Beat Food Addictions!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When It’s More Than “Just” Cravings
This is Dr. Nicole Avena. She’s a research neuroscientist who also teaches at Mount Sinai School of Medicine, as well as at Princeton. She’s done a lot of groundbreaking research in the field of nutrition, diet, and addition, with a special focus on women’s health and sugar intake specifically.
What does she want us to know?
Firstly, that food addictions are real addictions.
We know it can sound silly, like the famous line from Mad Max:
❝Do not, my friends, become addicted to water. It will take hold of you and you will resent its absence!❞
As an aside, it is actually possible to become addicted to water; if one drinks it excessively (we are talking gallons every day) it does change the structure of the brain (no surprise; the brain is not supposed to have that much water!) causing structural damage that then results in dependency, and headaches upon withdrawal. It’s called psychogenic polydipsia:
But back onto today’s more specific topic, and by a different mechanism of addiction…
Food addictions are dopaminergic addictions (as is cocaine)
If you are addicted to a certain food (often sugar, but other refined carbs such as potato products, and also especially refined flour products, are also potential addictive substances), then when you think about the food in question, your brain lights up with more dopamine than it should, and you are strongly motivated to seek and consume the substance in question.
Remember, dopamine functions by expectation, not by result. So until your brain’s dopamine-gremlin is sated, it will keep flooding you with motivational dopamine; that’s why the first bite tastes best, then you wolf down the rest before your brain can change its mind, and afterwards you may be left thinking/feeling “was that worth it?”.
Much like with other addictions (especially alcohol), shame and regret often feature strongly afterwards, even accompanied by notions of “never again”.
But, binge-eating is as difficult to escape as binge-drinking.
You can break free, but you will probably have to take it seriously
Dr. Avena recommends treating a food addiction like any other addiction, which means:
- Know why you want to quit (make a list of the reasons, and this will help you stay on track later!)
- Make a conscious decision to genuinely quit
- Learn about the nature of the specific addiction (know thy enemy!)
- Choose a strategy (e.g. wean off vs cold turkey, and decide what replacements, if any, you will use)
- Get support (especially from those around you, and/but the support of others facing, or who have successfully faced, the same challenge is very helpful too)
- Keep track of your success (build and maintain a streak!)
- Lean into how you will better enjoy life without addiction to the substance (it never really made you happy anyway, so enjoy your newfound freedom and good health!)
Want more from Dr. Avena?
You can check out her column at Psychology Today here:
Psychology Today | Food Junkie ← it has a lot of posts about sugar addiction in particular, and gives a lot of information and practical advice
You can also read her book, which could be a great help if you are thinking of quitting a sugar addiction:
Sugarless: A 7-Step Plan to Uncover Hidden Sugars, Curb Your Cravings, and Conquer Your Addiction
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Keep Inflammation At Bay
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How to Prevent (or Reduce) Inflammation
You asked us to do a main feature on inflammation, so here we go!
Before we start, it’s worth noting an important difference between acute and chronic inflammation:
- Acute inflammation is generally when the body detects some invader, and goes to war against it. This (except in cases such as allergic responses) is usually helpful.
- Chronic inflammation is generally when the body does a civil war. This is almost never helpful.
We’ll be tackling the latter, which frees up your body’s resources to do better at the former.
First, the obvious…
These five things are as important for this as they are for most things:
- Get a good diet—the Mediterranean diet is once again a top-scorer
- Exercise—move and stretch your body; don’t overdo it, but do what you reasonably can, or the inflammation will get worse.
- Reduce (or ideally eliminate) alcohol consumption. When in pain, it’s easy to turn to the bottle, and say “isn’t this one of red wine’s benefits?” (it isn’t, functionally*). Alcohol will cause your inflammation to flare up like little else.
- Don’t smoke—it’s bad for everything, and that goes for inflammation too.
- Get good sleep. Obviously this can be difficult with chronic pain, but do take your sleep seriously. For example, invest in a good mattress, nice bedding, a good bedtime routine, etc.
*Resveratrol (which is a polyphenol, by the way), famously found in red wine, does have anti-inflammatory properties. However, to get enough resveratrol to be of benefit would require drinking far more wine than will be good for your inflammation or, indeed, the rest of you. So if you’d like resveratrol benefits, consider taking it as a supplement. Superficially it doesn’t seem as much fun as drinking red wine, but we assure you that the results will be much more fun than the inflammation flare-up after drinking.
About the Mediterranean Diet for this…
There are many causes of chronic inflammation, but here are some studies done with some of the most common ones:
- Beneficial effect of Mediterranean diet in systemic lupus erythematosus patients
- How the Mediterranean diet and some of its components modulate inflammatory pathways in arthritis
- The effects of the Mediterranean diet on biomarkers of vascular wall inflammation and plaque vulnerability in subjects with high risk for cardiovascular disease
- Adherence to Mediterranean diet and 10-year incidence of diabetes: correlations with inflammatory and oxidative stress biomarkers*
*Type 1 diabetes is a congenital autoimmune disorder, as the pancreas goes to war with itself. Type 2 diabetes is different, being a) acquired and b) primarily about insulin resistance, and/but this is related to chronic inflammation regardless. It is also possible to have T1D and go on to develop insulin resistance, and that’s very bad, and/but beyond the scope of today’s newsletter, in which we are focusing on the inflammation aspects.
Some specific foods to eat or avoid…
Eat these:
- Leafy greens
- Cruciferous vegetables
- Tomatoes
- Fruits in general (berries in particular)
- Healthy fats, e.g. olives and olive oil
- Almonds and other nuts
- Dark chocolate (choose high cocoa, low sugar)
Avoid these:
- Processed meats (absolute worst offenders are hot dogs, followed by sausages in general)
- Red meats
- Sugar (includes most fruit juices, but not most actual fruits—the difference with actual fruits is they still contain plenty of fiber, and in many cases, antioxidants/polyphenols that reduce inflammation)
- Dairy products (unless fermented, in which case it seems to be at worst neutral, sometimes even a benefit, in moderation)
- White flour (and white flour products, e.g. white bread, white pasta, etc)
- Processed vegetable oils
See also: 9 Best Drinks To Reduce Inflammation, Says Science
Supplements?
Some supplements that have been found to reduce inflammation include:
(links are to studies showing their efficacy)
Consider Intermittent Fasting
Remember when we talked about the difference between acute and chronic inflammation? It’s fair to wonder “if I reduce my inflammatory response, will I be weakening my immune system?”, and the answer is: generally, no.
Often, as with the above supplements and dietary considerations, reducing inflammation actually results in a better immune response when it’s actually needed! This is because your immune system works better when it hasn’t been working in overdrive constantly.
Here’s another good example: intermittent fasting reduces the number of circulating monocytes (a way of measuring inflammation) in healthy humans—but doesn‘t compromise antimicrobial (e.g. against bacteria and viruses) immune response.
See for yourself: Dietary Intake Regulates the Circulating Inflammatory Monocyte Pool ← the study is about the anti-inflammatory effects of fasting
Share This Post
-
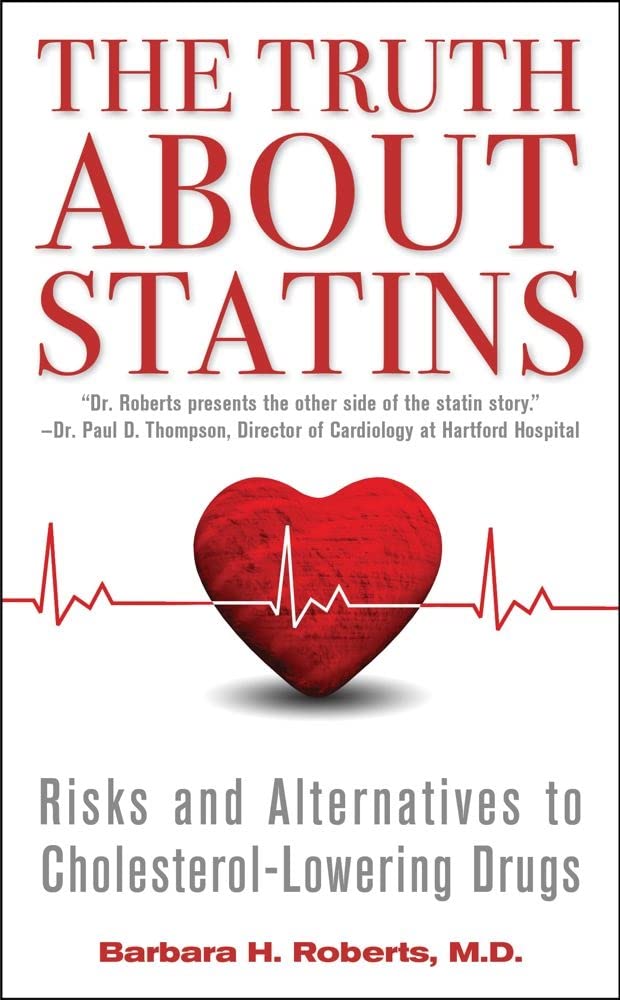
The Truth About Statins – by Barbara H. Roberts, M.D.
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
All too often, doctors looking to dispense a “quick fix” will prescribe from their playbook of a dozen or so “this will get you out of my office” drugs. Most commonly, things that treat symptoms rather than the cause. Sometimes, this can be fine! For example, in some cases, painkillers and antidepressants can make a big improvement to people’s lives. What about statins, though?
Prescribed to lower cholesterol, they broadly do exactly that. However…
Dr. Roberts wants us to know that we could be missing the big picture of heart health, and making a potentially fatal mistake.
This is not to say that the book argues that statins are necessarily terrible, or that they don’t have their place. Just, we need to understand what they will and won’t do, and make an informed choice.
To which end, she does advise regards when statins can help the most, and when they may not help at all. She also covers the questions to ask if your doctor wants to prescribe them. And—all so frequently overlooked—the important differences between men’s and women’s heart health, and the implications these have for the efficacy (or not) of statins.
With regard to the “alternatives to cholesterol-lowering drugs” promised in the subtitle… we won’t keep any secrets here:
Dr. Roberts (uncontroversially) recommends the Mediterranean diet. She also provides two weeks’ worth of recipes for such, in the final part of the book.
All in all, an important book to read if you or a loved one are taking, or thinking of taking, statins.
Pick up your copy of The Truth About Statins on Amazon today!
Share This Post
-
Hazelnuts vs Cashews – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing hazelnuts to cashews, we picked the hazelnuts.
Why?
It’s close! This one’s interesting…
In terms of macros, hazelnuts have more fiber and fats, while cashews have more protein and carbs. All in all, all good stuff all around; maybe a win for one or the other depending on your priorities. We’d pick hazelnuts here, but your preference may vary.
When it comes to vitamins, hazelnuts have more of vitamins A, B1, B2, B3, B5, B6, B9, C, and E, while cashews have more vitamin K. An easy win for hazelnuts here, and the margins weren’t close.
In the category of minerals, hazelnuts have more calcium, manganese, and potassium, while cashews have more copper, iron, magnesium, phosphorus, selenium, and zinc. This is a win for cashews, but it’s worth noting that cup for cup, both of these nuts provide more than the daily requirement of most of those minerals. This means that in practical terms, it doesn’t matter too much that (for example), while cashews provide 732% of the daily requirement for copper, hazelnuts “only” provide 575%. So while this category remains a victory for cashews, it’s something of a “on paper” thing for the most part.
Adding up the sections (ambivalent + clear win for hazelnuts + nominal win for cashews) means that in total today we’re calling it in favour of hazelnuts… But as ever, enjoy both, because both are good and so is diversity!
Want to learn more?
You might like to read:
Why You Should Diversify Your Nuts
Take care!
Share This Post
Related Posts
-
Don’t Do *This* If You’re Over 50 (And Want Better Sleep)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Michael Breus, sleep specialist, explains:
Don’t make these mistakes
Dr. Breus recommends avoiding…
- Misusing magnesium: magnesium is a helpful sleep aid but must be carefully monitored. Recommended doses are 250mg for women and 300–350 mg for men, with slight adjustments for hot climates or active lifestyles. Overdosing can cause stomach issues, diarrhea, and dehydration, disrupting sleep. He recommends starting with magnesium glycinate for fewer stomach issues, and later mix with magnesium citrate. Always check supplements to avoid excessive magnesium intake.
- Misusing melatonin: melatonin production declines after age 55–60, making low-dose supplementation (0.5–1 mg) beneficial. He recommends, however, avoiding high doses (3–10mg), and he recommends to take it 90 minutes before bedtime. Melatonin interacts with some medications (including some meds for blood pressure or depression), so consult a pharmacist before use to avoid risks like serotonin syndrome.
- Going to bed too early: going to bed too early disrupts circadian rhythms and reduces sleep drive, causing earlier waking. Now, being an “early bird” is a generally healthy thing, but if you’re already getting up at 5am, say, you probably want your schedule to not continue to creep further forwards until you become nocturnal. Set a consistent wake-up time and count 7.5 hours backward (plus a set time to fall asleep, e.g. 20 minutes, but you’ll know what it is for you) to determine bedtime.
- Excessive caffeine consumption: from the heading, it may seem like a no-brainer, but older adults metabolize caffeine 33% slower on average, prolonging its effects. Dr. Breus recommends to reduce intake with “caffeine fading,” switching to half-caffeinated coffee for a while and then considering transitioning to decaf. He also suggests enjoying increasingly lower-caffeine teas, like black tea in the morning, matcha in the afternoon, and herbal tea at night to reduce caffeine’s impact on sleep.
- Falling foul of serotonin: avoid taking 5-HTP supplements with SSRI antidepressants like Prozac or Zoloft due to the risk of serotonin syndrome.
- Consider checking for physical problems: if you regularly wake up tired and/or groggy (despite having ostensibly had enough sleep, and there not being a pharmaceutical explanation for your grogginess), consider screening for sleep apnea. Home sleep tests are a convenient way to identify and treat this common but often undiagnosed condition.
For more on each of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like:
How to Fall Asleep Faster: CBT-Insomnia Treatment
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Cabbage vs Cauliflower – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing cabbage to cauliflower, we picked the cauliflower.
Why?
First, let’s note: these are two different cultivars of the same species (Brassica oleracea) and/but as usual (we say, as there are a lot of cultivars of Brassica oleracea, and we’ve done a fair few pairings of them before) there are still nutritional differences to consider, such as…
In terms of macros, cabbage has very slightly more carbs and fiber, while cauliflower has very slightly more protein. However, the numbers are all so close (and the glycemic index equal), such that we’re going to call the macros category a tie.
In the category of vitamins, cabbage has more of vitamins A, B1, E, and K, while cauliflower has more of vitamins B2, B3, B5, B6, B7, B9, C, and choline. Superficially, this is a clear 8:4 win for cauliflower; it’s worth noting though that the differences in amounts are mostly small, so this isn’t as big a win as it looks like. Still a win for cauliflower, though.
When it comes to minerals, it’s a similar story: cabbage has a little more calcium, iron, and manganese, while cauliflower has a little more copper, magnesium, phosphorus, potassium, and zinc. This time a 6:3 win for cauliflower, and again, the margins are small so there’s really not as much between them as it looks like. Still a win for cauliflower, though.
In short: enjoy either or both (diversity is good), but the most nutritionally dense is cauliflower, even if cabbage isn’t far behind it.
Want to learn more?
You might like to read:
What’s Your Plant Diversity Score?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Shoulders Range – by Elia Bartolini
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Shoulder flexibility and mobility can be a big deal, especially when it starts to decline—more so than other kinds of flexibility. Most seniors can get through the day without doing the splits against a wall, for example, but shoulder tightness can be more of a problem if you can’t easily get into or out of your clothes.
If you think it couldn’t happen to you: the great Jane Fonda has a now-famous photoset of her looking glamorous in a dress at a red carpet event, and then looking frazzled making breakfast in the same dress in her kitchen the next morning, because, as she wrote, “I couldn’t get my dress unzipped so I slept in it”.
Now, “to avoid ending up like Jane Fonda” is not a series of words that usually precedes advice, but in this case: this book delves into the science of one of the most quirky joints of the human body, and how to leverage this to maximize shoulder mobility, while maintaining adequate strength (because flexibility without strength is just asking for a dislocation) without doing anything that would actually bulk up our shoulders, because it’s just about progressing through passive, active, and tensed stretching, static, dynamic, and loaded stretching, as well as PNF stretching and antagonist stretching.
If that seems like a lot of stretching, don’t worry; the author presents a series of workouts that will take us through these stretches in a very small amount of time each day.
The style is instructional like a textbook, with clear diagrams where appropriate, and lots of callout boxes, bullet points, emboldening for key points, etc. It all makes for every easy learning.
Bottom line: if you’d like to improve and maintain your shoulder mobility, this is an excellent book for that.
Click here to check out Shoulders Range, and perfect your shoulders and upper body flexibility!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: