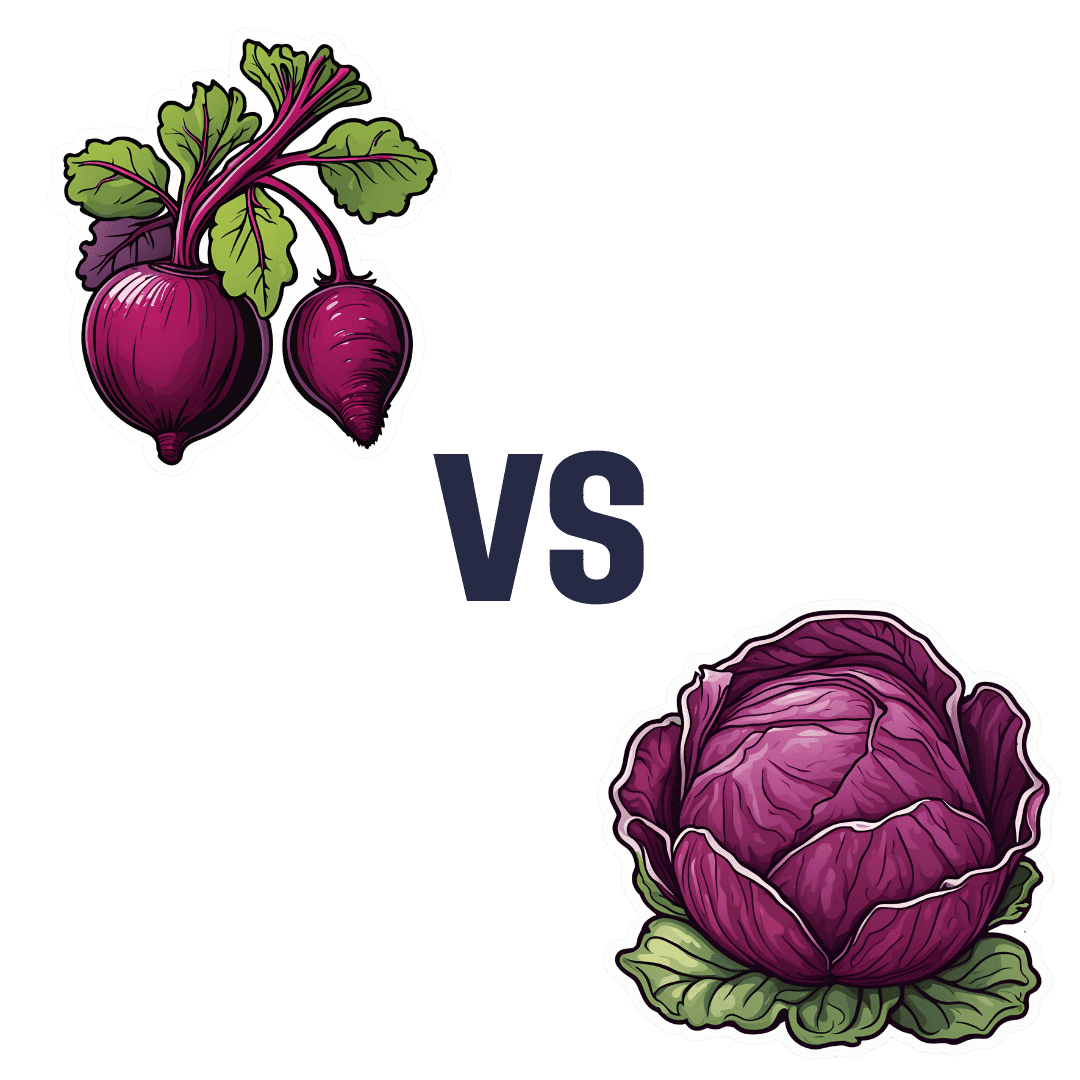
Beetroot vs Red Cabbage – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing beetroot to red cabbage, we picked the red cabbage.
Why?
Both are great, and both have their strengths!
In terms of macros, beetroot has very slightly more protein, carbs, and fiber, but the margins of difference are very small in each case. However, in terms of glycemic index, red cabbage has the considerably lower glycemic index, of 32 (low) as opposed to beetroot’s GI of 64 (medium). On the strength of this GI difference, we call this category a win for red cabbage.
In the category of vitamins, beetroot has more of vitamin B9, while red cabbage has a lot more of vitamins A, B1, B2, B3, B6, C, E, K, and choline. By strength of numbers and also by having very large margins of difference on most of those, red cabbage is the clear winner here.
When it comes to minerals, beetroot has more copper, magnesium, manganese, phosphorus, and potassium, while red cabbage has more calcium (and about ⅓ of the sodium). By the numbers, this is a win for beetroot, though it’s worth noting that the margins of difference were small, i.e. red cabbage was right behind beetroot on each of those.
Adding up the sections makes for an overall red cabbage win, but as we say, beetroot is great too, especially when it comes to minerals!
As ever, enjoy either or both; diversity is good.
Want to learn more?
You might like to read:
No, beetroot isn’t vegetable Viagra. But here’s what it can do!
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Fatigue? Unexplained weight gain and dry skin? Could it be Hashimoto’s disease?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Maybe you feel worn out. Perhaps you’re also having trouble losing weight. Generally, you just don’t feel 100%.
Could it be Hashimoto’s disease? This common autoimmune thyroid disorder is when your immune system (which fights off viruses and bacteria), mistakenly attacks a part of your body. In this case, it’s your thyroid – a gland located at the base of your neck – and can cause low thyroid hormones levels (hypothyroidism).
Hypothyroidism affects one in 33 Australians and Hashimoto’s is one of the most common thyroid conditions in first-world countries.
While symptoms can be subtle, untreated Hashimoto’s can cause long-term problems with your heart, memory and fertility. Here is what you need to know.
What happens when you have Hashimoto’s?
Your thyroid gland is a butterfly-shaped gland in the neck. It is essential in regulating things like muscle function, digestion, metabolism, the heart and lungs. In children, thyroid hormones are also needed for normal growth and development.
Hashimoto’s thyroid disease, named after the Japanese doctor who discovered it in 1912, is also known as Hashimoto’s thyroiditis or chronic lymphocytic thyroiditis. The disease can cause the immune system to mistakenly produce proteins called antibodies (thyroid peroxidase and thyroglobulin). These can cause inflammation and long-term damage to the thyroid gland. Over time, as thyroid tissue is inflamed and/or destroyed, there can be a decrease in the production of thyroid hormones (hypothyroidism).
Hashimoto’s can present subtly at first. If you only have antibodies with no change in thyroid levels, it is likely you won’t have any symptoms.
However, as the disease progresses, you may experience fatigue, weight gain (or difficulty losing weight), increased sensitivity to the cold, constipation, dry skin, muscle aches, irregular or heavy menstrual cycles, enlarged thyroid (goitre) and occasionally hair loss, including at the ends of your eyebrows.
What causes Hashimoto’s thyroid disease?
Several risk factors can contribute to the development of Hashimoto’s including:
-
genetic risk – your risk is higher if you have family members with Hashimoto’s
-
gender – women are up to ten times more likely than men to develop the disease
-
age – you are more likely to develop the disease from 30 to 50 years of age
-
autoimmune condition – having another autoimmune condition like systemic lupus, Type 1 diabetes and celiac disease increases your risk
-
excessive iodine intake and radiation exposure may also increase risk in people who are already genetically at greater risk.
What are the long-term risks?
Long-term, untreated Hashimoto’s thyroiditis can cause heart issues, higher cholesterol levels, nerve damage (peripheral neuropathy), reduced cognition and infertility.
In pregnancy, Hashimoto’s has a higher risk of pre-eclampsia (high blood pressure affecting several organs), premature birth, placental abruption (when the placenta separates from the inner wall of the uterus before birth) and, in severe cases, pregnancy loss.
The disease has also been linked with an increased risk (but low incidence) of the lymphocytes of the thyroid turning into cancer cells to cause thyroid lymphoma.
How is Hashimoto’s diagnosed?
Diagnosis can be confirmed with a blood test to check thyroid levels and antibodies.
Thyroid peroxidase antibodies are commonly present but about 5% of patients test antibody-negative. In those people, diagnosis depends on the thyroid levels, clinical presentation and ultrasound appearance of general inflammation. An ultrasound may not be required though, especially if the diagnosis is obvious.
Three hormone levels are tested to determine if you have Hashimoto’s.
Thyroid stimulating hormone (TSH) is produced by the brain to speak to the thyroid, telling it to produce two types of thyroid hormones – T3 and T4.
If you have either relative or absolute thyroid hormone deficiency, a test will show the stimulating hormones as high because the brain is trying to get the thyroid to work harder.
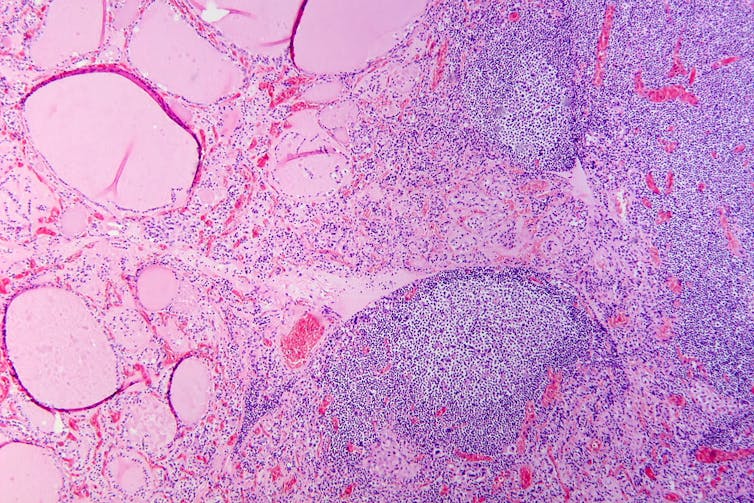
Hashimoto’s thyroiditis under the microscope. Antibodies against thyroid peroxidase and thyroglobulin were elevated.
Patho/Wikimedia Commons, CC BY-SACan it be treated?
The management of Hashimoto’s depends on the severity of the thyroid levels. Up to 20% of the population can have antibodies but normal thyroid levels. This is still Hashimoto’s thyroid disease, but it is very mild and does not require treatment. There is no current treatment to reduce antibody levels alone.
Because thyroid peroxidase antibodies increase the risk of abnormal thyroid levels in the future, regular thyroid testing is recommended.
When the thyroid stimulating hormone is high with normal thyroid hormone levels it is termed “subclinical hypothyroidism”. When it is paired with low hormone levels it is called “overt hypothyroidism”. The first is a mild form of the disease and treatment depends on the degree of stimulating hormone elevation.
Overt hypothyroidism warrants treatment. The main form of this is thyroid hormone replacement therapy (levothyroxine) with the dose of the drug adjusted until thyroid levels are within the normal range. This is usually a lifelong treatment but, once the dose is optimised, hormone levels usually remain relatively stable.
In some people with very enlarged thyroid glands causing compressive symptoms (such as difficulty swallowing or breathing), thyroidectomy (surgical removal of the thyroid) is considered.
Hashimoto’s thyroiditis is a common condition caused by your body’s immune system incorrectly damaging to your thyroid and can go undetected. Long-term, untreated, it can cause issues with your heart, cognition, and fertility. It can be diagnosed with a simple blood test. Speak to your doctor if you have any concerns as early diagnosis and treatment can help prevent complications.
Aakansha Zala, The University of Queensland
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
-
How worried should I be about cryptosporidiosis? Am I safe at the pool?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
You might have heard of something called “cryptosporidiosis” recently, closely followed by warnings to stay away from your local swimming pool if you’ve had diarrhoea.
More than 700 cases of this gastrointestinal disease were reported in Queensland in January, which is 13 times more than in January last year. Just under 500 cases have been recorded in New South Wales this year to-date, while other states have similarly reported an increase in the number of cryptosporidiosis infections in recent months.
Cryptosporidiosis has been listed as a national notifiable disease in Australia since 2001.
But what exactly is it, and should we be worried?What causes cryptosporidiosis, and who is affected?
Cryptosporidiosis is the disease caused by the parasite Cryptosporidium, of which there are two types that can make us sick. Cryptosporidum hominis only affects humans and is the major cause of recent outbreaks in Australia, while Cryptosporidium parvum can also affect animals.
The infection is spread by spores called oocysts in the stools of humans and animals. When ingested, these oocysts migrate and mature in the small bowel. They damage the small bowel lining and can lead to diarrhoea, nausea, vomiting, fever and abdominal discomfort.
Most people develop symptoms anywhere from one to 12 days after becoming infected. Usually these symptoms resolve within two weeks, but the illness may last longer and can be severe in those with a weakened immune system.
Children and the elderly tend to be the most commonly affected. Cryptosporidiosis is more prevalent in young children, particularly those under five, but the disease can affect people of any age.
A number of public pools have been closed lately due to cryptosporidiosis outbreaks.
LBeddoe/ShutterstockSo how do we catch it?
Most major outbreaks of cryptosporidiosis have been due to people drinking contaminated water. The largest recorded outbreak occurred in Milwaukee in 1993 where 403,000 people were believed to have been infected.
Cryptosporidium oocysts are very small in size and in Milwaukee they passed through the filtration system of one of the water treatment plants undetected, infecting the city’s water supply. As few as ten oocysts can cause infection, making it possible for contaminated drinking water to affect a very large number of people.
Four days after infection a person with cryptosporidiosis can shed up to ten billion oocysts into their stool a day, with the shedding persisting for about two weeks. This is why one infected person in a swimming pool can infect the entire pool in a single visit.
Cryptosporidium oocysts excreted in the faeces of infected humans and animals can also reach natural bodies of water such as beaches, rivers and lakes directly through sewer pipes or indirectly such as in manure transported with surface runoff after heavy rain.
One study which modelled Cryptosporidium concentrations in rivers around the world estimated there are anywhere from 100 to one million oocysts in a litre of river water.
In Australia, cryptosporidiosis outbreaks tend to occur during the late spring and early summer periods when there’s an increase in recreational water activities such as swimming in natural water holes, water catchments and public pools. We don’t know exactly why cases have seen such a surge this summer compared to other years, but we know Cryptosporidium is very infectious.
Oocysts have been found in foods such as fresh vegetables and seafood but these are not common sources of infection in Australia.
What about chlorine?
Contrary to popular belief, chlorine doesn’t kill off all infectious microbes in a swimming pool. Cryptosporidium oocysts are hardy, thick-walled and resistant to chlorine and acid. They are not destroyed by chlorine at the normal concentrations found in swimming pools.
We also know oocysts can be significantly protected from the effects of chlorine in swimming pools by faecal material, so the presence of even small amounts of faecal matter contaminated with Cryptosporidium in a swimming pool would necessitate closure and a thorough decontamination.
Young children and in particular children in nappies are known to increase the potential for disease transmission in recreational water. Proper nappy changing, frequent bathroom breaks and showering before swimming to remove faecal residue are helpful ways to reduce the risk.
Cryptosporidium can spread in other bodies of water, not just swimming pools.
Yulia Simonova/ShutterstockSome sensible precautions
Other measures you can take to reduce yours and others’ risk of cryptosporidiosis include:
- avoid swimming in natural waters such as rivers and creeks during and for at least three days after heavy rain
- avoid swimming in beaches for at least one day after heavy rain
- avoid drinking untreated water such as water from rivers or springs. If you need to drink untreated water, boiling it first will kill the Cryptosporidium
- avoid swallowing water when swimming if you can
- if you’ve had diarrhoea, avoid swimming for at least two weeks after it has resolved
- avoid sharing towels or linen for at least two weeks after diarrhoea has resolved
- avoid sharing, touching or preparing food that other people may eat for at least 48 hours after diarrhoea has resolved
- wash your hands with soap and water after going to the bathroom or before preparing food (Cryptosporidium is not killed by alcohol gels and sanitisers).
Not all cases of diarrhoea are due to cryptosporidiosis. There are many other causes of infectious gastroenteritis and because the vast majority of the time recovery is uneventful you don’t need to see a doctor unless very unwell. If you do suspect you may have cryptosporidiosis you can ask your doctor to refer you for a stool test.
Vincent Ho, Associate Professor and clinical academic gastroenterologist, Western Sydney University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
What you need to know about the new weight loss drug Zepbound
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In a recent poll, KFF found that nearly half of U.S. adults were interested in taking a weight management drug like the increasingly popular Ozempic, Wegovy, and Mounjaro.
“I can understand why there would be widespread interest in these medications,” says Dr. Alyssa Lampe Dominguez, an endocrinologist and clinical assistant professor at the University of Southern California. “Obesity is a chronic disease that is very difficult to treat. And a lot of the medications that we previously used weren’t as effective.”
Now, there’s a new option available: In November 2023, the FDA approved Zepbound, another weight management medication, developed by the pharmaceutical company Eli Lilly. Zepbound is different from other drugs in many ways, including the fact that it’s proven to be the most effective option so far.
Keep reading to find out more about Zepbound, including who can take it, its side effects, and more.
What is Zepbound?
Zepbound, one of the brand names for tirzepatide, is an injectable drug with a maximum dosage of 15 mg per week. It’s based on incretin, a hormone that’s naturally released in the gut after a meal. (Mounjaro is another brand name for tirzepatide.)
Tirzepatide is considered a dual agonist because it activates the two primary incretin hormones: the glucagon-like peptide-1 (GLP-1) and gastric inhibitory peptide (GIP) hormones.
According to Dr. Katherine H. Saunders, an obesity medicine physician at Weill Cornell Medicine and co-founder of Intellihealth, tirzepatide is involved with several processes that regulate blood sugar, slow the removal of food from the stomach, and affect brain areas involved in appetite.
This means that people taking the medication feel less hungry and get fuller faster, leading to less food intake and, ultimately, weight loss.
How is Zepbound different from Ozempic?
The medications are different in many ways. Ozempic and Wegovy, which are both brand names for semaglutide, only target the GLP-1 hormone. Studies have shown that Zepbound can lead to a higher percentage of total body weight loss than semaglutide medications. In addition to being more effective, there is some evidence that Zepbound is overall more tolerable than Ozempic or Wegovy.
“I have seen overall lower rates in severity of side effects with the tirzepatide medications. Mounjaro [tirzepatide] in particular is the one that I’ve used up until this point, but there’s a thought that the GIP component of the medication actually decreases nausea,” adds Lampe Dominguez. “Anecdotally, patients that I have switched from semaglutide or Ozempic to Mounjaro say that they have less side effects with Mounjaro.”
How is Zepbound different from Mounjaro?
Zepbound and Mounjaro are the same medication—tirzepatide—but they’re approved for different conditions. Zepbound is FDA-approved for weight loss, while Mounjaro is approved for type 2 diabetes. (However, Mounjaro is also at times prescribed off-label for weight loss.)
What are some of Zepbound’s side effects?
According to the FDA, side effects include nausea, vomiting, diarrhea, constipation, stomach discomfort and pain, fatigue, and burping. See a more comprehensive list of side effects here.
Who can take Zepbound?
Zepbound is FDA-approved for adults with obesity (a BMI of 30 or greater) or who have a BMI of 27 or greater with at least one weight-related condition, like high blood pressure, type 2 diabetes, or high cholesterol.
“I tend to advise patients who don’t meet those criteria to not take these medications because we really don’t know what the risks are,” says Lampe Dominguez, adding that people with lower BMI weren’t included in the medication’s studies. “We don’t know if there are specific risks to using this medication at a lower body mass index [or] if there might be some negative outcomes.”
Both doctors agree that it’s important for people who are interested in starting any weight loss medication to talk to their doctors about the potential risks and benefits. For instance, the FDA notes that Zepbound has caused thyroid tumors in rats, and while it’s unknown if this could also happen to humans, the agency said the medication shouldn’t be used in patients with a personal or family history of medullary thyroid cancer.
“Zepbound is a powerful medication that can lead to severe side effects, vitamin deficiencies, a complete lack of appetite, or too much weight loss if prescribed without the appropriate personalization, education, and close monitoring,” says Saunders.
“With all of these medications, and particularly with Zepbound, we would want to make sure that [patients] don’t have a family history of a specific type of thyroid cancer called medullary thyroid cancer,” says Lampe Dominguez.
How long should people take Zepbound for?
“Anti-obesity medications like Zepbound are not meant for short-term weight loss, but long-term treatment of obesity, which is a chronic disease,” explains Saunders. “We prepare our patients to be on the medication (or some type of medical obesity treatment) long term for their chronic disease, which is only controlled for the duration of time they’re being treated.”
For more information, talk to your health care provider.
This article first appeared on Public Good News and is republished here under a Creative Commons license.
Share This Post
Related Posts
-
The Diet Compass – by Bas Kast
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Facts about nutrition and health can be hard to memorize. There’s just so much! And often there are so many studies, and while the science is not usually contradictory, pop-science headlines sure can be. What to believe?
Bas Kast brings us a very comprehensive and easily digestible solution.
A science journalist himself, he has gone through the studies so that you don’t have to, and—citing them along the way—draws out the salient points and conclusions.
But, he’s not just handing out directions (though he does that too); he’s arranged and formatted the information in a very readable and logical fashion. Chapter by chapter, we learn the foundations of important principles for “this is better than that” choices in diet.
Most importantly, he lays out for us his “12 simple rules for healthy eating“, and they are indeed as simple as they are well-grounded in good science.
Bottom line: if you want “one easy-reading book” to just tell you how to make decisions about your diet, simply follow those rules and enjoy the benefits… Then this book is exactly that.
Click here to check out The Diet Compass and get your diet on the right track!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Ayurveda’s Contributions To Science
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Ayurveda’s Contributions To Science (Without Being Itself Rooted in Scientific Method)
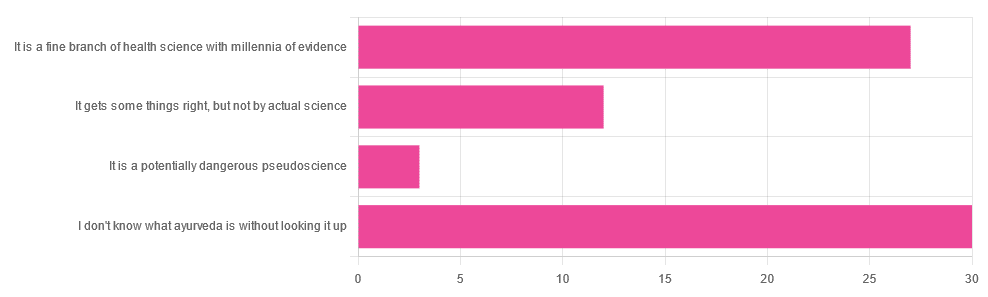
Yesterday, we asked you for your opinions on ayurveda, and got the above-depicted, below-described, set of responses. Of those who responded…
- A little over 41% said “I don’t know what ayurveda is without looking it up”
- A little over 37% said “It is a fine branch of health science with millennia of evidence”
- A little over 16% said “It gets some things right, but not by actual science”
- A little over 4% said “It is a potentially dangerous pseudoscience”
So, what does the science say?
Ayurveda is scientific: True or False?
False, simply. Let’s just rip the band-aid off in this case. That doesn’t mean it’s necessarily without merit, though!
Let’s put it this way:
- If you drink coffee to feel more awake because scientific method has discerned that caffeine has vasoconstrictive and adenosine-blocking effects while also promoting dopaminergic activity, then your consumption of coffee is evidence-based and scientific. Great!
- If you drink coffee to feel more awake because somebody told you that that somebody told them that it energizes you by balancing the elements fire (the heat of the coffee), air (the little bubbles on top), earth (the coffee grinds), water (the water), and ether (steam), then that is neither evidence-based nor scientific, but it will still work exactly the same.
Ayurveda is a little like that. It’s an ancient traditional Indian medicine, based on a combination of anecdotal evidence and supposition.
- The anecdotal evidence from ayurveda has often resulted in herbal remedies that, in modern scientific trials, have been found to have merit.
- Ayurvedic meditative practices also have a large overlap with modern mindfulness practices, and have also been found to have merit
- Ayurveda also promotes the practice of yoga, which is indeed a very healthful activity
- The supposition from ayurveda is based largely in those five elements we mentioned above, as well as a “balancing of humors” comparable to medieval European medicine, and from a scientific perspective, is simply a hypothesis with no evidence to support it.
Note: while ayurveda is commonly described as a science by its practitioners in the modern age, it did not originally claim to be scientific, but rather, wisdom handed down directly by the god Dhanvantari.
Ayurveda gets some things right: True or False?
True! Indeed, we covered some before in 10almonds; you may remember:
Bacopa Monnieri: A Well-Evidenced Cognitive Enhancer
(Bacopa monnieri is also known by its name in ayurveda, brahmi)
There are many other herbs that have made their way from ayurveda into modern science, but the above is a stand-out example. Others include:
- Ashwagandha: The Root of All Even-Mindedness?
- Boswellia serrata (Frankincense) Against Pain and Depression/Anxiety
Yoga and meditation are also great, and not only that, but great by science, for example:
- NCCIH | Yoga for Health: Clinical Guidelines, Scientific Literature, Info for Patients
- The Neuroscience of Mindfulness: How Mindfulness Alters the Brain and Facilitates Emotion Regulation
Ayurveda is a potentially dangerous pseudoscience: True or False?
Also True! We covered why it’s a pseudoscience above, but that doesn’t make it potentially dangerous, per se (you’ll remember our coffee example).
What does, however, make it potentially dangerous (dose-dependent) is its use of heavy metals such as lead, mercury, and arsenic:
Heavy Metal Content of Ayurvedic Herbal Medicine Products
Some final thoughts…
Want to learn more about the sometimes beneficial, sometimes uneasy relationship between ayurveda and modern science?
A lot of scholarly articles trying to bridge (or further separate) the two were very biased one way or the other.
Instead, here’s one that’s reasonably optimistic with regard to ayurveda’s potential for good, while being realistic about how it currently stands:
Development of Ayurveda—Tradition to trend
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
3 signs your diet is causing too much muscle loss – and what to do about it
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When trying to lose weight, it’s natural to want to see quick results. So when the number on the scales drops rapidly, it seems like we’re on the right track.
But as with many things related to weight loss, there’s a flip side: rapid weight loss can result in a significant loss of muscle mass, as well as fat.
So how you can tell if you’re losing too much muscle and what can you do to prevent it?
EvMedvedeva/Shutterstock Why does muscle mass matter?
Muscle is an important factor in determining our metabolic rate: how much energy we burn at rest. This is determined by how much muscle and fat we have. Muscle is more metabolically active than fat, meaning it burns more calories.
When we diet to lose weight, we create a calorie deficit, where our bodies don’t get enough energy from the food we eat to meet our energy needs. Our bodies start breaking down our fat and muscle tissue for fuel.
A decrease in calorie-burning muscle mass slows our metabolism. This quickly slows the rate at which we lose weight and impacts our ability to maintain our weight long term.
How to tell you’re losing too much muscle
Unfortunately, measuring changes in muscle mass is not easy.
The most accurate tool is an enhanced form of X-ray called a dual-energy X-ray absorptiometry (DXA) scan. The scan is primarily used in medicine and research to capture data on weight, body fat, muscle mass and bone density.
But while DEXA is becoming more readily available at weight-loss clinics and gyms, it’s not cheap.
There are also many “smart” scales available for at home use that promise to provide an accurate reading of muscle mass percentage.
Some scales promise to tell us our muscle mass. Lee Charlie/Shutterstock However, the accuracy of these scales is questionable. Researchers found the scales tested massively over- or under-estimated fat and muscle mass.
Fortunately, there are three free but scientifically backed signs you may be losing too much muscle mass when you’re dieting.
1. You’re losing much more weight than expected each week
Losing a lot of weight rapidly is one of the early signs that your diet is too extreme and you’re losing too much muscle.
Rapid weight loss (of more than 1 kilogram per week) results in greater muscle mass loss than slow weight loss.
Slow weight loss better preserves muscle mass and often has the added benefit of greater fat mass loss.
One study compared people in the obese weight category who followed either a very low-calorie diet (500 calories per day) for five weeks or a low-calorie diet (1,250 calories per day) for 12 weeks. While both groups lost similar amounts of weight, participants following the very low-calorie diet (500 calories per day) for five weeks lost significantly more muscle mass.
2. You’re feeling tired and things feel more difficult
It sounds obvious, but feeling tired, sluggish and finding it hard to complete physical activities, such as working out or doing jobs around the house, is another strong signal you’re losing muscle.
Research shows a decrease in muscle mass may negatively impact your body’s physical performance.
3. You’re feeling moody
Mood swings and feeling anxious, stressed or depressed may also be signs you’re losing muscle mass.
Research on muscle loss due to ageing suggests low levels of muscle mass can negatively impact mental health and mood. This seems to stem from the relationship between low muscle mass and proteins called neurotrophins, which help regulate mood and feelings of wellbeing.
So how you can do to maintain muscle during weight loss?
Fortunately, there are also three actions you can take to maintain muscle mass when you’re following a calorie-restricted diet to lose weight.
1. Incorporate strength training into your exercise plan
While a broad exercise program is important to support overall weight loss, strength-building exercises are a surefire way to help prevent the loss of muscle mass. A meta-analysis of studies of older people with obesity found resistance training was able to prevent almost 100% of muscle loss from calorie restriction.
Relying on diet alone to lose weight will reduce muscle along with body fat, slowing your metabolism. So it’s essential to make sure you’ve incorporated sufficient and appropriate exercise into your weight-loss plan to hold onto your muscle mass stores.
Strength-building exercises help you retain muscle. BearFotos/Shutterstock But you don’t need to hit the gym. Exercises using body weight – such as push-ups, pull-ups, planks and air squats – are just as effective as lifting weights and using strength-building equipment.
Encouragingly, moderate-volume resistance training (three sets of ten repetitions for eight exercises) can be as effective as high-volume training (five sets of ten repetitions for eight exercises) for maintaining muscle when you’re following a calorie-restricted diet.
2. Eat more protein
Foods high in protein play an essential role in building and maintaining muscle mass, but research also shows these foods help prevent muscle loss when you’re following a calorie-restricted diet.
But this doesn’t mean just eating foods with protein. Meals need to be balanced and include a source of protein, wholegrain carb and healthy fat to meet our dietary needs. For example, eggs on wholegrain toast with avocado.
3. Slow your weight loss plan down
When we change our diet to lose weight, we take our body out of its comfort zone and trigger its survival response. It then counteracts weight loss, triggering several physiological responses to defend our body weight and “survive” starvation.
Our body’s survival mechanisms want us to regain lost weight to ensure we survive the next period of famine (dieting). Research shows that more than half of the weight lost by participants is regained within two years, and more than 80% of lost weight is regained within five years.
However, a slow and steady, stepped approach to weight loss, prevents our bodies from activating defence mechanisms to defend our weight when we try to lose weight.
Ultimately, losing weight long-term comes down to making gradual changes to your lifestyle to ensure you form habits that last a lifetime.
At the Boden Group, Charles Perkins Centre, we are studying the science of obesity and running clinical trials for weight loss. You can register here to express your interest.
Nick Fuller, Charles Perkins Centre Research Program Leader, University of Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: