Can We Side-Step Age-Related Alienation?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When The World Moves Without Us…
We’ve written before about how reduced social engagement can strike people of all ages, and what can be done about it:
How To Beat Loneliness & Isolation
…but today we’re going to talk more about a specific aspect of it, namely, the alienation that can come with old age—and other life transitions too, but getting older is something that (unless accident or incident befall us first) all of us will definitely do.
What’s the difference?
Loneliness is a status, alienation is more of a process. It can be the alienation in the sense of an implicit “you don’t belong here” message from the world that’s geared around the average person and thus alienates those who are not that (a lack of accessibility to people with disabilities can be an important and very active example of this), and it can also be an alienation from what we’ve previously considered our “niche” in the world—the loss of purpose many people feel upon retirement fits this bill. It can even be a more generalized alienation from our younger selves; it’s easy to have a self-image that doesn’t match one’s current reality, for instance.
Read more: Estranged by Time: Alienation in the Aging Process
So, how to “un-alienate”?
To “un-alienate”, that is to say, to integrate/reintegrate, can be hard. Some things may even be outright impossible, but most will not be!
Consider how, for example, former athletes become coaches—or for that matter, how former party-goers might become party-hosts (even if the kind of “party” might change with time, give or take the pace at which we like to live our lives).
What’s important is that we take what matters the most to us, and examine how we can realistically still engage with that thing.
This is different from trying to hold on grimly to something that’s no longer our speed.
Letting go of the only thing we’ve known will always be scary; sometimes it’s for the best, and sometimes what we really need is just more of a pivot, like the examples above. The crux lies in knowing which:
- Is our relationship with the thing (whatever it may be) still working for us, or is it just bringing strife now?
- If it’s not working for us, is it because of a specific aspect that could be side-stepped while keeping the rest?
- If we’re going to drop that thing entirely (or be dropped by it, which, while cruel, also happens in life), then where are we going to land?
This latter is one where foresight is a gift, because if we bury our heads in the sand we’re going to land wherever we’re dropped, whereas if we acknowledge the process, we can make a strategic move and land on our feet.
Here’s a good pop-science article about this—it’s aimed at people around retirement age, but honestly the advice is relevant for people of all ages, and facing all manner of life transitions, e.g. career transitions (of which retirement is of course the career transition to end all career transitions), relationship transitions (including B/B/B/B: births, betrothals/break-ups, and bereavements) health transitions (usually: life-changing illnesses and/or disabilities—which again, happens to most of us if something doesn’t get us first), etc. So with all that in mind, this becomes more of a “how to reassess your life at those times when it needs reassessing”:
How to Reassess Your Life in Retirement
But that doesn’t mean that letting go is always necessary
Sometimes, the opposite! Sometimes, the age-old advice to “lean in” really is all the situation calls for, which means:
- Be ready to say “yes” to things, and if nobody’s asking, be ready to “hey, do you wanna…?” and take a “build it and they will come” approach. This includes with people of different ages, too! Intergenerational friendships can be very rewarding for all concerned, if done right. Communities that span age-ranges can be great for this—they might be about special interests (this writer has friends ranging through four generations from playing chess, for instance), they could be religious communities if we be religious, LGBT groups if that fits for us, even mutual support groups such as for specific disabilities or chronic illness if we have such—notice how the very things that might isolate us can also bring us together!
- Be open-minded to new experiences; it’s easy to get stuck in a rut of “I’ve never done that” and mistake that self-assessment for an uncritical assumption of “I’m not the kind of person who does that”. Sometimes, you really won’t be! But at least think about it and entertain the possibility, before dismissing it out of hand. And, here’s a life tip: it can be really good to (within the realms of safety, and one’s personal moral principles, of course) take an approach of “try anything once”. Even if we’re almost certain we won’t like it, and even if we then turn out to indeed not like it, it can be a refreshing experience—and now we can say “Yep, tried that, not doing that again” from a position of informed knowledge. That’s the only way we get to look back on a richly lived life of broad experiences, after all, and it is never too late for such.
- Be comfortable prioritizing quality over quantity. This goes for friends, it goes for activities, it goes for experiences. The topic of “what’s the best number of friends to have?” has been a matter of discussion since at least ancient Greek times (Plato and Aristotle examined this extensively), but whatever number we might arrive at, it’s clear that quality is the critical factor, and quantity after that is just a matter of optimizing.
In short: make sure you’re investing—in your relationships, in your areas of interest, in your community (whatever that may mean for you personally), and most of all, and never forget this: in yourself.
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Calm For Surgery – by Dr Chris Bonney
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
As a general rule of thumb, nobody likes having surgery. We may like the results of the surgery, we may like having the surgery done and behind us, but surgery itself is not most people’s idea of fun, and honestly, the recovery period afterwards can be a pain in every sense of the word.
Dr. Chris Bonney, an anesthesiologist, gives us the industry-secrets low-down, and is the voice of experience when it comes to the things to know about and/or prepare in advance—the little things that make a world of difference to your in-hospital experience and afterwards.
Think of it like “frequent flyer traveller tips” but for surgeries, whereupon knowing a given tip can mean the difference between deeply traumatic suffering and merely not being at your usual best. We think that’s worth it.
Share This Post
-
Stop Sabotaging Your Weight Loss – by Jennifer Powter, MSc
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is not a dieting book, and it’s not a motivational pep talk.
The book starts with the assumption that you do want to lose weight (it also assumes you’re a woman, and probably over 40… that’s just the book’s target market, but the same advice is good even if that’s not you), and that you’ve probably been trying, on and off, for a while. Her position is simple:
❝I don’t believe that you have a weight loss problem. I believe that you have a self-sabotage problem❞
As to how this sabotage may be occurring, Powter talks about fears that may be holding you back, including but not limited to:
- Fear of failure
- Fear of the unknown
- Fear of loss
- Fear of embarrassment
- Fear of your weight not being the reason your life sucks
Far from putting the reader down, though, Powter approaches everything with compassion. To this end, her prescription starts with encouraging self-love. Not when you’re down to a certain size, not when you’re conforming perfectly to a certain diet, but now. You don’t have to be perfect to be worthy of love.
On the topic of perfection: a recurring theme in the book is the danger of perfectionism. In her view, perfectionism is nothing more nor less than the most justifiable way to hold yourself back in life.
Lastly, she covers mental reframes, with useful questions to ask oneself on a daily basis, to ensure progressing step by step into your best life.
In short: if you’d like to lose weight and have been trying for a while, maybe on and off, this book could get you out of that cycle and into a much better state of being.
Get your copy of “Stop Sabotaging Your Weight Loss” from Amazon today!
Share This Post
-
Professional-Style Dental Cleaning At Home?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
You know the scene: your dentist is rummaging around inside your mouth with an implement that looks like a medieval torture device; you wince at a sudden sharp pain, only to be told “if you flossed, you wouldn’t be bleeding now”.
For most of us, going to the dentist isn’t near the top of our “favorite things to do” list, but it is of course a necessity of (healthy) life.
So, what can we do to minimize suffering in the dentist’s chair?
First, the basics
Of course, good oral hygiene is the absolute baseline, but with so many choices out there, which is best? We examined an array of options in this three-part series:
- Toothpastes & Mouthwashes: Which Help And Which Harm?
- Flossing Without Flossing?
- Less Common Oral Hygiene Options ← we recommend the miswak! Not only does it clean the teeth as well as or better than traditional brushing, but also it changes the composition of saliva to improve the oral microbiome, effectively turning your saliva into a biological mouthwash that kills unwanted microbes and is comfortable for the ones that should be there.
In fact, caring for the composition of one’s saliva, and thus one’s oral microbiome, is so important that we did a main feature on that, a little later:
Make Your Saliva Better For Your Teeth ← this is especially important if you take any meds that affect the composition of your saliva (scroll down to the table of meds). Your medications’ leaflets won’t tell you that it does that directly, but they will list “dry mouth” as one of the potential side effects (and you’ll probably know if you have a medication that gives you a dry mouth).
Next, level up
For this one, we’ll drop some links to some videos we’ve featured (for those who prefer text, worry not, your faithful writer has added text-based overviews):
- How To Regrow Receding Gums
- Tooth Remineralization: How To Heal Your Teeth Naturally
- Tartar Removal At Home & How To Prevent Tartar
Now, that last one sounds slightly more exciting than it is—it is about using chemical processes to gradually lessen the tartar over time, with a six-month timeframe.
So, what if you want to do one better than that?
Finally… Buckle up, this one’s fun
Ok, so “fun” and “dental care” don’t usually go hand-in-hand, and maybe your sense of fun differs from this writer’s, but hey. The thing is, we’re going to get hands-on with dental tools.
Specifically, these dental tools:
👆 these are literally the tools this writer has; if you look in the specula (the round mirror bits), you can see the reflection of the fluffy gray bathrobe I was wearing when I took the picture!
You can get tools like these easily online; here’s an example product on Amazon; do also shop around of course, and we recommend checking the reviews to ensure good quality.
Writer’s story on why I have these: once upon a time, a wisdom tooth came through at 45°, ploughing through the molar next to it, which then needed removing.
However, my teeth have the interesting anatomical quirk that I have hooked/barbed roots, which does not make tooth extraction easy; it had to come out sidewise, and the process was somewhat bungled by an inexperienced dental surgeon.
When the anesthetic wore off, it was the most pain I’ve ever been in in my life.
After that, I wasn’t a very regular returner to the dentist, and in 2013, I fell into a very deep depression for unrelated reasons, and during that period, I got some plaque/tartar buildup on some of my teeth due to lack of care, that then just stayed until I decided to take care of it more recently, which I am happy to say, I’ve now done (my teeth are the happiest and healthiest they’ve ever been), and I’m going to share how, with you.
So, here’s how to do it… First, you’ll need those tools, of course.
You will also want a good quality backlit magnifying mirror. Again, here’s an example product on Amazon ← this is the exact kind this writer has, and it’s very good.
You may be thinking: “wait a minute, this is scary, those are dangerous and I’m not a dentist!”
If so, then a few quick things to bear in mind:
- If you’re not comfortable doing it, don’t do it. As ever, our medical/legal disclaimer applies, and we share information for your interest only, and not as an exhortation to take any particular action. By all means confer with your dentist, too, and see whether they support the idea.
- These things do look scarier than they are once you get used to them. Do you use metal silverware when eating? Technically you could stab yourself with a fork any time, or damage your teeth with it, but when was the last time you did that?
- With regard to manual dexterity, if you have the manual dexterity required to paint your nails, floss your teeth, sew by hand, or write with a pen, then you have the manual dexterity to do this, too.
Now, about the tools:
- Speculum / magnifying speculum: the one with the mirror. This is useful for looking at the backs of teeth.
- Tweezers: the one with the gold grip in the photo above. You probably won’t need to use these, but we’re sure you know how to use tweezers in general.
- Dental explorer: the one with the big wicked-looking hook on one end, and a tiny (almost invisible in the photo) hook on the other end. This is for examining cavities, not for manipulating things. Best leave that to your dentist if you have cavities.
- Dental pick: this is the one to the right of the dental explorer, and it is for cleaning in the crevices between teeth. One end is quite blunt; the other is pointier, and you can choose which end to use depending on what fits into the shape of the crevice between your teeth.
- Dental scraper: this is the one with chisel ends. One end curves very slightly to the left, the other, very slightly to the right. This is for ergonomics depending on which hand you’re using, and which side you’re scraping (you’ll become very aware that your teeth, even if they look straight, curve very slightly at the edges.
You’ll be using these last two for the actual tartar removal, selecting the tool appropriate to cleaning the flat surface of a tooth, or the crevice where the teeth meet (not like flossing! That part, yes, but under no circumstances is this thing going all the way through to the other side, it’s just for getting into to nook that the scraper can’t so easily clean, that’s all).
A word on using metal against your teeth: a scary prospect, initially! However…
While steel is indeed harder than the enamel of your teeth, the enamel of your teeth is much harder than the plaque/tartar/calculus that you will be removing. Therefore, the technique to use is very gently scrape, starting as gently as humanly possible until you get a feel for it.
Unlike the dentist, you will have an advantage here in that you have biofeedback, and bone conduction of the sounds in your mouth, so you can exercise much more restraint than your dentist can. With the correct minimum of pressure, the tool should glide smoothly down enamel, but when it’s scraping tartar, it should make a very fine sandpapery noise.
This is why “or write with a pen” was one of the skills we mentioned earlier; it’s the same thing; you don’t press with a pen so hard that it goes through the paper, so don’t press so hard with the tool that it damages your enamel, that’s all.
Because of the differential in hardness between the tartar and the enamel, it’s really very easy to remove the tartar without harming the enamel, provided one is gentle.
Final word of warning; we’ll repeat: If you’re not comfortable doing it, don’t do it. As ever, our medical/legal disclaimer applies, and we share information for your interest only, and not as an exhortation to take any particular action. By all means confer with your dentist, too, and see whether they support the idea.
Also, while this kind of cleaning can be done safely at home, we recommend against doing anything more complicated than that.
See for example: Can You Repair Your Own Teeth At Home? ← the short answer is “no”, or not beyond tooth remineralization, anyway, and kits that say otherwise are potentially misleading, or stop-gap solutions at best.
One last time: always consult with a professional and get their advice (ours is not advice; it’s just information).
Take care!
Share This Post
Related Posts
-
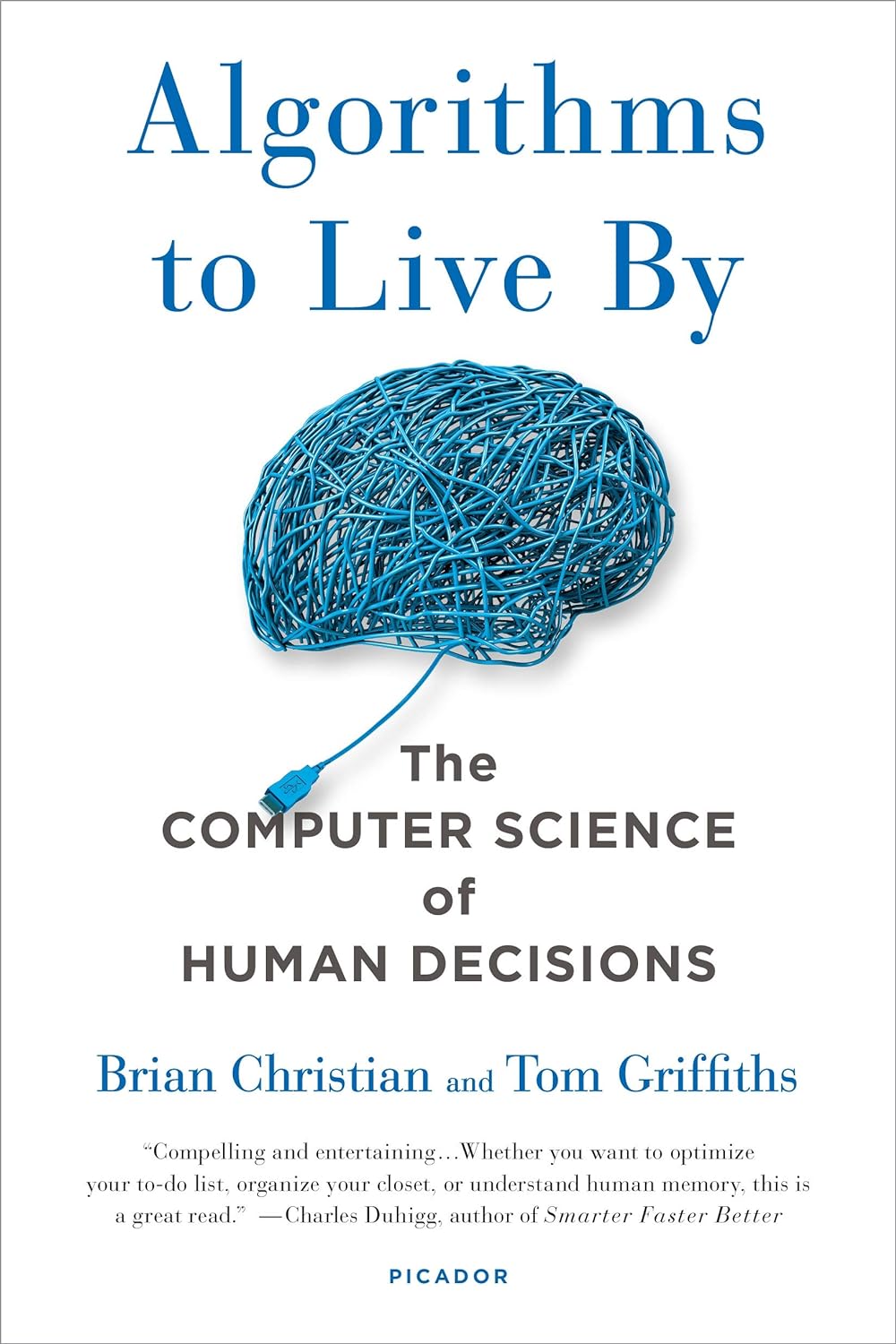
Algorithms to Live By – by Brian Christian and Tom Griffiths
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
As humans, we subconsciously use heuristics a lot to make many complex decisions based on “fuzzy logic”. For example:
Do we buy the cheap shoes that may last us a season, or the much more expensive ones that will last us for years? We’ll—without necessarily giving it much conscious thought—quickly weigh up:
- How much do we like each prospective pair of shoes?
- What else might we need to spend money on now/soon?
- How much money do we have right now?
- How much money do we expect to have in the future?
- Considering our lifestyle, how important is it to have good quality shoes?
How well we perform this rapid calculation may vary wildly, depending on many factors ranging from the quality of the advertising to how long ago we last ate.
And if we make the wrong decision, later we may have buyer’s (or non-buyer’s!) remorse. So, how can we do better?
Authors Brain Christian and Tom Griffiths have a manual for us!
This book covers many “kinds” of decision we often have to make in life, and how to optimize those decisions with the power of mathematics and computer science.
The problems (and solutions) run the gamut of…
- Optimal stopping (when to say “alright, that’s good enough”)
- Overcoming cognitive biases
- Scheduling quandaries
- Bayes’ Theorem
- Game Theory
- And when it’s more efficient to just leave things to chance!
…and many more (12 main areas of decision-making are covered).
For all it draws heavily from mathematics and computer science, the writing style is very easy-reading. It’s a “curl up in the armchair and read for pleasure” book, no matter how weighty and practical its content.
Bottom line: if you improve your ability to make the right decisions even marginally, this book will have been worth your while in the long run!
Order your copy of “Algorithms To Live By” from Amazon today!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
What are the most common symptoms of menopause? And which can hormone therapy treat?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Despite decades of research, navigating menopause seems to have become harder – with conflicting information on the internet, in the media, and from health care providers and researchers.
Adding to the uncertainty, a recent series in the Lancet medical journal challenged some beliefs about the symptoms of menopause and which ones menopausal hormone therapy (also known as hormone replacement therapy) can realistically alleviate.
So what symptoms reliably indicate the start of perimenopause or menopause? And which symptoms can menopause hormone therapy help with? Here’s what the evidence says.
Remind me, what exactly is menopause?
Menopause, simply put, is complete loss of female fertility.
Menopause is traditionally defined as the final menstrual period of a woman (or person female at birth) who previously menstruated. Menopause is diagnosed after 12 months of no further bleeding (unless you’ve had your ovaries removed, which is surgically induced menopause).
Perimenopause starts when menstrual cycles first vary in length by seven or more days, and ends when there has been no bleeding for 12 months.
Both perimenopause and menopause are hard to identify if a person has had a hysterectomy but their ovaries remain, or if natural menstruation is suppressed by a treatment (such as hormonal contraception) or a health condition (such as an eating disorder).
What are the most common symptoms of menopause?
Our study of the highest quality menopause-care guidelines found the internationally recognised symptoms of the perimenopause and menopause are:
- hot flushes and night sweats (known as vasomotor symptoms)
- disturbed sleep
- musculoskeletal pain
- decreased sexual function or desire
- vaginal dryness and irritation
- mood disturbance (low mood, mood changes or depressive symptoms) but not clinical depression.
However, none of these symptoms are menopause-specific, meaning they could have other causes.
In our study of Australian women, 38% of pre-menopausal women, 67% of perimenopausal women and 74% of post-menopausal women aged under 55 experienced hot flushes and/or night sweats.
But the severity of these symptoms varies greatly. Only 2.8% of pre-menopausal women reported moderate to severely bothersome hot flushes and night sweats symptoms, compared with 17.1% of perimenopausal women and 28.5% of post-menopausal women aged under 55.
So bothersome hot flushes and night sweats appear a reliable indicator of perimenopause and menopause – but they’re not the only symptoms. Nor are hot flushes and night sweats a western society phenomenon, as has been suggested. Women in Asian countries are similarly affected.
You don’t need to have night sweats or hot flushes to be menopausal.
Maridav/ShutterstockDepressive symptoms and anxiety are also often linked to menopause but they’re less menopause-specific than hot flushes and night sweats, as they’re common across the entire adult life span.
The most robust guidelines do not stipulate women must have hot flushes or night sweats to be considered as having perimenopausal or post-menopausal symptoms. They acknowledge that new mood disturbances may be a primary manifestation of menopausal hormonal changes.
The extent to which menopausal hormone changes impact memory, concentration and problem solving (frequently talked about as “brain fog”) is uncertain. Some studies suggest perimenopause may impair verbal memory and resolve as women transition through menopause. But strategic thinking and planning (executive brain function) have not been shown to change.
Who might benefit from hormone therapy?
The Lancet papers suggest menopause hormone therapy alleviates hot flushes and night sweats, but the likelihood of it improving sleep, mood or “brain fog” is limited to those bothered by vasomotor symptoms (hot flushes and night sweats).
In contrast, the highest quality clinical guidelines consistently identify both vasomotor symptoms and mood disturbances associated with menopause as reasons for menopause hormone therapy. In other words, you don’t need to have hot flushes or night sweats to be prescribed menopause hormone therapy.
Often, menopause hormone therapy is prescribed alongside a topical vaginal oestrogen to treat vaginal symptoms (dryness, irritation or urinary frequency).
You don’t need to experience hot flushes and night sweats to take hormone therapy.
Monkey Business Images/ShutterstockHowever, none of these guidelines recommend menopause hormone therapy for cognitive symptoms often talked about as “brain fog”.
Despite musculoskeletal pain being the most common menopausal symptom in some populations, the effectiveness of menopause hormone therapy for this specific symptoms still needs to be studied.
Some guidelines, such as an Australian endorsed guideline, support menopause hormone therapy for the prevention of osteoporosis and fracture, but not for the prevention of any other disease.
What are the risks?
The greatest concerns about menopause hormone therapy have been about breast cancer and an increased risk of a deep vein clot which might cause a lung clot.
Oestrogen-only menopause hormone therapy is consistently considered to cause little or no change in breast cancer risk.
Oestrogen taken with a progestogen, which is required for women who have not had a hysterectomy, has been associated with a small increase in the risk of breast cancer, although any risk appears to vary according to the type of therapy used, the dose and duration of use.
Oestrogen taken orally has also been associated with an increased risk of a deep vein clot, although the risk varies according to the formulation used. This risk is avoided by using estrogen patches or gels prescribed at standard doses
What if I don’t want hormone therapy?
If you can’t or don’t want to take menopause hormone therapy, there are also effective non-hormonal prescription therapies available for troublesome hot flushes and night sweats.
In Australia, most of these options are “off-label”, although the new medication fezolinetant has just been approved in Australia for postmenopausal hot flushes and night sweats, and is expected to be available by mid-year. Fezolinetant, taken as a tablet, acts in the brain to stop the chemical neurokinin 3 triggering an inappropriate body heat response (flush and/or sweat).
Unfortunately, most over-the-counter treatments promoted for menopause are either ineffective or unproven. However, cognitive behaviour therapy and hypnosis may provide symptom relief.
The Australasian Menopause Society has useful menopause fact sheets and a find-a-doctor page. The Practitioner Toolkit for Managing Menopause is also freely available.
Susan Davis, Chair of Women’s Health, Monash University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Imposter Syndrome (and why almost everyone has it)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Imposter Syndrome (and why almost everyone has it)
Imposter syndrome is the pervasive idea that we’re not actually good enough, people think we are better than we are, and at any moment we’re going to get found out and disappoint everyone.
Beyond the workplace
Imposter syndrome is most associated with professionals. It can range from a medical professional who feels like they’ve been projecting an image of confidence too much, to a writer or musician who is sure that their next piece will never live up to the acclaim of previous pieces and everyone will suddenly realize they don’t know what they’re doing, to a middle-manager who feels like nobody above or below them realizes how little they know how to do.
But! Less talked-about (but no less prevalent) is imposter syndrome in other areas of life. New parents tend to feel this strongly, as can the “elders” of a family that everyone looks to for advice and strength and support. Perhaps worst is when the person most responsible for the finances of a household feels like everyone just trusts them to keep everything running smoothly, and maybe they shouldn’t because it could all come crashing down at any moment and everyone will see them for the hopeless shambles of a human being that they really are.
Feelings are not facts
And yet (while everyone makes mistakes sometimes) the reality is that we’re all doing our best. Given that imposter syndrome affects up to 82% of people, let’s remember to have some perspective. Everyone feels like they’re winging it sometimes. Everyone feels the pressure.
Well, perhaps not everyone. There’s that other 18%. Some people are sure they’re the best thing ever. Then again, there’s probably some in that 18% that actually feel worse than the 82%—they just couldn’t admit it, even in an anonymized study.
But one thing’s for sure: it’s very, very common. Especially in high-performing women, by the way, and people of color. In other words, people who typically “have to do twice as much to get recognized as half as good”.
That said, the flipside of this is that people who are not in any of those categories may feel “everything is in my favor, so I really have no excuse to not achieve the most”, and can sometimes take very extreme actions to try to avoid perceived failure, and it can be their family that pays the price.
Things to remember
If you find imposter syndrome nagging at you, remember these things:
- There are people far less competent than you, doing the same thing
- Nobody knows how to do everything themselves, especially at first
- If you don’t know how to do something, you can usually find out
- There is always someone to ask for help, or at least advice, or at least support
At the end of the day, we evolved to eat fruit and enjoy the sun. None of us are fully equipped for all the challenges of the modern world, but if we do our reasonable best, and look after each other (and that means that you too, dear reader, deserve looking after as well), we can all do ok.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: