energetic, overseas escapades.
Since then, the term “bucket list” – a list of experiences or achievements to complete before you “kick the bucket” or die – has become common.
You can read articles listing the seven cities you must visit before you die or the 100 Australian bucket-list travel experiences. https://www.youtube.com/embed/UvdTpywTmQg?wmode=transparent&start=0
But there is a more serious side to the idea behind bucket lists. One of the key forms of suffering at the end of life is regret for things left unsaid or undone. So bucket lists can serve as a form of insurance against this potential regret.
The bucket-list search for adventure, memories and meaning takes on a life of its own with a diagnosis of life-limiting illness.
In a study published this week, we spoke to 54 people living with cancer, and 28 of their friends and family. For many, a key bucket list item was travel.
Why is travel so important?
There are lots of reasons why travel plays such a central role in our ideas about a “life well-lived”. Travel is often linked to important life transitions: the youthful gap year, the journey to self-discovery in the 2010 film Eat Pray Love, or the popular figure of the “grey nomad”.
The significance of travel is not merely in the destination, nor even in the journey. For many people, planning the travel is just as important. A cancer diagnosis affects people’s sense of control over their future, throwing into question their ability to write their own life story or plan their travel dreams.
Mark, the recently retired husband of a woman with cancer, told us about their stalled travel plans:
We’re just in that part of our lives where we were going to jump in the caravan and do the big trip and all this sort of thing, and now [our plans are] on blocks in the shed.
For others, a cancer diagnosis brought an urgent need to “tick things off” their bucket list. Asha, a woman living with breast cancer, told us she’d always been driven to “get things done” but the cancer diagnosis made this worse:
So, I had to do all the travel, I had to empty my bucket list now, which has kind of driven my partner round the bend.
People’s travel dreams ranged from whale watching in Queensland to seeing polar bears in the Arctic, and from driving a caravan across the Nullarbor Plain to skiing in Switzerland.
Whale watching in Queensland was on one person’s bucket list. Uwe Bergwitz/Shutterstock Nadia, who was 38 years old when we spoke to her, said travelling with her family had made important memories and given her a sense of vitality, despite her health struggles. She told us how being diagnosed with cancer had given her the chance to live her life at a younger age, rather than waiting for retirement:
In the last three years, I think I’ve lived more than a lot of 80-year-olds.
But travel is expensive
Of course, travel is expensive. It’s not by chance Nicholson’s character in The Bucket List is a billionaire.
Some people we spoke to had emptied their savings, assuming they would no longer need to provide for aged care or retirement. Others had used insurance payouts or charity to make their bucket-list dreams come true.
But not everyone can do this. Jim, a 60-year-old whose wife had been diagnosed with cancer, told us:
We’ve actually bought a new car and [been] talking about getting a new caravan […] But I’ve got to work. It’d be nice if there was a little money tree out the back but never mind.
Not everyone’s bucket list items were expensive. Some chose to spend more time with loved ones, take up a new hobby or get a pet.
Our study showed making plans to tick items off a list can give people a sense of self-determination and hope for the future. It was a way of exerting control in the face of an illness that can leave people feeling powerless. Asha said:
This disease is not going to control me. I am not going to sit still and do nothing. I want to go travel.
Something we ‘ought’ to do?
Bucket lists are also a symptom of a broader culture that emphasises conspicuous consumption and productivity, even into the end of life.
Indeed, people told us travelling could be exhausting, expensive and stressful, especially when they’re also living with the symptoms and side effects of treatment. Nevertheless, they felt travel was something they “ought” to do.
Travel can be deeply meaningful, as our study found. But a life well-lived need not be extravagant or adventurous. Finding what is meaningful is a deeply personal journey.
Names of study participants mentioned in this article are pseudonyms.
Leah Williams Veazey, ARC DECRA Research Fellow, University of Sydney; Alex Broom, Professor of Sociology & Director, Sydney Centre for Healthy Societies, University of Sydney, and Katherine Kenny, ARC DECRA Senior Research Fellow, University of Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
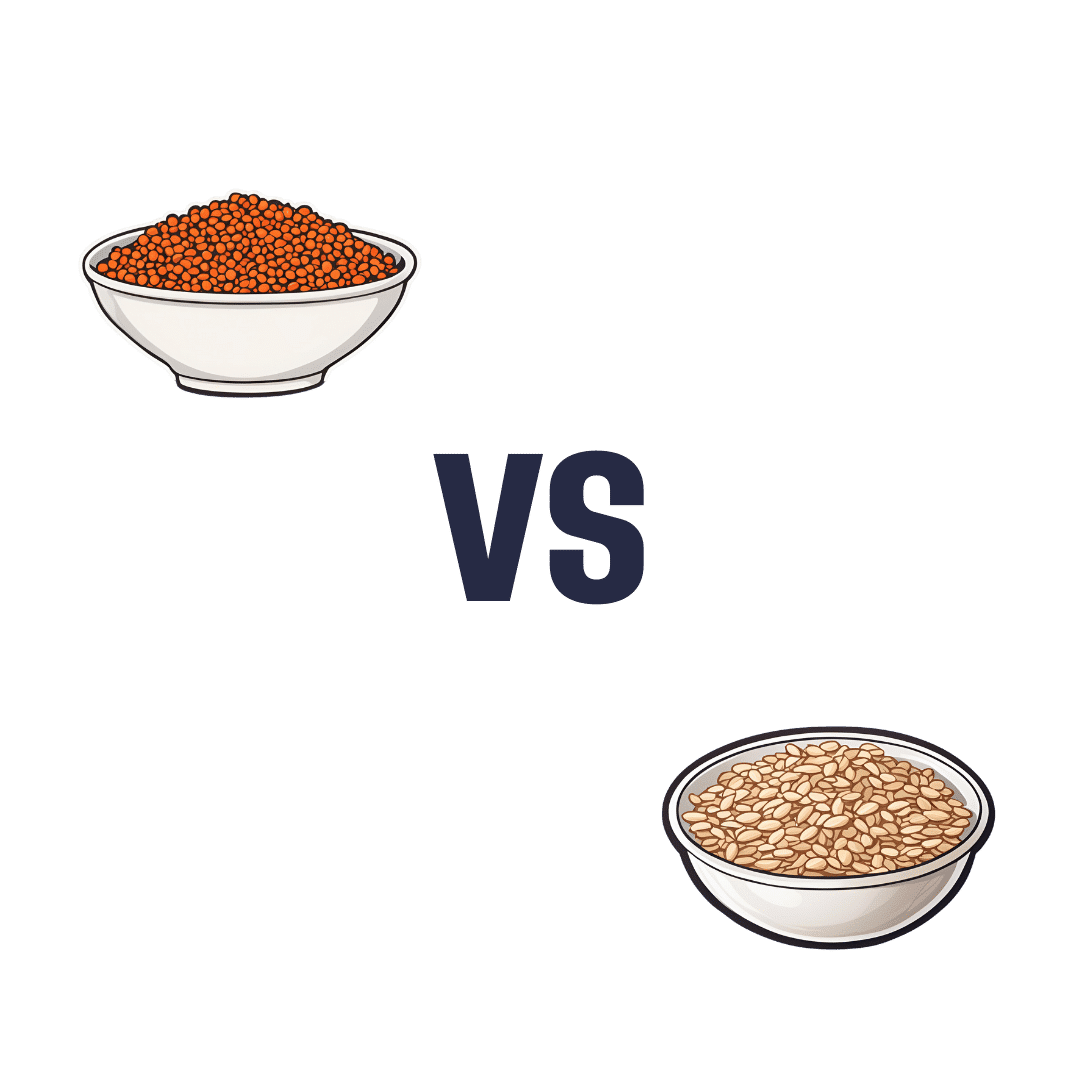
Red Lentils vs Oats – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing red lentils to oats, we picked the oats.
Why?
In terms of macros, oats have more protein, carbs, fiber, and even a little fat—mostly healthy mono- and polyunsaturated fats, thus making them the more nutritionally dense. That said, red lentils have the lower glycemic index, (low GI compared to oats’ medium GI) which offsets that, so we’ll call this category a tie.
In the category of vitamins, red lentils have more of vitamins B6, B9, and choline, while oats have more of vitamins B1, B2, and B5. Another tie!
When it comes to minerals, however, we have a tiebreaker category: red lentils have more selenium, while oats have more calcium, copper, iron, magnesium, manganese, phosphorus, potassium, and zinc. An easy win for oats this time!
So, thanks to the minerals, oats are the clear winner in total. But by all means, enjoy either or both; diversity is good!
Want to learn more?
You might like to read:
The Best Kind Of Fiber For Overall Health? ← it’s β-glucan, the kind find in oats!
Enjoy!
Share This Post
Related Posts
-
Cordyceps: Friend Or Foe?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Cordyceps: friend or foe?
Cordyceps is a famously frightening fungus. It’s the one responsible for “zombie ants” and other zombie creatures, and it’s the basis for the existential threat to humanity in the TV show The Last of Us.
It’s a parasitic fungus that controls the central and peripheral nervous systems of its host, slowly replacing the host’s body, as well as growing distinctive spines that erupt out of the host’s body. Taking over motor functions, it compels the host to do two main things, which are to eat more food, and climb to a position that will be good to release spores from.
Fortunately, none of that matters to humans. Cordyceps does not (unlike in the TV show) affect humans that way.
What does Cordyceps do in humans?
Cordyceps (in various strains) is enjoyed as a health supplement, based on a long history of use in Traditional Chinese Medicine, and nowadays it’s coming under a scientific spotlight too.
The main health claims for it are:
- Against inflammation
- Against aging
- Against cancer
- For blood sugar management
- For heart health
- For exercise performance
Sounds great! What does the science say?
There’s a lot more science for the first three (which are all closely related to each other, and often overlapping in mechanism and effect).
So let’s take a look:
Against inflammation
The science looks promising for this, but studies so far have either been in vitro (cell cultures in petri dishes), or else murine in vivo (mouse studies), for example:
- Anti-inflammatory effects of Cordyceps mycelium in murine macrophages
- Cordyceps sinensis as an immunomodulatory agent
- Immunomodulatory functions of extracts from Cordyceps cicadae
- Cordyceps pruinosa inhibits in vitro and in vivo inflammatory mediators
In summary: we can see that it has anti-inflammatory properties for mice and in the lab; we’d love to see the results of studies done on humans, though. Also, while it has anti-inflammatory properties, it performed less well than commonly-prescribed anti-inflammatory drugs, for example:
❝C. militaris can modulate airway inflammation in asthma, but it is less effective than prednisolone or montelukast.❞
Against aging
Because examining the anti-aging effects of a substance requires measuring lifespans and repeating the experiment, anti-aging studies do not tend to be done on humans, because they would take lifetimes to perform. To this end, it’s inconvenient, but not a criticism of Cordyceps, that studies have been either mouse studies (short lifespan, mammals like us) or fruit fly studies (very short lifespan, genetically surprisingly similar to us).
The studies have had positive results, with typical lifespan extensions of 15–20%:
- The lifespan-extending effect of Cordyceps sinensis in normal mice
- Cordyceps sinensis oral liquid prolongs the lifespan of the fruit fly, Drosophila melanogaster
- Anti-aging activity of polysaccharides from Cordyceps militaris
- Anti-aging effect of Cordyceps sinensis extract
Against cancer
Once again, the studies here have been in vitro, or murine in vivo. They do look good though:
In vitro (human cell cultures in a lab):
In vivo (mouse studies):
Summary of these is: Cordyceps quite reliably inhibits tumor growth in vitro (human cell cultures) and in vivo (mouse studies). However, trials in human cancer patients are so far conspicuous by their absence.
For blood sugar management
Cordyceps appears to mimic the action of insulin, without triggering insulin sensitivity. For example:
The anti-hyperglycemic activity of the fruiting body of Cordyceps in diabetic rats
There were some other rat/mouse studies with similar results. No studies in humans yet.
For heart health
Cordyceps contains adenosine. You may remember that caffeine owes part of its stimulant effect to blocking adenosine, the hormone that makes us feel sleepy. So in this way, Cordyceps partially does the opposite of what caffeine does, and may be useful against arrhythmia:
Cardiovascular protection of Cordyceps sinensis act partially via adenosine receptors
For exercise performance
A small (30 elderly participants) study found that Cordyceps supplementation improved VO2 max by 7% over the course of six weeks:
However, another small study (22 young athletes) failed to reproduce those results:
Cordyceps Sinensis supplementation does not improve endurance exercise performance
In summary…
Cordyceps almost certainly has anti-inflammation, anti-aging, and anti-cancer benefits.
Cordyceps may have other benefits too, but the evidence is thinner on the ground for those, so far.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
PTSD, But, Well…. Complex.
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
PTSD is typically associated with military veterans, for example, or sexual assault survivors. There was a clear, indisputable, Bad Thing™ that was experienced, and it left a psychological scar. When something happens to remind us of that—say, there are fireworks, or somebody touches us a certain way—it’ll trigger an immediate strong response of some kind.
These days the word “triggered” has been popularly misappropriated to mean any adverse emotional reaction, often to something trivial.
But, not all trauma is so clear. If PTSD refers to the result of that one time you were smashed with a sledgehammer, C-PTSD (Complex PTSD) refers to the result of having been hit with a rolled-up newspaper every few days for fifteen years, say.
This might have been…
- childhood emotional neglect
- a parent with a hair-trigger temper
- bullying at school
- extended financial hardship as a young adult
- “just” being told or shown all too often that your best was never good enough
- the persistent threat (real or imagined) of doom of some kind
- the often-reinforced idea that you might lose everything at any moment
If you’re reading this list and thinking “that’s just life though”, you might be in the estimated 1 in 5 people with (often undiagnosed) C-PTSD.
How About You? Take The (5mins) Test Here
Now, we at 10almonds are not doctors or therapists and even if we were, we certainly wouldn’t try to diagnose from afar. But, even if there’s only a partial match, sometimes the same advice can help.
So what are the symptoms of C-PTSD?
- A feeling that nothing is safe; we might suddenly lose what we have gained
- The body keeps the score… And it shows. We may have trouble relaxing, an aversion to exercise for reasons that don’t really add up, or an aversion to being touched.
- Trouble sleeping, born of nagging sense that to sleep is to be vulnerable to attack, and/or lazy, and/or negligent of our duties
- Poor self-image, about our body and/or about ourself as a person.
- We’re often drawn to highly unavailable people—or we are the highly unavailable person to which our complementary C-PTSD sufferers are attracted.
- We are prone to feelings of rage. Whether we keep a calm lid on it or lose our temper, we know it’s there. We’re angry at the world and at ourselves.
- We are not quick to trust—we may go through the motions of showing trust, but we’re already half-expecting that trust to have been misplaced.
- “Hell is other people” has become such a rule of life that we may tend to cloister ourselves away from company.
- We may try to order our environment around us as a matter of safety, and be easily perturbed by sudden changes being imposed on us, even if ostensibly quite minor or harmless.
- In a bid to try to find safety, we may throw ourselves into work—whatever that is for us. It could be literally our job, or passion projects, or our family, or community, and in and of itself that’s great! But the motivation is more of an attempt to distract ourselves from The Horrors™.
“Alright, I scored more of those than I care to admit. What now?”
A lot of the answer lies in first acknowledging to yourself what happened, to make you feel the way you do now. If you, for example, have an abject hatred of Christmas, what were your childhood Christmases like? If you fear losing money that you’ve accumulated, what underpins that fear? It could be something that directly happened to you, but it also could just be repeated messages you received from your parents, for example.
It could even be that you had superficially an idyllic perfect childhood. Health, wealth, security, a loving family… and simply a chemical imbalance in your brain made it a special kind of Hell for you that nobody understood, and perhaps you didn’t either.
Unfortunately, a difficult task now lies ahead: giving love, understanding, compassion, and reassurance to the person for whom you may have the most contempt in the world: yourself.
If you’d like some help with that, here are some resources:
ComplexTrauma.org (a lot of very good free resources, with no need for interaction)
CPTSD Foundation (mostly paid courses and the like)
Some final words about healing…
- You are in fact amazing,
- You can do it, and
- You deserve it.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Pistachios vs Cashews – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing pistachios to cashews, we picked the pistachios.
Why?
In terms of macros, both are great sources of protein and healthy fats, and considered head-to-head:
- pistachios have slightly more protein, but it’s close
- pistachios have slightly more (health) fat, but it’s close
- cashews have slightly more carbs, but it’s close
- pistachios have a lot more fiber (more than 3x more!)
All in all, both have a good macro balance, but pistachios win easily on account of the fiber, as well as the slight edge for protein and fats.
When it comes to vitamins, pistachios have more of vitamins A, B1, B2, B3, B6, B9, C, & E.
Cashews do have more vitamin B5, also called pantothenic acid, pantothenic literally meaning “from everywhere”. Guess what’s not a common deficiency to have!
So pistachios win easily on vitamins, too.
In the category of minerals, things are more balanced, though cashews have a slight edge. Pistachios have more notably more calcium and potassium, while cashews have notably more selenium, zinc, and magnesium.
Both of these nuts have anti-inflammatory, anti-diabetic, and anti-cancer benefits, often from different phytochemicals, but with similar levels of usefulness.
Taking everything into account, however, one nut comes out in the clear lead, mostly due to its much higher fiber content and better vitamin profile, and that’s the pistachios.
Want to learn more?
Check out:
Why You Should Diversify Your Nuts
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: