Antihistamines for Runny Nose?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small 😎
❝Do you have any articles about using Anti-Histamines? My nose seems to be running a lot. I don’t have a cold or any allergies that I know of. I tried a Nasal spray Astepro, but it doesn’t do much.?❞
Just for you, we wrote such an article yesterday in response to this question!
The Astepro that you tried, by the way, is a brand name of the azelastine we mentioned near the end, before we got to talking about systemic corticosteroids such as beclometasone dipropionate—this latter might help you if antihistamines haven’t, and if your doctor advises there’s no contraindication (for most people it is safe for there are exceptions, such as if you are immunocompromised and/or currently fighting some infection).
You can find more details on all this in yesterday’s article, which in case you missed it, can be found at:
Antihistamines’ Generation Gap: Are You Ready For Allergy Season?
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
What Do The Different Kinds Of Fiber Do? 30 Foods That Rank Highest
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve talked before about how important fiber is:
Why You’re Probably Not Getting Enough Fiber (And How To Fix It)
And even how it’s arguably the most important dietary factor when it comes to avoiding heart disease:
What Matters Most For Your Heart? Eat More (Of This) For Lower Blood Pressure ← Spoiler: it’s fiber
And yes, that’s even when considered alongside other (also laudable) dietary interventions such as lowering intake of sodium, various kinds of saturated fat, and red meat.
So, what should we know about fiber, aside from “aim to get nearer 40g/day instead of the US average 16g/day”?
Soluble vs Insoluble
The first main way that dietary fibers can be categorized is soluble vs insoluble. Part of the difference is obvious, but bear with us, because there’s more to know about each:
- Soluble fiber dissolves (what a surprise) in water and, which part is important, forms a gel. This slows down things going through your intestines, which is important for proper digestion and absorption of nutrients (as well as avoiding diarrhea). Yes, you heard right: getting enough of the right kind of fiber helps you avoid diarrhea.
- Insoluble fiber does not dissolve (how shocking) in water and thus mostly passes through undigested by us (some will actually be digested by gut microbes who subsist on this, and in return for us feeding them daily, they make useful chemicals for us). This kind of fiber is also critical for healthy bowel movements, because without it, constipation can ensue.
Both kinds of fiber improve just about every metric related to blood, including improving triglycerides and improving insulin sensitivity and blood glucose levels. Thus, they help guard against various kinds of cardiovascular disease, diabetes, and metabolic disease in general. Do note that because whatever’s good for your heart/blood is good for your brain (which requires a healthy heart and bloodstream to nourish it and take away waste), likely this also has a knock-on effect against cognitive decline, but we don’t have hard science for that claim so we’re going to leave that last item as a “likely”.
However, one thing’s for sure: if you want a healthy gut, heart, and brain, you need a good balance of soluble and insoluble fibers.
10 of the best for soluble fiber
Food Soluble Fiber Type(s) Soluble Fiber (g per serving) Insoluble Fiber Type(s) Insoluble Fiber (g per serving) Total Fiber (g per serving) Kidney beans (1 cup cooked) Pectin, Resistant Starch 1.5–2 Hemicellulose, Cellulose 6 8 Lentils (1 cup cooked) Pectin, Resistant Starch 1.5–2 Cellulose 6 7.5 Barley (1 cup cooked) Beta-glucan 3–4 Hemicellulose 2 6 Brussels sprouts (1 cup cooked) Pectin 1–1.5 Cellulose, Hemicellulose 2 3.5 Oats (1 cup cooked) Beta-glucan 2–3 Cellulose 1 3 Apples (1 medium) Pectin 1–2 Cellulose, Hemicellulose 2 3 Carrots (1 cup raw) Pectin 1–1.5 Cellulose, Hemicellulose 2 3 Citrus fruits (orange, 1 medium) Pectin 1–1.5 Cellulose 1 2.5 Flaxseeds (2 tbsp) Mucilage, Lignin 1–1.5 Cellulose 1 2.5 Psyllium husk (1 tbsp) Mucilage 3–4 Trace amounts 0 3–4 10 of the best for insoluble fiber
Food Soluble Fiber Type(s) Soluble Fiber (g per serving) Insoluble Fiber Type(s) Insoluble Fiber (g per serving) Total Fiber (g per serving) Wheat bran (1 cup) Trace amounts 0 Cellulose, Lignin 6–8 6–8 Black beans (1 cup cooked) Pectin, Resistant Starch 1.5 Cellulose 6 7.5 Brown rice (1 cup cooked) Trace amounts 0.5 Hemicellulose, Lignin 2–3 2.5–3.5 Popcorn (3 cups popped) Trace amounts 0.5 Hemicellulose 3 3.5 Broccoli (1 cup cooked) Pectin 1 Cellulose, Hemicellulose 4 5 Green beans (1 cup cooked) Trace amounts 0.5 Cellulose, Hemicellulose 3 3.5 Sweet potatoes (1 cup cooked) Pectin 1–1.5 Cellulose 3 4.5 Whole wheat bread (1 slice) Trace amounts 0.5 Cellulose, Hemicellulose 1 1.5 Pears (1 medium) Pectin 1 Cellulose, Hemicellulose 4 5 Almonds (1 oz) Trace amounts 0.5 Cellulose, Hemicellulose 2 2.5 10 of the best for a balance of both
Food Soluble Fiber Type(s) Soluble Fiber (g per serving) Insoluble Fiber Type(s) Insoluble Fiber (g per serving) Total Fiber (g per serving) Raspberries (1 cup) Pectin 1 Cellulose 5 6 Edamame (1 cup cooked) Pectin 1 Cellulose 5 6 Chia seeds (2 tbsp) Mucilage, Pectin 2–3 Lignin, Cellulose 3 5.5 Artichokes (1 medium) Inulin 1 Cellulose, Hemicellulose 5 6 Avocado (1 medium) Pectin ~2 Cellulose 4 6 Black beans (1 cup cooked) Pectin, Resistant Starch 1.5 Cellulose 6 7.5 Quinoa (1 cup cooked) Pectin, Saponins 1 Cellulose, Hemicellulose 3 4 Spinach (1 cup cooked) Pectin 0.5 Cellulose, Lignin 3 3.5 Prunes (1/2 cup) Pectin, Sorbitol 2 Cellulose 4 6 Figs (3 medium) Pectin 1 Cellulose 2 3 You’ll notice that the above “balance” is not equal; that’s ok; we need greater quantities of insoluble than soluble anyway, so it is as well that nature provides such.
This is the same kind of balance when we talk about “balanced hormones” (does not mean all hormones are in equal amounts; means they are in the right proportions) or “balanced microbiome” (does not mean that pathogens and friendly bacteria are in equal numbers), etc.
Some notes on the above:
About those fiber types, some of the most important soluble ones to aim for are:
- Beta-glucan: found in oats and barley, it supports heart health.
- Pectin: found in fruits like apples, citrus, and pears, it helps with cholesterol control.
- Inulin: a type of prebiotic fiber found in artichokes.
- Lignin: found in seeds and wheat bran, it has antioxidant properties.
- Resistant starch: found in beans and lentils, it acts as a prebiotic for gut health.
See also: When Is A Fiber Not A Fiber? The Food Additive You Do Want
One fiber to rule them all
Well, not entirely (we still need the others) but there is a best all-rounder:
The Best Kind Of Fiber For Overall Health?
Enjoy!
Share This Post
-
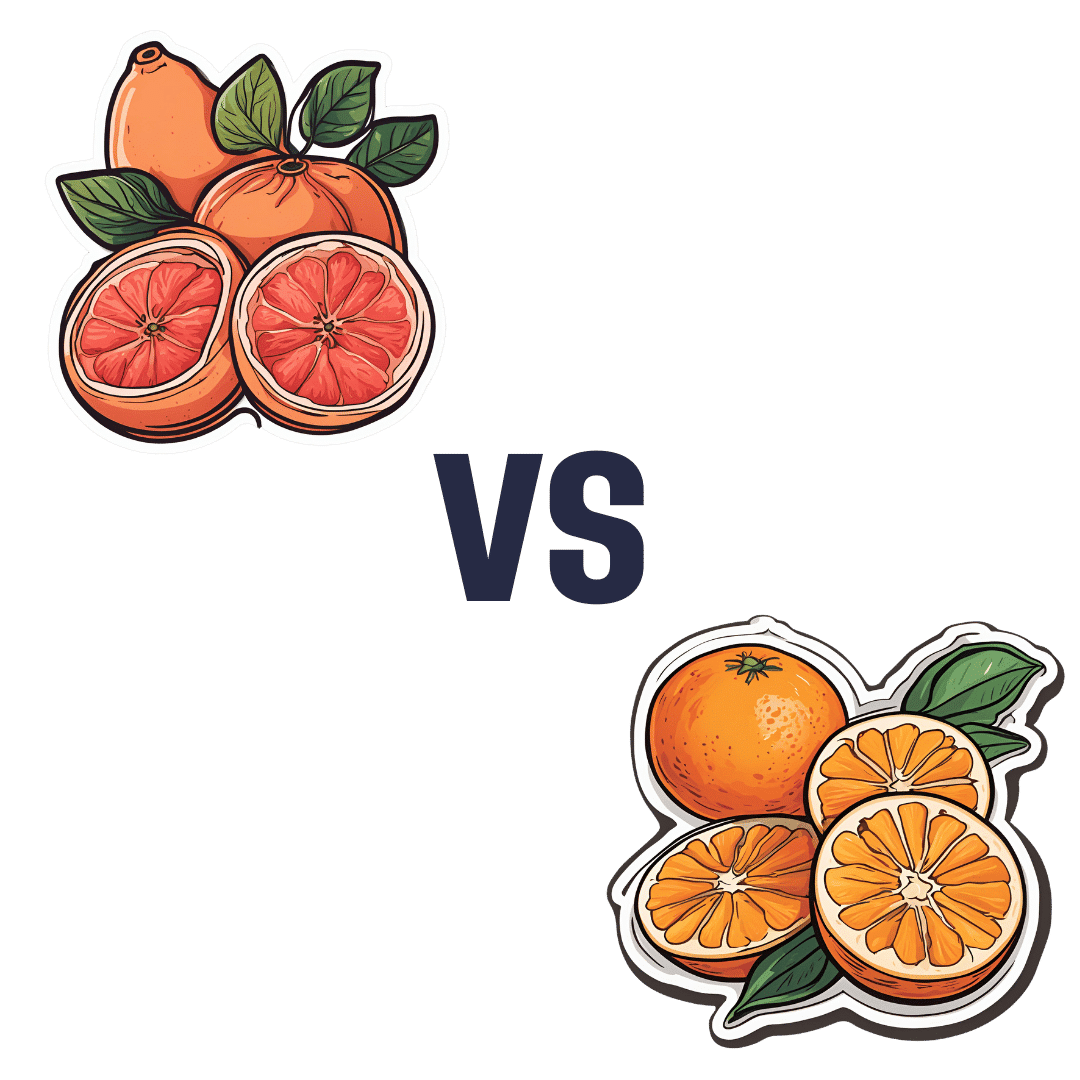
Grapefruit vs Orange – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing grapefruit to orange, we picked the orange.
Why?
It’s easy, when guessing which is the healthier out of two things, to guess that the more expensive or perhaps less universally available one is the healthier. But it’s not always so, and today is one of those cases!
In terms of macros, they are very similar fruits, with almost identical levels of carbohydrates, proteins, and fats, as well as water. Looking more carefully, we find that grapefruit’s sugars contain a slightly high proportion of fructose; not enough to make it unhealthy by any means (indeed, no whole unprocessed fruit is unhealthy unless it’s literally poisonous), but it is a thing to note if we’re micro-analysing the macronutrients. Also, oranges have slightly more fiber, which is always a plus.
When it comes to vitamins, oranges stand out with more of vitamins B1, B2, B3, B6, B9, C, and E, while grapefruit boasts more vitamin A (hence its color). Still, we’re calling this category another win for oranges.
In the category of minerals, oranges again sweep with more calcium, copper, iron, magnesium, manganese, potassium, and selenium, while grapefruit has just a little more phosphorus. So, another easy win for oranges.
One final consideration that’s not shown in the nutritional values, is that grapefruit contains furanocoumarin, which can inhibit cytochrome P-450 3A4 isoenzyme and P-glycoptrotein transporters in the intestine and liver—slowing down their drug metabolism capabilities, thus effectively increasing the bioavailability of many drugs manifold. It can also be found in lower quantities in Seville (sour) oranges, and it’s not present (or at least, if it is, it’s in truly tiny quantities) in most oranges.
This may sound superficially like a good thing (improving bioavailability of things we want), but in practice it means that in the case of many drugs, if you take them with (or near in time to) grapefruit or grapefruit juice, then congratulations, you just took an overdose. This happens with a lot of meds for blood pressure, cholesterol (including statins), calcium channel-blockers, anti-depressants, benzo-family drugs, beta-blockers, and more. Oh, and Viagra, too. Which latter might sound funny, but remember, Viagra’s mechanism of action is blood pressure modulation, and that is not something you want to mess around with unduly. So, do check with your pharmacist to know if you’re on any meds that would be affected by grapefruit or grapefruit juice!
All in all, today’s sections add up to an overwhelming win for oranges!
Want to learn more?
You might like to read:
Take care!
Share This Post
-
How To Rebuild Your Neurons’ Myelin Sheaths
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
PS: We Love You
Phosphatidylserine, or “PS” for short, is a phospholipid found in the brain. In other words, a kind of fatty compound that is such stuff as our brains are made of.
In particular, it’s required for healthy nerve cell membranes and myelin (the protective sheath that neurons live in—basically, myelin sheaths do for neurons what telomere caps do for DNA).
For an overview that’s more comprehensive than we have room for here, check out:
Phosphatidylserine and the human brain
Many people take it as a supplement.
Does taking it as a supplement work?
This is a valid question, as a lot of supplements can’t be absorbed well, and/or can’t pass the blood-brain barrier. But, as the above-linked study notes:
❝Exogenous PS (300-800 mg/d) is absorbed efficiently in humans, crosses the blood-brain barrier, and safely slows, halts, or reverses biochemical alterations and structural deterioration in nerve cells. It supports human cognitive functions, including the formation of short-term memory, the consolidation of long-term memory, the ability to create new memories, the ability to retrieve memories, the ability to learn and recall information, the ability to focus attention and concentrate, the ability to reason and solve problems, language skills, and the ability to communicate. It also supports locomotor functions, especially rapid reactions and reflexes.❞
(“Exogenous” means “coming from outside of the body”, as opposed to “endogenous”, meaning “made inside the body”. Effectively, in this context “exogenous” means “taken as a supplement”.)
Why do people take it?
The health claims for phosphatidylserine fall into two main categories:
- Neuroprotection (helping your brain to avoid age-related decline in the long term)
- Cognitive enhancement (helping your brain work better in the short term)
What does the science say?
There’s a lot of science that’s been done on the neuroprotective properties of PS, and there are thousands of studies we could draw from here. The upshot is that regular phosphatidylserine supplementation (most often 300mg/day, but studies are also found for 100–500mg/day) is strongly associated with a reduction in cognitive decline over the course of 12 weeks (a common study duration). Here are a some spotlight studies showing this:
- Effects of phosphatidylserine in Alzheimer’s disease
- Double-blind cross-over study of phosphatidylserine vs. placebo in patients with early dementia of the Alzheimer type
- Effect of Phosphatidylserine on Cerebral Glucose Metabolism in Alzheimer’s Disease
- The effect of soybean-derived phosphatidylserine on cognitive performance in elderly with subjective memory complaints
Note: PS can be derived from various sources, with the two most common forms being bovine (i.e., from cow brains) or soy-derived.
There is no established difference in the efficacy of these.
There have been some concerns raised about the risk of CJD (the human form of BSE, as in “mad cow disease”) from consuming brain matter from cows, but studies have not found any evidence of this actually happening.
There is also some evidence that phosphatidyserine significantly boosts cognitive performance, even in young people with no extant cognitive decline, for example:
(as the title suggests, they did also test for its effect on mood and endocrine response, but found it made no difference to those, just the cognitive function—which enjoyed a boost before exercise, as well as after it, meaning that the boost wasn’t dependent on the exercise)
PS for cognitive enhancement in the young and healthy is not nearly so well-explored as its use as a later-life guard against age-related cognitive decline. However, just because the studies in younger people are dwarfed in number by the studies in older people, doesn’t detract from the validity of the studies in younger people.
Basically: its use in older people has been studied the most, but all available evidence points to it being beneficial to brain health at all ages.
Where can we get it?
We don’t sell it (or anything else), but for your convenience, here’s an example product on Amazon.
Enjoy!
Share This Post
Related Posts
-
Glycemic Index vs Glycemic Load vs Insulin Index
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How To Actually Use Those Indices
Carbohydrates are essential for our life, and/but often bring about our early demise. It would be a very conveniently simple world if it were simply a matter of “enjoy in moderation”, but the truth is, it’s not that simple.
To take an extreme example, for the sake of clearest illustration: The person who eats an 80% whole fruit diet (and makes up the necessary protein and fats etc in the other 20%) will probably be healthier than the person who eats a “standard American diet”, despite not practising moderation in their fruit-eating activities. The “standard American diet” has many faults, and one of those faults is how it promotes sporadic insulin spikes leading to metabolic disease.
If your breakfast is a glass of orange juice, this is a supremely “moderate” consumption, but an insulin spike is an insulin spike.
Quick sidenote: if you’re wondering why eating immoderate amounts of fruit is unlikely to cause such spikes, but a single glass of orange juice is, check out:
Which Sugars Are Healthier, And Which Are Just The Same?
Glycemic Index
The first tool in our toolbox here is glycemic index, or GI.
GI measures how much a carb-containing food raises blood glucose levels, also called blood sugar levels, but it’s just glucose that’s actually measured, bearing in mind that more complex carbs will generally get broken down to glucose.
Pure glucose has a GI of 100, and other foods are ranked from 0 to 100 based on how they compare.
Sometimes, what we do to foods changes its GI.
- Some is because it changed form, like the above example of whole fruit (low GI) vs fruit juice (high GI).
- Some is because of more “industrial” refinement processes, such as whole grain wheat (medium GI) vs white flour and white flour products (high GI)
- Some is because of other changes, like starches that were allowed to cool before being reheated (or eaten cold).
Broadly speaking, a daily average GI of 45 is considered great.
But that’s not the whole story…
Glycemic Load
Glycemic Load, or GL, takes the GI and says “ok, but how much of it was there?”, because this is often relevant information.
Refined sugar may have a high GI, but half a teaspoon of sugar in your coffee isn’t going to move your blood sugar levels as much as a glass of Coke, say—the latter simply has more sugar in, and just the same zero fiber.
GL is calculated by (grams of carbs / 100) x GI, by the way.
But it still misses some important things, so now let’s look at…
Insulin Index
Insulin Index, which does not get an abbreviation (probably because of the potentially confusing appearance of “II”), measures the rise in insulin levels, regardless of glucose levels.
This is important, because a lot of insulin response is independent of blood glucose:
- Some is because of other sugars, some some is in response to fats, and yes, even proteins.
- Some is a function of metabolic base rate.
- Some is a stress response.
- Some remains a mystery!
Another reason it’s important is that insulin drives weight gain and metabolic disorders far more than glucose.
Note: the indices of foods are calculated based on average non-diabetic response. If for example you have Type 1 Diabetes, then when you take a certain food, your rise in insulin is going to be whatever insulin you then take, because your body’s insulin response is disrupted by being too busy fighting a civil war in your pancreas.
If your diabetes is type 2, or you are prediabetic, then a lot of different things could happen depending on the stage and state of your diabetes, but the insulin index is still a very good thing to be aware of, because you want to resensitize your body to insulin, which means (barring any urgent actions for immediate management of hyper- or hypoglycemia, obviously) you want to eat foods with a low insulin index where possible.
Great! What foods have a low insulin index?
Many factors affect insulin index, but to speak in general terms:
- Whole plant foods are usually top-tier options
- Lean and/or white meats generally have lower insulin index than red and/or fatty ones
- Unprocessed is generally lower than processed
- The more solid a food is, generally the lower its insulin index compared to a less solid version of the same food (e.g. baked potatoes vs mashed potatoes; cheese vs milk, etc)
But do remember the non-food factors too! This means where possible:
- reducing/managing stress
- getting frequent exercise
- getting good sleep
- practising intermittent fasting
See for example (we promise you it’s relevant):
Fix Chronic Fatigue & Regain Your Energy, By Science
…as are (especially recommendable!) the two links we drop at the bottom of that page; do check them out if you can
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Stretching & Mobility – by James Atkinson
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
“I will stretch for just 10 minutes per day”, we think, and do our best. Then there are a plethora of videos saying “Stretching mistakes that you are making!” and it turns out we haven’t been doing them in a way that actually helps.
This book fixes that. Unlike some books of the genre, it’s not full of jargon and you won’t need an anatomy and physiology degree to understand it. It is, however, dense in terms of the information it gives—it’s not padded out at all; it contains a lot of value.
The stretches are all well-explained and well-illustrated; the cover art will give you an idea of the anatomical illustration style contained with in.
Atkinson also gives workout plans, so that we know we’re not over- or under-training or trying to do too much or missing important things out.
Bottom line: if you’re looking to start a New Year routine to develop better suppleness, this book is a great primer for that.
Click here to check out Stretching and Mobility, and improve yours!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
28-Day FAST Start Day-by-Day – by Gin Stephens
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We have previously reviewed Gin Stephens’ other book, “Fast. Feast. Repeat.”, so what’s so special about this one that it deserves reviewing too?
This one is all about troubleshooting the pitfalls that many people find when taking up intermittent fasting.
To be clear: the goal here is not a “28 days and yay you did it, put that behind you now”, but rather “28 days and you are now intermittently fasting easily each day and can keep it up without difficulty”. As for the difficulties that may arise early in the 28 days…
Not just issues of willpower, but also the accidental breaks. For example, some artificial sweeteners, while zero-calorie, trigger an insulin response, which breaks the fast on the metabolic level (avoiding that is the whole point of IF). Lots of little tips like that peppered through the book help the reader to stop accidentally self-sabotaging their progress.
The author does talk about psychological issues too, and also how it will feel different at first while the liver is adapting, than later when it has already depleted its glycogen reserves and the body must burn body fat instead. Information like that makes it easier to understand that some initial problems (hunger, getting “hangry”, feeling twitchy, or feeling light-headed) will last only a few weeks and then disappear.
So, understanding things like that makes a big difference too.
The style of the book is simple and clear pop-science, with lots of charts and bullet points and callout-boxes and the like; it makes for very easy reading, and very quick learning of all the salient points, of which there are many.
Bottom line: if you’ve tried intermittent fasting but struggled to make it stick, this book can help you get to where you want to be.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: