Behind Book Recommendations
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day!
Each Thursday, we respond to subscriber questions and requests! If it’s something small, we’ll answer it directly; if it’s something bigger, we’ll do a main feature in a follow-up day instead!
So, no question/request to big or small; they’ll just get sorted accordingly
Remember, you can always hit reply to any of our emails, or use the handy feedback widget at the bottom. We always look forward to hearing from you!
Q: What’s the process behind the books you recommend? You seem to have a limitless stream of recommendations
We do our best!
The books we recommend are books that…
- are on Amazon—it makes things tidy, consistent, and accessible. And if you end up buying one of the books, we get a small affiliate commission*.
- we have read—we would say “obviously”, but you might be surprised how many people write about books without having read them.
- pertain in at least large part to health and/or productivity.
- are written by humans—bookish people (and especially Kindle Unlimited users) may have noticed lately that there are a lot of low quality AI-written books flooding the market, sometimes with paid 5-star reviews to bolster them. It’s frustrating, but we can tell the difference and screen those out.
- are of a certain level of quality. They don’t have to be “top 5 desert-island books”, because well, there’s one every day and the days keep coming. But they do have to genuinely deliver the value that we describe, and merit a sincere recommendation.
- are varied—we try to not give a run of “samey” books one after another. We will sometimes review a book that covers a topic another previously-reviewed book did, but it must have something about it that makes it different. It may be a different angle or a different writing style, but it needs something to set it apart.
*this is from Amazon and isn’t product-specific, so this is not affecting our choice of what books to review at all—just that they will be books that are available on Amazon.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Next-Level Headache Hacks
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A Muscle With A Lot Of Therapeutic Value
First, a quick anatomy primer, so that the rest makes sense. We’re going to be talking about your sternocleidomastoid (SCM) muscle today.
To find it, there are two easy ways:
- look in a mirror, turn your head to one side and it’ll stick out on the opposite side of your neck
- look at this diagram
(we’re going to talk about it in the singular, but you have one on each side)
This muscle is interesting for very many reasons, but what we’re going to focus on today is that massaging/stretching it (correctly!) can benefit several things that are right next to it and/or behind it, namely:
- The tenth cranial nerve
- The eleventh cranial nerve
- The carotid artery
Why do we care about these?
Well, we would die quickly without the first and last of those. However, more practically, massaging each has benefits:
The tenth cranial nerve
This one is also known by its superhero alter-ego name:
The Vagus Nerve (And How You Can Make Use Of It)
The eleventh cranial nerve
This one’s not nearly so critical to life, but it does facilitate most of the motor functions in that general part of the body—including some mechanics of speech production, and maintaining posture of the shoulders/neck/head (which in turn strongly affects presence/absence of certain kinds of headaches).
The carotid artery
We suspect you know what this one does already; it supplies the brain (and the rest of your head, for that matter) with oxygenated blood.
What is useful to know today, is that it can be massaged, via the SCM, in a way that brings about a gentler version of this “one weird trick” to cure a lot of kinds of headaches:
Curing Headaches At Home With Actual Science
How (And Why) To Massage Your SCM
…to relieve many kinds of headache, migraine, eye-ache, and tension or pain the jaw. It’s not a magical cure all so this comes with no promises, but it can and will help with a lot of things.
In few words: turn your ahead away from the side where it hurts (if both, just pick one and then repeat for the other side), and slightly downwards. When your SCM sticks out a bit on the other side, gently pinch and rub it, working from the bottom to the top.
If you prefer videos, here is a demonstration:
How (And Why) To Stretch Your SCM
The above already includes a little stretch, but you can stretch it in a way that specifically stimulates your vagus nerve (this is good for many things).
In few words: stand (or sit) up straight, and interlace your fingers together. Put your hands on the back of your neck, thumbs-downwards, and (keeping your face forward) look to one side with your eyes only, and hold that until you feel the urge to yawn (it’ll probably take between about 3 seconds and 30 seconds). Then repeat on the other side.
If you prefer videos, this one is a very slight variation of what we just described but works the same way:
Take care!
Share This Post
-
5 Stretches To Relieve The Pain From Sitting & Poor Posture
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Sitting is not good for the health, yes often it’s a necessity of modern life, especially if driving. To make things worse, it can often be difficult to remember to maintain good posture the rest of the time, if it’s not a habit. So, while reducing sitting and improving posture are both very good things to do, here are 5 stretches to mitigate the damage meanwhile:
Daily doses:
These are best done at a rate of 2–3 sets daily:
Cat-Cow Stretch:
- Benefits: eases spinal tension, boosts flexibility, improves posture.
- How to: start on all fours, alternate between arching and rounding your back while syncing with your breath (10-15 times).
Butterfly Stretch:
- Benefits: loosens tight hips, improves lower back flexibility, and enhances mobility for activities like squats.
- How to: sit with soles of feet together, let knees fall toward the floor, lean forward slightly, and hold for 30 seconds to 1 minute.
Supine Twist:
- Benefits: unlocks the spine, relieves post-workout tension, and relaxes the shoulders and hips.
- How to: lie on your back, bend knees, twist to one side while keeping shoulders grounded, and hold for 30 seconds to 1 minute per side.
Calf Stretch:
- Benefits: improves ankle mobility, loosens tight calves, and prevents injuries like Achilles tendinitis.
- How to: stand facing a wall, extend one leg back with the heel on the ground, lean into the stretch, or use a step for deeper stretches. Hold for 30 seconds to 1 minute per leg.
Child’s Pose:
- Benefits: decompresses the spine, relaxes hips, and relieves tension in back and thighs.
- How to: start on hands and knees, sit back onto your heels, stretch arms forward, and rest forehead on the mat. Hold for 30 seconds to 1 minute.
For more on each of these, plus visual demonstrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like:
10 Tips To Reduce Morning Pain & Stiffness With Arthritis
Take care!
Share This Post
-
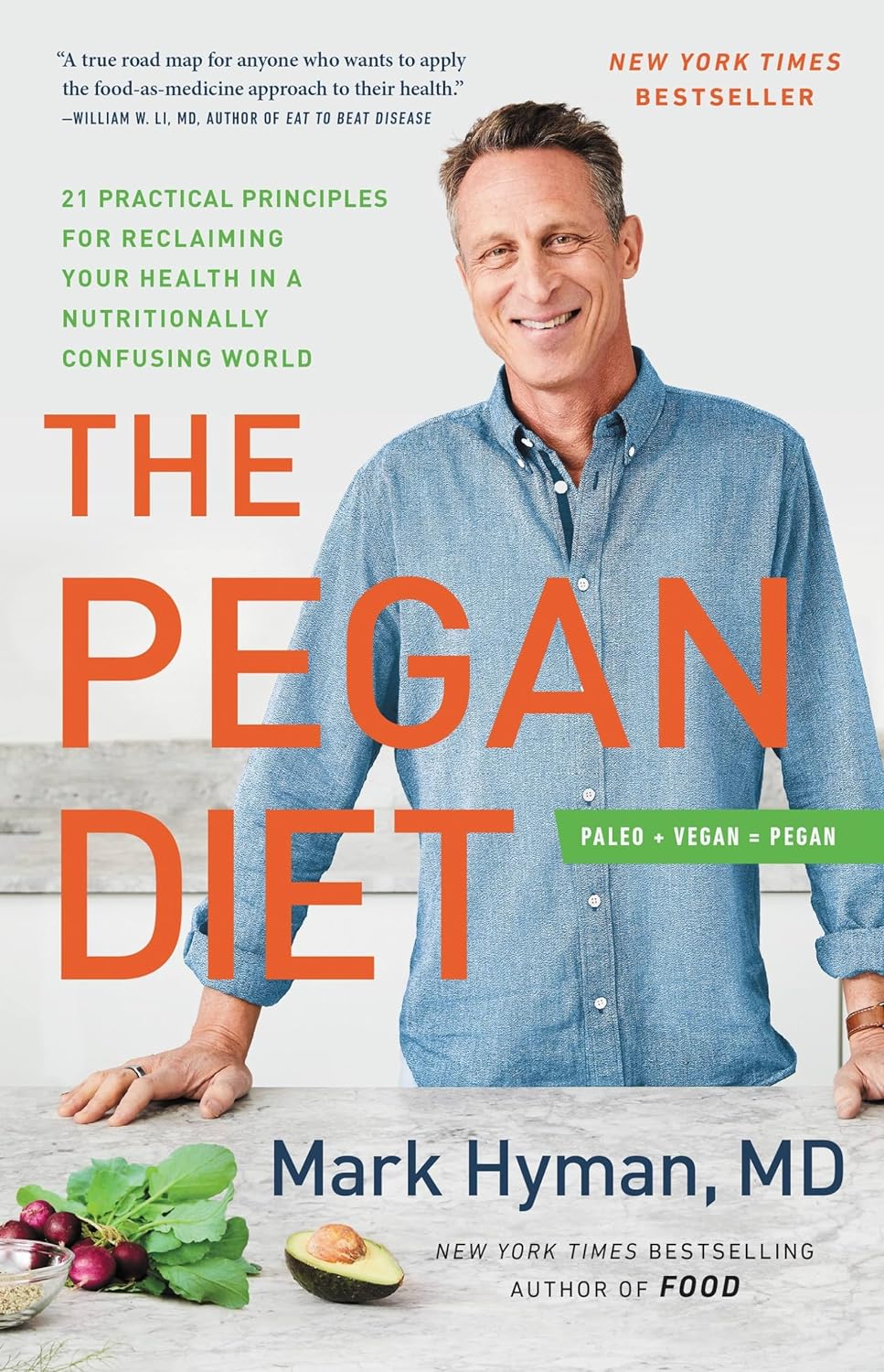
The Pegan Diet – by Dr. Mark Hyman
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
First things first: the title of the book is a little misleading. “Pegan” is a portmanteau of “paleo” and “vegan”, making it sound like it will be appropriate for both of those dietary practices. Instead:
- Dr. Hyman offers advice about eating the right grains and legumes (inappropriate for a paleo diet)
- He also offers such advice as “be picky about poultry, eggs, and fish”, and “avoid dairy—mostly” (inappropriate for a vegan diet).
So, since his paleo vegan diet is neither paleo nor vegan, what actually is it?
It’s a whole foods diet that encourages the enjoyment of a lot of plants, and discretion with regard to the quality of animal products.
It’s a very respectable approach to eating, even if it didn’t live up to the title.
The style is somewhat sensationalist, while nevertheless including plenty of actual science in there too—so the content is good, even if the presentation isn’t what this reviewer would prefer.
He has recipes; they can be a little fancy (e.g. “matcha poppy bread with rose water glaze”) which may not be to everyone’s taste, but they are healthy.
Bottom line: the content is good; the style you may love or hate, and again, don’t be misled by the title.
Share This Post
Related Posts
-
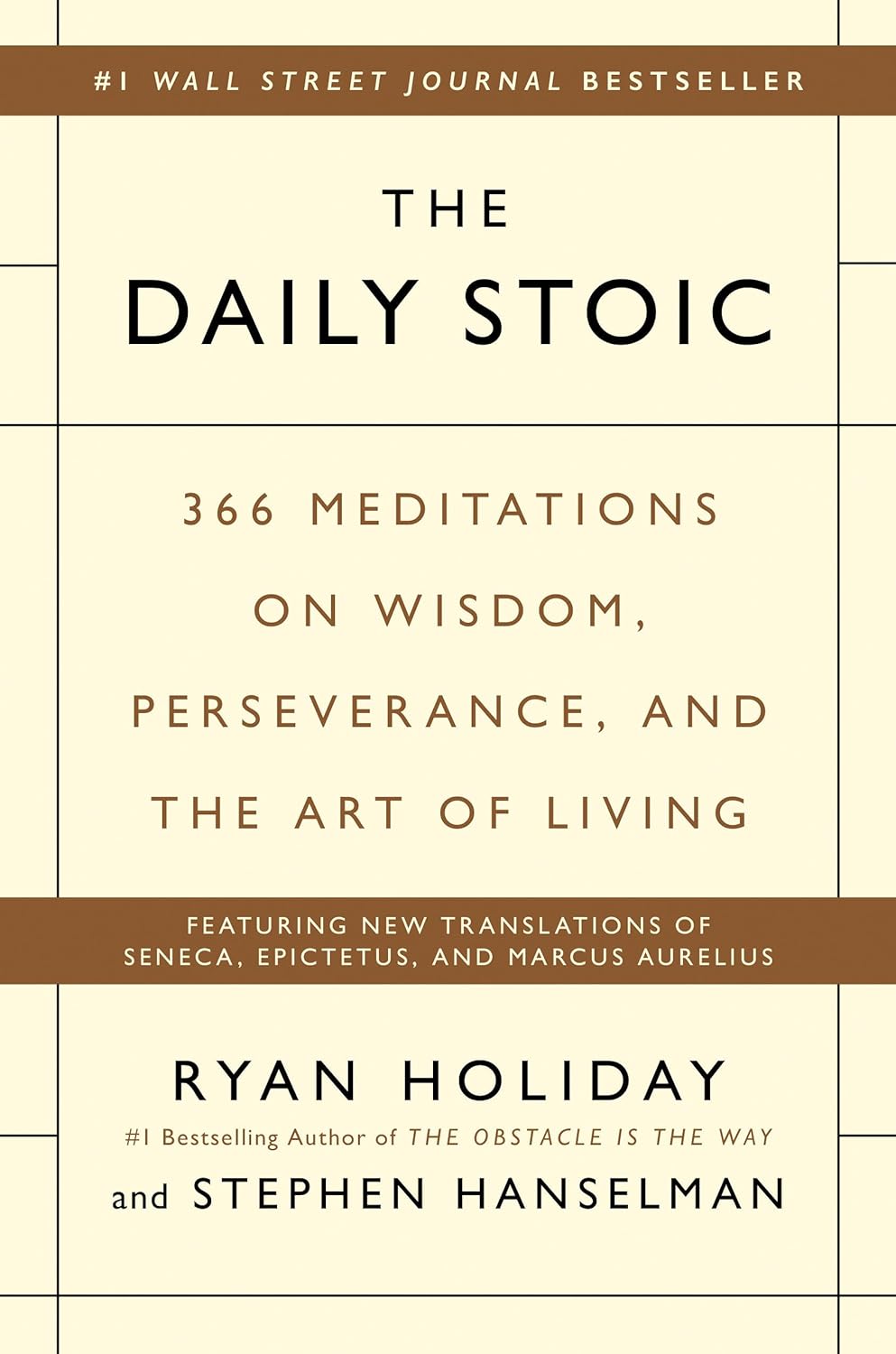
The Daily Stoic – by Ryan Holiday & Stephen Hanselman
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What’s this, a philosophy book in a health and productivity newsletter? Well, look at it this way: Aristotle basically wrote the “How To Win Friends And Influence People” of his day, and Plato before him wrote a book about management.
In this (chiefly modern!) book, we see what the later Stoic philosophers had to say about getting the most out of life—which is also what we’re about, here at 10almonds!
We tend to use the word “stoic” in modern English to refer to a person who is resolute in the face of hardship. The traditional meaning does encompass that, but also means a lot more: a whole, rounded, philosophy of life.
Philosophy in general is not an easy thing into which to “dip one’s toe”. No matter where we try to start, it seems, it turns out there were a thousand other things we needed to read first!
This book really gets around that. The format is:
- There’s a theme for each month
- Each month has one lesson per day
- Each daily lesson starts with some words from a renowned stoic philosopher, and then provides commentary on such
- The commentary provides a jumping-off point and serves as a prompt to actually, genuinely, reflect and apply the ideas.
Unlike a lot of “a year of…” day-by-day books, this is not light reading, by the way, and you are getting a weighty tome for your money.
But, the page-length daily lessons are indeed digestible—which, again, is what we like at 10almonds!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Progesterone Menopausal HRT: When, Why, And How To Benefit
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Progesterone doesn’t get talked about as much as other sex hormones, so what’s its deal? Dr. Heather Hirsch explains:
Menopausal progesterone
Dr. Hirsch considers progesterone essential for menopausal women who are taking estrogen and have an intact uterus, to keep conditions at bay such as endometriosis or even uterine cancer.
However, she advises it is not critical in those without a uterus, unless there was a previous case of one of the above conditions.
10almonds addition: on the other hand, progesterone can still be beneficial from a metabolic and body composition standpoint, so do speak with your endocrinologist about it.
As an extra bonus: while not soporific (it won’t make you sleepy), taking progesterone at night will improve the quality of your sleep once you do sleep, so that’s a worthwhile thing for many!
Dr. Hirsch also discusses the merits of continuous vs cyclic use; continuous maintains the above sleep benefits, for example, while cyclic use can help stabilize menstrual patterns in late perimenopause and early menopause.
For more on these things, plus discussion of different types of progesterone, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
- What Does “Balance Your Hormones” Even Mean?
- What You Should Have Been Told About The Menopause Beforehand
- HRT: Bioidentical vs Animal – A Tale Of Two Approaches
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Caramelized Caraway Cabbage
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Cabbage is an underrated vegetable for its many nutrients and its culinary potential—here’s a great way to make it a delectable starter or respectable side.
You will need
- 1 medium white cabbage, sliced into 1″ thick slabs
- 1 tbsp extra-virgin olive oil
- 1 tbsp caraway seeds
- 1 tsp black pepper
- ½ tsp turmeric
- ¼ tsp MSG or ½ tsp low-sodium salt
Method
(we suggest you read everything at least once before doing anything)
1) Preheat the oven to 400℉ / 200℃.
2) Combine the non-cabbage ingredients in a small bowl, whisking to mix thoroughly—with a tiny whisk if you have one, but a fork will work if necessary.
3) Arrange the cabbage slices on a lined baking tray and brush the seasoning-and-oil mixture over both sides of each slice.
4) Roast for 20–25 minutes until the cabbage is tender and beginning to caramelize.
5) Serve warm.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Curcumin (Turmeric) is worth its weight in gold
- Black Pepper’s Impressive Anti-Cancer Arsenal (And More)
- Avocado Oil vs Olive Oil – Which is Healthier?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: