Bamboo Shoots vs Asparagus – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing bamboo shoots to asparagus, we picked the asparagus.
Why?
Both are great! But asparagus does distinguish itself on nutritional density.
In terms of macros, bamboo starts strong with more protein and fiber, but it’s not a huge amount more; the margins of difference are quite small.
In the category of vitamins, asparagus wins easily with more of vitamins A, B2, B3, B5, B9, C, E, K, and choline. In contrast, bamboo boasts only more vitamin B6. A clear win for asparagus.
The minerals line-up is closer; asparagus has more calcium, iron, magnesium, and selenium, while bamboo shoots have more manganese, phosphorus, potassium, and zinc. That’s a 4:4 tie, but asparagus’s margins of difference are larger, and if we need a further tiebreaker, bamboo also contains more sodium, which most people in the industrialized world could do with less of rather than more. So, a small win for asparagus.
In short, adding up the sections… Bamboo shoots, but asparagus scores, and wins the day. Enjoy both, of course, but if making a pick, then asparagus has more bang-for-buck.
Want to learn more?
You might like to read:
Asparagus vs Eggplant – Which is Healthier?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Can you drink your fruit and vegetables? How does juice compare to the whole food?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Do you struggle to eat your fruits and vegetables? You are not alone. Less than 5% of Australians eat the recommended serves of fresh produce each day (with 44% eating enough fruit but only 6% eating the recommended vegetables).
Adults should aim to eat at least five serves of vegetables (or roughly 375 grams) and two serves of fruit (about 300 grams) each day. Fruits and vegetables help keep us healthy because they have lots of nutrients (vitamins, minerals and fibre) and health-promoting bioactive compounds (substances not technically essential but which have health benefits) without having many calories.
So, if you are having trouble eating the rainbow, you might be wondering – is it OK to drink your fruits and vegetables instead in a juice or smoothie? Like everything in nutrition, the answer is all about context.
Darina Belonogova/Pexels It might help overcome barriers
Common reasons for not eating enough fruits and vegetables are preferences, habits, perishability, cost, availability, time and poor cooking skills. Drinking your fruits and vegetables in juices or smoothies can help overcome some of these barriers.
Juicing or blending can help disguise tastes you don’t like, like bitterness in vegetables. And it can blitz imperfections such as bruises or soft spots. Preparation doesn’t take much skill or time, particularly if you just have to pour store-bought juice from the bottle. Treating for food safety and shipping time does change the make up of juices slightly, but unsweetened juices still remain significant sources of nutrients and beneficial bioactives.
Juicing can extend shelf life and reduce the cost of nutrients. In fact, when researchers looked at the density of nutrients relative to the costs of common foods, fruit juice was the top performer.
So, drinking my fruits and veggies counts as a serve, right?
How juice is positioned in healthy eating recommendations is a bit confusing. The Australian Dietary Guidelines include 100% fruit juice with fruit but vegetable juice isn’t mentioned. This is likely because vegetable juices weren’t as common in 2013 when the guidelines were last revised.
The guidelines also warn against having juice too often or in too high amounts. This appears to be based on the logic that juice is similar, but not quite as good as, whole fruit. Juice has lower levels of fibre compared to fruits, with fibre important for gut health, heart health and promoting feelings of fullness. Juice and smoothies also release the sugar from the fruit’s other structures, making them “free”. The World Health Organization recommends we limit free sugars for good health.
But fruit and vegetables are more than just the sum of their parts. When we take a “reductionist” approach to nutrition, foods and drinks are judged based on assumptions made about limited features such as sugar content or specific vitamins.
But these features might not have the impact we logically assume because of the complexity of foods and people. When humans eat varied and complex diets, we don’t necessarily need to be concerned that some foods are lower in fibre than others. Juice can retain the nutrients and bioactive compounds of fruit and vegetables and even add more because parts of the fruit we don’t normally eat, like the skin, can be included.
Juicing or blending might mean you eat different parts of the fruit or vegetable. flyingv3/Shutterstock So, it is healthy then?
A recent umbrella review of meta-analyses (a type of research that combines data from multiple studies of multiple outcomes into one paper looked at the relationship between 100% juice and a range of health outcomes.
Most of the evidence showed juice had a neutral impact on health (meaning no impact) or a positive one. Pure 100% juice was linked to improved heart health and inflammatory markers and wasn’t clearly linked to weight gain, multiple cancer types or metabolic markers (such as blood sugar levels).
Some health risks linked to drinking juice were reported: death from heart disease, prostate cancer and diabetes risk. But the risks were all reported in observational studies, where researchers look at data from groups of people collected over time. These are not controlled and do not record consumption in the moment. So other drinks people think of as 100% fruit juice (such as sugar-sweetened juices or cordials) might accidentally be counted as 100% fruit juice. These types of studies are not good at showing the direct causes of illness or death.
What about my teeth?
The common belief juice damages teeth might not stack up. Studies that show juice damages teeth often lump 100% juice in with sweetened drinks. Or they use model systems like fake mouths that don’t match how people drinks juice in real life. Some use extreme scenarios like sipping on large volumes of drink frequently over long periods of time.
Juice is acidic and does contain sugars, but it is possible proper oral hygiene, including rinsing, cleaning and using straws can mitigate these risks.
Again, reducing juice to its acid level misses the rest of the story, including the nutrients and bioactives contained in juice that are beneficial to oral health.
Juice might be more convenient and could replace less healthy drinks. PintoArt/Shutterstock So, what should I do?
Comparing whole fruit (a food) to juice (a drink) can be problematic. They serve different culinary purposes, so aren’t really interchangeable.
The Australian Guide to Healthy Eating recommends water as the preferred beverage but this assumes you are getting all your essential nutrients from eating.
Where juice fits in your diet depends on what you are eating and what other drinks it is replacing. Juice might replace water in the context of a “perfect” diet. Or juice might replace alcohol or sugary soft drinks and make the relative benefits look very different.
On balance
Whether you want to eat your fruits and vegetables or drink them comes down to what works for you, how it fits into the context of your diet and your life.
Smoothies and juices aren’t a silver bullet, and there is no evidence they work as a “cleanse” or detox. But, with society’s low levels of fruit and vegetable eating, having the option to access nutrients and bioactives in a cheap, easy and tasty way shouldn’t be discouraged either.
Emma Beckett, Adjunct Senior Lecturer, Nutrition, Dietetics & Food Innovation – School of Health Sciences, UNSW Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Relationships: When To Stick It Out & When To Call It Quits
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Like A Ship Loves An Anchor?
Today’s article may seem a little bit of a downer to start with, but don’t worry, it picks up again too. Simply put, we’ve written before about many of the good parts of relationships, e.g:
Only One Kind Of Relationship Promotes Longevity This Much!
…but what if that’s not what we have?
Note: if you have a very happy, secure, fulfilling, joyous relationship, then, great! Or if you’re single and happy, then, also great! Hopefully you will still find today’s feature of use if you find yourself advising a friend or family member one day. So without further ado, let’s get to it…
You may be familiar with the “sunk cost fallacy”; if not: it’s what happens when a person or group has already invested into a given thing, such that even though the thing is not going at all the way they hoped, they now want to continue trying to make that thing work, lest their previous investment be lost. But the truth is: if it’s not going to work, then the initial investment is already lost, and pouring out extra won’t help—it’ll just lose more.
That “investment” in a given thing could be money, time, energy, or (often the case) a combination of the above.
In the field of romance, the “sunk cost fallacy” keeps a lot of bad relationships going for longer than perhaps they should, and looking back (perhaps after a short adjustment period), the newly-single person says “why did I let that go on?” and vows to not make the same mistake again.
But that prompts the question: how can we know when it’s right to “keep working on it, because relationships do involve work”, as perfectly reasonable relationship advice often goes, and when it’s right to call it quits?
Should I stay or should I go?
Some questions for you (or perhaps a friend you might find yourself advising) to consider:
- What qualities do you consider the most important for a partner to have—and does your partner have them?
- If you described the worst of your relationship to a close friend, would that friend feel bad for you?
- Do you miss your partner when they’re away, or are you glad of the break? When they return, are they still glad to see you?
- If you weren’t already in this relationship, would you seek to enter it now? (This takes away sunk cost and allows a more neutral assessment)
- Do you feel completely safe with your partner (emotionally as well as physically), or must you tread carefully to avoid conflict?
- If your partner decided tomorrow that they didn’t want to be with you anymore and left, would that be just a heartbreak, or an exciting beginning of a new chapter in your life?
- What things would you generally consider dealbreakers in a relationship—and has your partner done any of them?
The last one can be surprising, by the way. We often see or hear of other people’s adverse relationship situations and think “I would never allow…” yet when we are in a relationship and in love, there’s a good chance that we might indeed allow—or rather, excuse, overlook, and forgive.
And, patience and forgiveness certainly aren’t inherently bad traits to have—it’s just good to deploy them consciously, and not merely be a doormat.
Either way, reflect (or advise your friend/family member to reflect, as applicable) on the “score” from the above questions.
- If the score is good, then maybe it really is just a rough patch, and the tools we link at the top and bottom of this article might help.
- If the score is bad, the relationship is bad, and no amount of historic love or miles clocked up together will change that. Sometimes it’s not even anyone’s fault; sometimes a relationship just ran its course, and now it’s time to accept that and turn to a new chapter.
“At my age…”
As we get older, it’s easy for that sunk cost fallacy to loom large. Inertia is heavy, the mutual entanglement of lives is far-reaching, and we might not feel we have the same energy for dating that we did when we were younger.
And there may sometimes be a statistical argument for “sticking it out” at least for a while, depending on where we are in the relationship, per this study (with 165,039 participants aged 20–76), which found:
❝Results on mean levels indicated that relationship satisfaction decreased from age 20 to 40, reached a low point at age 40, then increased until age 65, and plateaued in late adulthood.
As regards the metric of relationship duration, relationship satisfaction decreased during the first 10 years of the relationship, reached a low point at 10 years, increased until 20 years, and then decreased again.❞
Source: Development of Relationship Satisfaction Across the Life Span: A Systematic Review and Meta-Analysis
And yet, when it comes to prospects for a new relationship…
- If our remaining life is growing shorter, then it’s definitely too short to spend in an unhappy relationship
- Maybe we really won’t find romance again… And maybe that’s ok, if w’re comfortable making our peace with that and finding joy in the rest of life (this widowed writer (hi, it’s me) plans to remain single now by preference, and her life is very full of purpose and beauty and joy and yes, even love—for family, friends, etc, plus the memory of my wonderful late beloved)
- Nevertheless, the simple fact is: many people do find what they go on to describe as their best relationship yet, late in life ← this study is with a small sample size, but in this case, even anecdotal evidence seems sufficient to make the claim reasonable; probably you personally know someone who has done so. If they can, so can you, if you so wish.
- Adding on to that last point… Later life relationships can also offer numerous significant advantages unique to such (albeit some different challenges too—but with the right person, those challenges are just a fun thing to tackle together). See for example:
An exploratory investigation into dating among later‐life women
And about those later-life relationships that do work? They look like this:
this one looks like the title says it all, but it really doesn’t, and it’s very much worth at least reading the abstract, if not the entire paper—because it talks a lot about the characteristics that make for happy or unhappy relationships, and the effect that those things have on people. It really is very good, and quite an easy read.
See again: Healthy Relationship, Healthy Life
Take care!
Share This Post
-
Synergistic Brain-Training
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Let The Games Begin (But It Matters What Kind)
Exercise is good for brain health; we’ve written about this before, for example:
How To Reduce Your Alzheimer’s Risk ← there are many advices here, but exercise, especially cardiovascular exercise in this case, is an important item on the list!
Today it’s Psychology Sunday though, and we’re going to talk about looking after brain health by means of brain-training, via games.
“Brain-training” gets a lot of hype and flak:
- Hype: do sudoku every day and soon you will have an IQ of 200 and still have a sharp wit at the age of 120
- Flak: brain-training is usually training only one kind of cognitive function, with limited transferability to the rest of life
The reality is somewhere between the two. Brain training really does improve not just outwardly measurable cognitive function, but also internally measurable improvements visible on brain scans, for example:
- Cognitive training modified age-related brain changes in older adults with subjective memory decline
- Functional brain changes associated with cognitive training in healthy older adults: A preliminary ALE meta-analysis
But what about the transferability?
Let us play
This is where game-based brain-training comes in. And, the more complex the game, the better the benefits, because there is more chance of applicability to life, e.g:
- Sudoku: very limited applicability
- Crosswords: language faculties
- Chess: spatial reasoning, critical path analysis, planning, memory, focus (also unlike the previous two, chess tends to be social for most people, and also involve a lot of reading, if one is keen)
- Computer games: wildly varied depending on the game. While an arcade-style “shoot-em-up” may do little for the brain, there is a lot of potential for a lot of much more relevant brain-training in other kinds of games: it could be planning, problem-solving, social dynamics, economics, things that mirror the day-to-day challenges of running a household, even, or a business.
- It’s not that the skills are useful, by the way. Playing “Stardew Valley” will not qualify you to run a real farm, nor will playing “Civilization” qualify you to run a country. But the brain functions used and trained? Those are important.
It becomes easily explicable, then, why these two research reviews with very similar titles got very different results:
- A Game a Day Keeps Cognitive Decline Away? A Systematic Review and Meta-Analysis of Commercially-Available Brain Training Programs in Healthy and Cognitively Impaired Older Adults
- Game-based brain training for improving cognitive function in community-dwelling older adults: A systematic review and meta-regression
The first review found that game-based brain-training had negligible actual use. The “games” they looked at? BrainGymmer, BrainHQ, CogMed, CogniFit, Dakim, Lumosity, and MyBrainTrainer. In other words, made-for-purpose brain-trainers, not actual computer games per se.
The second reviewfound that game-based training was very beneficial. The games they looked at? They didn’t name them, but based on the descriptions, they were actual multiplayer online turn-based computer games, not made-for-purpose brain-trainers.
To summarize the above in few words: multiplayer online turn-based computer games outperform made-for-purpose brain-trainers for cognitive improvement.
Bringing synergy
However, before you order that expensive gaming-chair for marathon gaming sessions (research suggests a tail-off in usefulness after about an hour of continuous gaming per session, by the way), be aware that cognitive training and (physical) exercise training combined, performed close in time to each other or simultaneously, perform better than the sum of either alone:
See also:
❝Simultaneous training was the most efficacious approach for cognition, followed by sequential combinations and cognitive training alone, and significantly better than physical exercise.
Our findings suggest that simultaneously and sequentially combined interventions are efficacious for promoting cognitive alongside physical health in older adults, and therefore should be preferred over implementation of single-domain training❞
~ Dr. Hanna Malmberg Gavelin et al.
Take care!
Share This Post
Related Posts
-
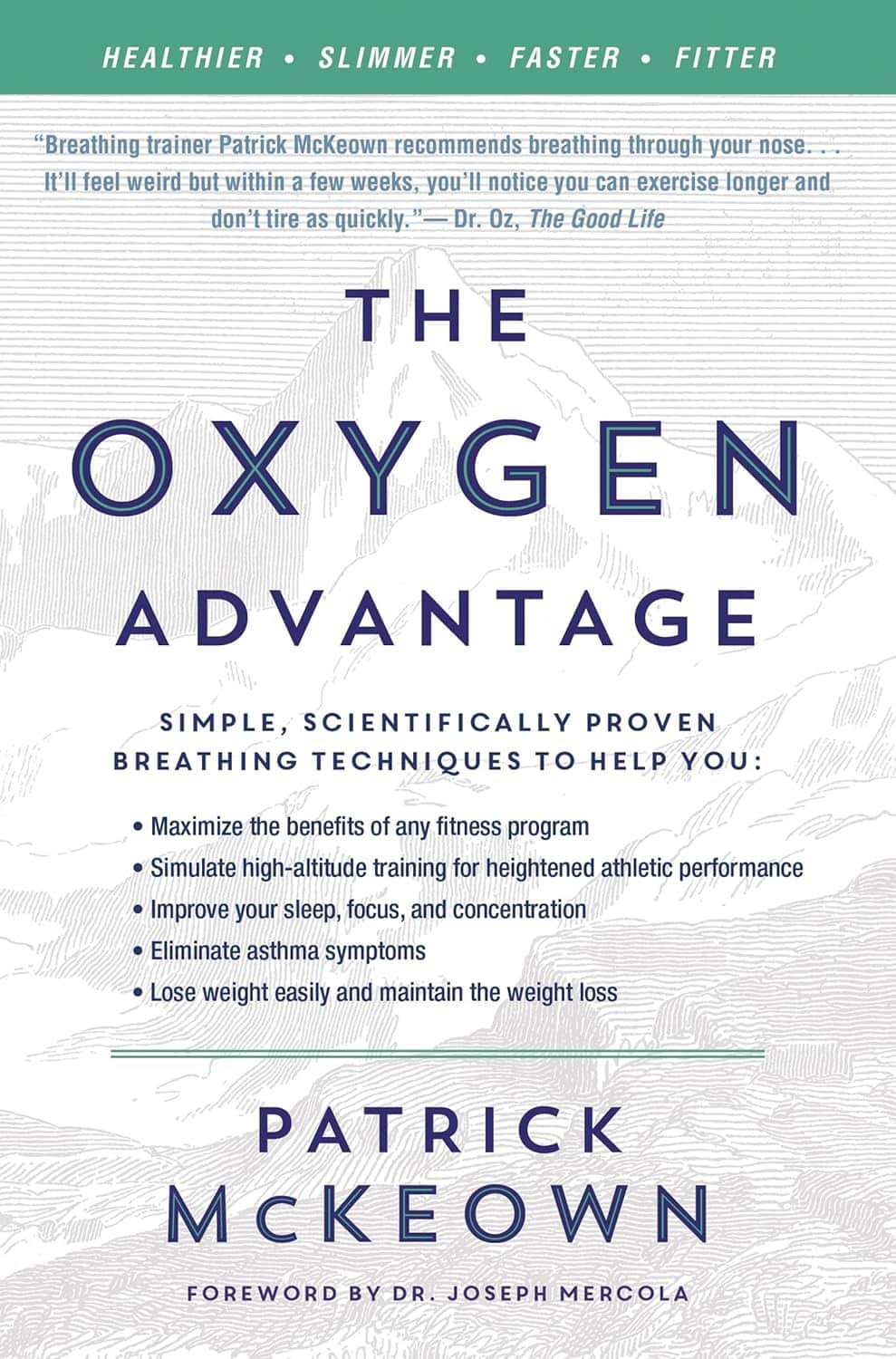
The Oxygen Advantage – by Patrick McKeown
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
You probably know to breathe through your nose, and use your diaphragm. What else does this book have to offer?
A lot of the book is aimed at fixing specific problems, and optimizing what can be optimized—including with tips and tricks you may not have encountered before. Yet, the offerings are not bizarre either; we don’t need to learn to breathe through our ears while drinking a glass of water upside down or anything.
Rather, such simple things as improving one’s VO₂Max by occasionally holding one’s breath while walking briskly. But, he advises specifically, this should be done by pausing the breath halfway through the exhalation (a discussion of the ensuing physiological response is forthcoming).
Little things like that are woven throughout the book, whose style is mostly anecdotal rather than hard science, yet is consistent with broad scientific consensus in any case.
Bottom line: if you’ve any reason to think your breathing might be anything less than the best it could possibly be, this book is likely to help you to tweak it to be a little better.
Click here to check out The Oxygen Advantage, and get yours!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
An unbroken night’s sleep is a myth. Here’s what good sleep looks like
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What do you imagine a good night’s sleep to be?
Often when people come into our sleep clinic seeking treatment, they share ideas about healthy sleep.
Many think when their head hits the pillow, they should fall into a deep and restorative sleep, and emerge after about eight hours feeling refreshed. They’re in good company – many Australians hold the same belief.
In reality, healthy sleep is cyclic across the night, as you move in and out of the different stages of sleep, often waking up several times. Some people remember one or more of these awakenings, others do not. Let’s consider what a healthy night’s sleep looks like.
Bricolage/Shutterstock Sleep cycles are a roller-coaster
As an adult, our sleep moves through different cycles and brief awakenings during the night. Sleep cycles last roughly 90 minutes each.
We typically start the night with lighter sleep, before moving into deeper sleep stages, and rising again into rapid eye movement (REM) sleep – the stage of sleep often linked to vivid dreaming.
If sleeping well, we get most of our deep sleep in the first half of the night, with REM sleep more common in the second half of the night.
Deepest sleep usually happens during the first half of the night. Verin/Shutterstock Adults usually move through five or six sleep cycles in a night, and it is entirely normal to wake up briefly at the end of each one. That means we might be waking up five times during the night. This can increase with older age and still be healthy. If you’re not remembering these awakenings that’s OK – they can be quite brief.
What does getting a ‘good’ sleep actually mean?
You’ll often hear that adults need between seven and nine hours of sleep per night. But good sleep is about more than the number of hours – it’s also about the quality.
For most people, sleeping well means being able to fall asleep soon after getting into bed (within around 30 minutes), sleeping without waking up for long periods, and waking feeling rested and ready for the day.
You shouldn’t be feeling excessively sleepy during the day, especially if you’re regularly getting at least seven hours of refreshing sleep a night (this is a rough rule of thumb).
But are you noticing you’re feeling physically tired, needing to nap regularly and still not feeling refreshed? It may be worthwhile touching base with your general practitioner, as there a range of possible reasons.
Common issues
Sleep disorders are common. Up to 25% of adults have insomnia, a sleep disorder where it may be hard to fall or stay asleep, or you may wake earlier in the morning than you’d like.
Rates of common sleep disorders such as insomnia and sleep apnoea – where your breathing can partially or completely stop many times during the night – also increase with age, affecting 20% of early adults and 40% of people in middle age. There are effective treatments, so asking for help is important.
Beyond sleep disorders, our sleep can also be disrupted by chronic health conditions – such as pain – and by certain medications.
There can also be other reasons we’re not sleeping well. Some of us are woken by children, pets or traffic noise during the night. These “forced awakenings” mean we may find it harder to get up in the morning, take longer to leave bed and feel less satisfied with our sleep. For some people, night awakenings may have no clear cause.
A good way to tell if these awakenings are a problem for you is by thinking about how they affect you. When they cause feelings of frustration or worry, or are impacting how we feel and function during the day, it might be a sign to seek some help.
If waking up in the night is interfering with your normal day-to-day activities, it may indicate a problem. BearFotos/Shutterstock We also may struggle to get up in the morning. This could be for a range of reasons, including not sleeping long enough, going to bed or waking up at irregular times – or even your own internal clock, which can influence the time your body prefers to sleep.
If you’re regularly struggling to get up for work or family needs, it can be an indication you may need to seek help. Some of these factors can be explored with a sleep psychologist if they are causing concern.
Can my smart watch help?
It is important to remember sleep-tracking devices can vary in accuracy for looking at the different sleep stages. While they can give a rough estimate, they are not a perfect measure.
In-laboratory polysomnography, or PSG, is the best standard measure to examine your sleep stages. A PSG examines breathing, oxygen saturation, brain waves and heart rate during sleep.
Rather than closely examining nightly data (including sleep stages) from a sleep tracker, it may be more helpful to look at the patterns of your sleep (bed and wake times) over time.
Understanding your sleep patterns may help identify and adjust behaviours that negatively impact your sleep, such as your bedtime routine and sleeping environment.
And if you find viewing your sleep data is making you feel worried about your sleep, this may not be useful for you. Most importantly, if you are concerned it is important to discuss it with your GP who can refer you to the appropriate specialist sleep health provider.
Amy Reynolds, Associate Professor in Clinical Sleep Health, Flinders University; Claire Dunbar, Research Associate, Sleep Health, Flinders University; Gorica Micic, Postdoctoral Research Fellow, Clinical Psychologist, Flinders University; Hannah Scott, Research Fellow in Sleep Health, Flinders University, and Nicole Lovato, Associate Professor, Adelaide Institute for Sleep Health, Flinders University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Antihistamines’ Generation Gap
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Are You Ready For Allergy Season?
For those of us in the Northern Hemisphere, fall will be upon us soon, and we have a few weeks to be ready for it. A common seasonal ailment is of course seasonal allergies—it’s not serious for most of us, but it can be very annoying, and can disrupt a lot of our normal activities.
Suddenly, a thing that notionally does us no real harm, is making driving dangerous, cooking take three times as long, sex laughable if not off-the-table (so to speak), and the lightest tasks exhausting.
So, what to do about it?
Antihistamines: first generation
Ye olde antihistamines such as diphenhydramine and chlorpheniramine are probably not what to do about it.
They are small molecules that cross the blood-brain barrier and affect histamine receptors in the central nervous system. This will generally get the job done, but there’s a fair bit of neurological friendly-fire going on, and while they will produce drowsiness, the sleep will usually be of poor quality. They also tax the liver rather.
If you are using them and not experiencing unwanted side effects, then don’t let us stop you, but do be aware of the risks.
See also: Long-term use of diphenhydramine ← this is the active ingredient in Benadryl in the US and Canada, but safety regulations in many other countries mean that Benadryl has different, safer active ingredients elsewhere.
Antihistamines: later generations
We’re going to aggregate 2nd gen, 3rd gen, and 4th gen antihistamines here, because otherwise we’ll be writing a history article and we don’t have room for that. But suffice it to say, later generations of antihistamines do not come with the same problems.
Instead of going in all-guns-blazing to the CNS like first-gens, they are more specific in their receptor-targetting, resulting in negligible collateral damage:
Special shout-out to cetirizine and loratadine, which are the drugs behind half the brand names you’ll see on pharmacy shelves around most of the world these days (including many in the US and Canada).
Note that these two are very often discussed in the same sentence, sit next to each other on the shelf, and often have identical price and near-identical packaging. Their effectiveness (usually: moderate) and side effects (usually: low) are similar and comparable, but they are genuinely different drugs that just happen to do more or less the same thing.
This is relevant because if one of them isn’t working for you (and/or is creating an unwanted side effect), you might want to try the other one.
Another honorable mention goes to fexofenadine, for which pretty much all the same as the above goes, though it gets talked about less (and when it does get mentioned, it’s usually by its most popular brand name, Allegra).
Finally, one that’s a little different and also deserving of a special mention is azelastine. It was recently (ish, 2021) moved from being prescription-only to being non-prescription (OTC), and it’s a nasal spray.
It can cause drowsiness, but it’s considered safe and effective for most people. Its main benefit is not really the difference in drug, so much as the difference in the route of administration (nasal rather than oral). Because the drug is in liquid spray form, it can be absorbed through the mucus lining of the nose and get straight to work on blocking the symptoms—in contrast, oral antihistamines usually have to go into your stomach and take their chances there (we say “usually”, because there are some sublingual antihistamines that dissolve under the tongue, but they are less common.)
Better than antihistamines?
Writer’s note: at this point, I was given to wonder: “wait, what was I squirting up my nose last time anyway?”—because, dear readers, at the time I got it I just bought one of every different drug on the shelf, desperate to find something that worked. What worked for me, like magic, when nothing else had, was beclometasone dipropionate, which a) smelled delightfully of flowers, which might just be the brand I got, b) needs replacing now because I got it in March 2023 and it expired July 2024, and c) is not an antihistamine at all.
But, that brings us to the final chapter for today: systemic corticosteroids
They’re not ok for everyone (check with your doctor if unsure), and definitely should not be taken if immunocompromised and/or currently suffering from an infection (including colds, flu, COVID, etc) unless your doctor tells you otherwise (and even then, honestly, double-check).
But! They can work like magic when other things don’t. Unlike antihistamines, which only block the symptoms, systemic corticosteroids tackle the underlying inflammation, which can stop the whole thing in its tracks.
Here’s how they measure up against antihistamines:
❝The results of this systematic review, together with data on safety and cost effectiveness, support the use of intranasal corticosteroids over oral antihistamines as first line treatment for allergic rhinitis.❞
~ Dr. Robert Puy et al.
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: