A new government inquiry will examine women’s pain and treatment. How and why is it different?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Victorian government has announced an inquiry into women’s pain. Given women are disproportionately affected by pain, such a thorough investigation is long overdue.
The inquiry, the first of its kind in Australia and the first we’re aware of internationally, is expected to take a year. It aims to improve care and services for Victorian girls and women experiencing pain in the future.
The gender pain gap
Globally, more women report chronic pain than men do. A survey of over 1,750 Victorian women found 40% are living with chronic pain.
Approximately half of chronic pain conditions have a higher prevalence in women compared to men, including low back pain and osteoarthritis. And female-specific pain conditions, such as endometriosis, are much more common than male-specific pain conditions such as chronic prostatitis/chronic pelvic pain syndrome.
These statistics are seen across the lifespan, with higher rates of chronic pain being reported in females as young as two years old. This discrepancy increases with age, with 28% of Australian women aged over 85 experiencing chronic pain compared to 18% of men.
It feels worse
Women also experience pain differently to men. There is some evidence to suggest that when diagnosed with the same condition, women are more likely to report higher pain scores than men.
Similarly, there is some evidence to suggest women are also more likely to report higher pain scores during experimental trials where the same painful pressure stimulus is applied to both women and men.
Pain is also more burdensome for women. Depression is twice as prevalent in women with chronic pain than men with chronic pain. Women are also more likely to report more health care use and be hospitalised due to their pain than men.

Shutterstock
Medical misogyny
Women in pain are viewed and treated differently to men. Women are more likely to be told their pain is psychological and dismissed as not being real or “all in their head”.
Hollywood actor Selma Blair recently shared her experience of having her symptoms repeatedly dismissed by doctors and put down to “menstrual issues”, before being diagnosed with multiple sclerosis in 2018.
It’s an experience familiar to many women in Australia, where medical misogyny still runs deep. Our research has repeatedly shown Australian women with pelvic pain are similarly dismissed, leading to lengthy diagnostic delays and serious impacts on their quality of life.
Misogyny exists in research too
Historically, misogyny has also run deep in medical research, including pain research. Women have been viewed as smaller bodied men with different reproductive functions. As a result, most pre-clinical pain research has used male rodents as the default research subject. Some researchers say the menstrual cycle in female rodents adds additional variability and therefore uncertainty to experiments. And while variability due to the menstrual cycle may be true, it may be no greater than male-specific sources of variability (such as within-cage aggression and dominance) that can also influence research findings.
The exclusion of female subjects in pre-clinical studies has hindered our understanding of sex differences in pain and of response to treatment. Only recently have we begun to understand various genetic, neurochemical, and neuroimmune factors contribute to sex differences in pain prevalence and sensitivity. And sex differences exist in pain processing itself. For instance, in the spinal cord, male and female rodents process potentially painful stimuli through entirely different immune cells.
These differences have relevance for how pain should be treated in women, yet many of the existing pharmacological treatments for pain, including opioids, are largely or solely based upon research completed on male rodents.
When women seek care, their pain is also treated differently. Studies show women receive less pain medication after surgery compared to men. In fact, one study found while men were prescribed opioids after joint surgery, women were more likely to be prescribed antidepressants. In another study, women were more likely to receive sedatives for pain relief following surgery, while men were more likely to receive pain medication.
So, women are disproportionately affected by pain in terms of how common it is and sensitivity, but also in how their pain is viewed, treated, and even researched. Women continue to be excluded, dismissed, and receive sub-optimal care, and the recently announced inquiry aims to improve this.
What will the inquiry involve?
Consumers, health-care professionals and health-care organisations will be invited to share their experiences of treatment services for women’s pain in Victoria as part of the year-long inquiry. These experiences will be used to describe the current service delivery system available to Victorian women with pain, and to plan more appropriate services to be delivered in the future.
Inquiry submissions are now open until March 12 2024. If you are a Victorian woman living with pain, or provide care to Victorian women with pain, we encourage you to submit.
The state has an excellent track record of improving women’s health in many areas, including heart, sexual, and reproductive health, but clearly, we have a way to go with women’s pain. We wait with bated breath to see the results of this much-needed investigation, and encourage other states and territories to take note of the findings.
Jane Chalmers, Senior Lecturer in Pain Sciences, University of South Australia and Amelia Mardon, PhD Candidate, University of South Australia
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Knee Cracking & Popping: Should You Be Worried?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Tom Walters (Doctor of Physical Therapy) explains about what’s going on behind our musical knees, and whether or not this synovial symphony is cause for concern.
When to worry (and when not to)
If the clicking/cracking/popping/etc does not come with pain, then it is probably being caused by the harmless movement of fluid within the joints, in this case specifically the patellofemoral joint, just behind the kneecap.
As Dr. Walters says:
❝It is extremely important that people understand that noises from the knee are usually not associated with pathology and may actually be a sign of a healthy, well-lubricated joint. let’s be careful not to make people feel bad about their knee noise as it can negatively influence how they view their body!❞
On the other hand, there is also such a thing as patellofemoral joint pain syndrome (PFPS), which is very common, and involves pain behind the kneecap, especially upon over-stressing the knee(s).
In such cases, it is good to get that checked out by a doctor/physiotherapist.
Dr. Walters advises us to gradually build up strength, and not try for too much too quickly. He also advises us to take care to strengthen our glutes in particular, so our knees have adequate support. Gentle stretching of the quadriceps and soft tissue mobilization with a foam roller, are also recommended, to reduce tension on the kneecap.
For more on these things and especially about the exercises, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might like to read:
How To Really Take Care Of Your Joints
Take care!
Share This Post
-
From straight to curly, thick to thin: here’s how hormones and chemotherapy can change your hair
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Head hair comes in many colours, shapes and sizes, and hairstyles are often an expression of personal style or cultural identity.
Many different genes determine our hair texture, thickness and colour. But some people’s hair changes around the time of puberty, pregnancy or after chemotherapy.
So, what can cause hair to become curlier, thicker, thinner or grey?
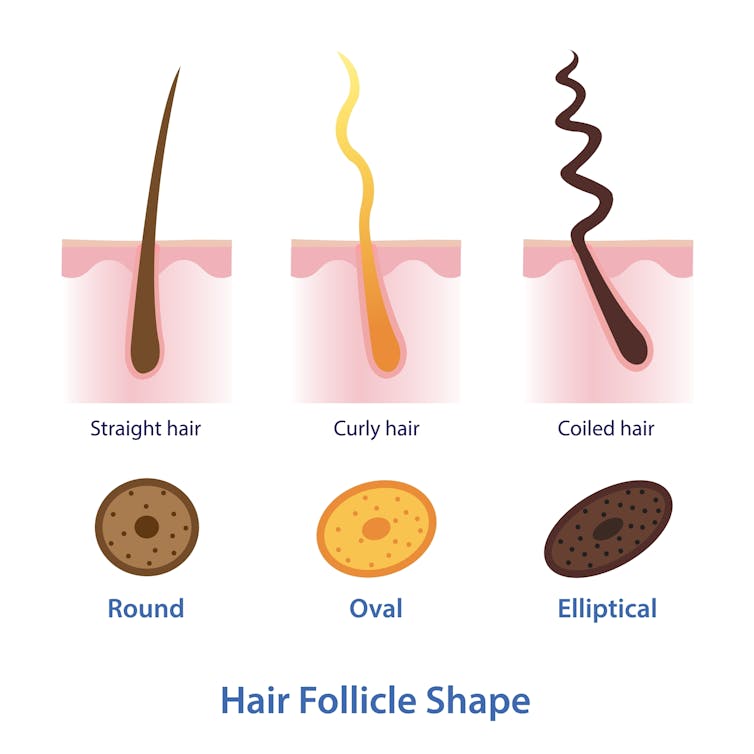
Curly or straight? How hair follicle shape plays a role
Hair is made of keratin, a strong and insoluble protein. Each hair strand grows from its own hair follicle that extends deep into the skin.
Curly hair forms due to asymmetry of both the hair follicle and the keratin in the hair.
Follicles that produce curly hair are asymmetrical and curved and lie at an angle to the surface of the skin. This kinks the hair as it first grows.
The asymmetry of the hair follicle also causes the keratin to bunch up on one side of the hair strand. This pulls parts of the hair strand closer together into a curl, which maintains the curl as the hair continues to grow.
Follicles that are symmetrical, round and perpendicular to the skin surface produce straight hair.
Each hair strand grows from its own hair follicle.
Mosterpiece/ShutterstockLife changes, hair changes
Our hair undergoes repeated cycles throughout life, with different stages of growth and loss.
Each hair follicle contains stem cells, which multiply and grow into a hair strand.
Head hairs spend most of their time in the growth phase, which can last for several years. This is why head hair can grow so long.
Let’s look at the life of a single hair strand. After the growth phase is a transitional phase of about two weeks, where the hair strand stops growing. This is followed by a resting phase where the hair remains in the follicle for a few months before it naturally falls out.
The hair follicle remains in the skin and the stems cells grow a new hair to repeat the cycle.
Each hair on the scalp is replaced every three to five years.
Each hair on the scalp is replaced every three to five years.
Just Life/ShutterstockHormone changes during and after pregnancy alter the usual hair cycle
Many women notice their hair is thicker during pregnancy.
During pregnancy, high levels of oestrogen, progesterone and prolactin prolong the resting phase of the hair cycle. This means the hair stays in the hair follicle for longer, with less hair loss.
A drop in hormones a few months after delivery causes increased hair loss. This is due to all the hairs that remained in the resting phase during pregnancy falling out in a fairly synchronised way.
Hair can change around puberty, pregnancy or after chemotherapy
This is related to the genetics of hair shape, which is an example of incomplete dominance.
Incomplete dominance is when there is a middle version of a trait. For hair, we have curly hair and straight hair genes. But when someone has one curly hair gene and one straight hair gene, they can have wavy hair.
Hormonal changes that occur around puberty and pregnancy can affect the function of genes. This can cause the curly hair gene of someone with wavy hair to become more active. This can change their hair from wavy to curly.
Researchers have identified that activating specific genes can change hair in pigs from straight to curly.
Chemotherapy has very visible effects on hair. Chemotherapy kills rapidly dividing cells, including hair follicles, which causes hair loss. Chemotherapy can also have genetic effects that influence hair follicle shape. This can cause hair to regrow with a different shape for the first few cycles of hair regrowth.
Your hair can change at different stages of your life.
Igor Ivakhno/ShutterstockHormonal changes as we age also affect our hair
Throughout life, thyroid hormones are essential for production of keratin. Low levels of thyroid hormones can cause dry and brittle hair.
Oestrogen and androgens also regulate hair growth and loss, particularly as we age.
Balding in males is due to higher levels of androgens. In particular, high dihydrotestosterone (sometimes shortened to DHT), which is produced in the body from testosterone, has a role in male pattern baldness.
Some women experience female pattern hair loss. This is caused by a combination of genetic factors plus lower levels of oestrogen and higher androgens after menopause. The hair follicles become smaller and smaller until they no longer produce hairs.
Reduced function of the cells that produce melanin (the pigment that gives our hair colour) is what causes greying.
Theresa Larkin, Associate professor of Medical Sciences, University of Wollongong
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Air Purifiers & Sleep
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝I’ve read that air pollution has a negative effect on sleep quality and duration. Since I live next to a busy road, I was wondering whether I should invest in an air purifier. What are 10Almonds’s views?❞
Going straight to the science, there are two questions here:
- Does air pollution negatively affect sleep quality and duration?
- Does the use of an air purify actually improve the air quality in the way(s) necessary to make a difference?
We thought we’d have to tackle these questions separately, but we did find one study that addressed your question directly. It was a small study (n=30 if you believe the abstract; n=29 if you read the paper itself—one person dropped out); the results were modest but clear:
❝The purifier filter was associated with increased total sleep time for an average of 12 min per night, and increased total time in bed for an average of 19 min per night relative to the placebo.
There were several sleep and mood outcomes for which no changes were observed, and time awake after sleep onset was higher for the purifier filter. Air quality was better during the high-efficiency particulate air filter condition.
These findings offer positive indications that environmental interventions that improve air quality can have benefits for sleep outcomes in healthy populations who are not exhibiting clinical sleep disturbances.❞
In the above-linked paper’s introduction, it does establish the deleterious effect of air pollution on a wide variety of health metrics, including sleep, this latter evidenced per Caddick et al. (2018): A review of the environmental parameters necessary for an optimal sleep environment
Now, you may be wondering: is an extra 12 minutes per night worth it?
That’s your choice to make, but we would argue that it is. We can make many choices in our lives that affect our health slightly for the better or the worse. If we make a stack of choices in a particular direction, the effects will also stack, if not outright compound.
So in the case of sleep, it might be (arbitrary numbers for the sake of illustration):
- Get good exercise earlier in the day (+3%)
- Get good food earlier in the day (+2.5%)
- Practice mindfulness/meditation before bed (+2.5%)
- Have a nice dark room (+5%)
- Have fresh bedding (+2.5%)
- Have an air purifier running (+3%)
Now, those numbers are, as we said, arbitrary*, but remember that percentages don’t add up; they compound. So that “+3%” starts being a lot more meaningful than if it were just by itself.
*Confession: the figure of 3% for the air purifier wasn’t entirely arbitrary; it was based on 100(12/405) = 80/27 ≈ 3, wherein the 405 figure was an approximation of the average total time (in minutes) spent sleeping with placebo, based on a peep at their results graph. There are several ways the average could be reasonably calculated, but 6h45 (i.e., 405 minutes) was an approximate average of those reasonable approximate averages.
So, 12 minutes is a 3% improvement on that.
Don’t have an air purifier and want one?
We don’t sell them, but here’s an example on Amazon, for your convenience
Take care!
Share This Post
Related Posts
-
Healing Arthritis – by Dr. Susan Blum
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We previously reviewed another book by this author, her Immune System Recovery Plan, and today it’s more specific: healing arthritis
Of course, not all arthritis is rooted in immune dysfunction, but a) all of it is made worse by immune dysfunction and b) rheumatoid arthritis, which is an autoimmune disease, affects 1% of the population.
This book tackles all kinds of arthritis, by focusing on addressing the underlying causes and treating those, and (whether it was the cause or not) reducing inflammation without medication, because that will always help.
The “3 steps” mentioned in the subtitle are three stages of a plan to improve the gut microbiome in such a way that it not only stops worsening your arthritis, but starts making it better.
The style here is on the hard end of pop-science, so if you want something more conversational/personable, then this won’t be so much for you, but if you just want the information and explanation, then this does it just fine, and it has frequent references to the science to back it up, with a reassuringly extensive bibliography.
Bottom line: if you have arthritis and want a book that will help you to get either symptom-free or as close to that as is possible from your current condition (bearing in mind that arthritis is generally degenerative), then this is a great book for that.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Improve Your Insulin Sensitivity!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve written before about blood sugar management, for example:
10 Ways To Balance Blood Sugars ← this one really is the most solid foundation possible; if you do nothing else, do these 10 things!
And as for why we care:
Good (Or Bad) Health Starts With Your Blood
…because the same things that cause type 2 diabetes, go on to cause many other woes, with particularly strong comorbidities in the case of Alzheimer’s disease and other dementias, as well as heart disease of various kinds, and a long long laundry list of immune dysfunctions / inflammatory disorders in general.
In short, if you can’t keep your blood sugars even, the rest of your health will fall like so many dominoes.
Getting a baseline
Are you counting steps? Counting calories? Monitoring your sleep? Heart rate zones? These all have their merits:
- Steps: One More Resource Against Osteoporosis!
- Calories: Is Cutting Calories The Key To Healthy Long Life?
- Sleep: A Head-To-Head Of Google and Apple’s Top Apps For Getting Your Head Down
- Heart Rate Zones: Heart Rate Zones, Oxalates, & More
But something far fewer people do unless they have diabetes or are very enthusiastic about personal health, is to track blood sugars:
Here’s how: Track Your Blood Sugars For Better Personalized Health
And for understanding some things to watch out for when using a continuous glucose monitor:
Continuous Glucose Monitors Without Diabetes: Pros & Cons
Writer’s anecdote: I decided to give one a try for a few months, and so far it has been informative, albeit unexciting. It seems that with my diet (mostly whole-foods plant based, though I do have a wholegrain wheat product about twice per week (usually: flatbread once, pasta once) which is… Well, we could argue it’s whole-food plant based, but let’s be honest, it’s a little processed), my blood sugars don’t really have spikes at all; the graph looks more like gently rolling low hills (which is good). However! Even so, by experimenting with it, I can see for myself what differences different foods/interventions make to my blood sugars, which is helpful, and it also improves my motivation for intermittent fasting. It also means that if I think “hmm, my energy levels are feeling low; I need a snack” I can touch my phone to my arm and find out if that is really the reason (so far, it hasn’t been). I expect that as I monitor my blood sugars continuously and look at the data frequently, I’ll start to get a much more intuitive feel for my own blood sugars, in much the same way I can generally intuit my hormone levels correctly after years of taking-and-testing.
So much for blood sugars. Now, what about insulin?
Step Zero
If taking care of blood sugars is step one, then taking care of insulin is step zero.
Often’s it’s viewed the other way around: we try to keep our blood sugars balanced, to reduce the need for our bodies to produce so much insulin that it gets worn out. And that’s good and fine, but…
To quote what we wrote when reviewing “Why We Get Sick” last month:
❝Dr. Bikman makes the case that while indeed hyper- or hypoglycemia bring their problems, mostly these are symptoms rather than causes, and the real culprit is insulin resistance, and this is important for two main reasons:
- Insulin resistance occurs well before the other symptoms set in (which means: it is the thing that truly needs to be nipped in the bud; if your fasting blood sugars are rising, then you missed “nipping it in the bud” likely by a decade or more)
- Insulin resistance causes more problems than “mere” hyperglycemia (the most commonly-known result of insulin resistance) does, so again, it really needs to be considered separately from blood sugar management.
This latter, Dr. Bikman goes into in great detail, linking insulin resistance (even if blood sugar levels are normal) to all manner of diseases (hence the title).
You may be wondering: how can blood sugar levels be normal, if we have insulin resistance?
And the answer is that for as long as it is still able, your pancreas will just faithfully crank out more and more insulin to deal with the blood sugar levels that would otherwise be steadily rising. Since people measure blood sugar levels much more regularly than anyone checks for actual insulin levels, this means that one can be insulin resistant for years without knowing it, until finally the pancreas is no longer able to keep up with the demand—then that’s when people finally notice.❞
You can read the full book review here:
Now, testing for insulin is not so quick, easy, or accessible as testing for glucose, but it can be worthwhile to order such a test—because, as discussed, your insulin levels could be high even while your blood sugars are still normal, and it won’t be until the pancreas finally reaches breaking point that your blood sugars show it.
So, knowing your insulin levels can help you intervene before your pancreas reaches that breaking point.
We can’t advise on local services available for ordering blood tests (because they will vary depending on location), but a simple Google search should suffice to show what’s available in your region.
Once you know your insulin levels (or even if you don’t, but simply take the principled position that improving insulin sensitivity will be good regardless), you can set about managing them.
Insulin sensitivity is important, because the better it is (higher insulin sensitivity), the less insulin the pancreas has to make to tidy up the same amount of glucose into places that are good for it to go—which is good. In contrast, the worse it is (higher insulin resistance), the more insulin the pancreas has to make to do the same blood sugar management. Which is bad.
What to do about it
We imagine you will already be eating in a way that is conducive to avoiding or reversing type 2 diabetes, but for anyone who wants a refresher,
See: How To Prevent And Reverse Type 2 Diabetes
…which yes, as well as meaning eating/avoiding certain foods, does recommend intermittent fasting. For anyone who wants a primer on that,
See: Intermittent Fasting: Methods & Benefits
There are also drugs you may want to consider:
Metformin Without Diabetes, For Weight-Loss & More
And “nutraceuticals” that sound like drugs, for example:
Glutathione’s Benefits: The Usual And The Unique ← the good news is, it’s found in several common foods
You may have heard the hype about “nature’s Ozempic”, and berberine isn’t exactly that (works in mostly different ways), but its benefits do include improving insulin sensitivity:
Berberine For Metabolic Health
Lastly, while eating for blood sugar management is all well and good, do be aware that some things affect insulin levels without increased blood sugar levels. So even if you’re using a CGM, you may go blissfully unaware of an insulin spike, because there was no glucose spike on the graph—and in contrast, there could even be a dip in blood sugar levels, if you consumed something that increased insulin levels without providing glucose at the same time, making you think “I should have some carbs”, which visually on the graph would even out your blood sugars, but invisibly, would worsen the already-extant insulin spike.
Read more about this: Strange Things Happening In The Islets Of Langerhans: When Carbs, Proteins, & Fats Switch Metabolic Roles
Now, since you probably can’t test your insulin at a moment’s notice, the way to watch out for this is “hmm, I ate some protein/fats (delete as applicable) without carbs and my blood sugars dipped; I know what’s going on here”.
Want to know more?
We heartily recommend the “Why We Get Sick” book we linked above, as this focuses on insulin resistance/sensitivity itself!
However, a very good general primer on blood sugar management (and thus, by extension, at least moderately good insulin management), is:
Glucose Revolution: The Life-Changing Power of Balancing Your Blood Sugar – by Jessie Inchauspé
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Miss Diagnosis: Anxiety, ADHD, & Women
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝Why is ADHD so often misdiagnosed as anxiety in women?❞
A great question! A short and slightly flippant answer could be “it’s the medical misogyny”:
Women and Minorities Bear the Brunt of Medical Misdiagnosis
…and if you’d like to learn more in-depth about this, we recommend this excellent book:
Unwell Women: Misdiagnosis and Myth in a Man-Made World – by Dr. Elinor Cleghorn ← you can read our review here
However, in this case there is more going on too!
Part of this is because ADHD is, like many psychiatric issues, a collection of symptoms that may or may not all always be present. Since clinical definitions are decided by clinicians, rather than some special natural law of the universe, sometimes this results in “several small conditions in a trenchcoat”, and if one symptom is or isn’t present, it can make things look quite different:
What’s The Difference Between ADD and ADHD?
There are two things at hand here: as in the above example, there’s the presence or absence of hyperactivity, but also, that “attention deficit”?
It’s often not really a deficit of attention, so much as the attention is going somewhere else—an example of naming psychiatric disorders for how they affect other people, rather than the person in question.
Sidenote: personality disorders really get the worst of this!
“You have a deep insecurity about never being good enough, and you constantly mess up in your attempt to overcompensate? You may have Evil Bastard Disorder!”
“You have a crippling fear of abandonment and that you are fundamentally unloveable, so you do all you can to try to keep people close? You must have Manipulative Bitch Disorder!”
etc
See also: Why Everyone You Don’t Like Is A Narcissist
In the case of ADHD and anxiety and women, a lot of this comes down to how the redirection of focus is perceived:
❝For some time, it has been held that women with ADHD are more likely to internalize symptoms and become anxious and depressed and to suffer emotional dysregulation❞
This internalization of symptoms, vs the externalization more generally perceived in boys and men, is more likely to be seen as anxiety.
Double standards also abound for social reasons, e.g:
- He is someone who thinks ten steps ahead and covers all bases
- She is anxious and indecisive and unable to settle on one outcome
Here’s a very good overview of how this double-standard makes its way into diagnostic processes, along with other built-in biases:
Miss. Diagnosis: A Systematic Review of ADHD in Adult Women
Want to learn more?
We’ve reviewed quite a few books about ADHD, but if we had to pick one to spotlight, we’d recommend this one:
The Silent Struggle: Taking Charge of ADHD in Adults – by L. William Ross-Child, MLC
Enjoy! And while we have your attention… Would you like this section to be bigger? If so, send us more questions!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: