A new emergency procedure for cardiac arrests aims to save more lives – here’s how it works
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
As of January this year, Aotearoa New Zealand became just the second country (after Canada) to adopt a groundbreaking new procedure for patients experiencing cardiac arrest.
Known as “double sequential external defibrillation” (DSED), it will change initial emergency response strategies and potentially improve survival rates for some patients.
Surviving cardiac arrest hinges crucially on effective resuscitation. When the heart is working normally, electrical pulses travel through its muscular walls creating regular, co-ordinated contractions.
But if normal electrical rhythms are disrupted, heartbeats can become unco-ordinated and ineffective, or cease entirely, leading to cardiac arrest.
Defibrillation is a cornerstone resuscitation method. It gives the heart a powerful electric shock to terminate the abnormal electrical activity. This allows the heart to re-establish its regular rhythm.
Its success hinges on the underlying dysfunctional heart rhythm and the proper positioning of the defibrillation pads that deliver the shock. The new procedure will provide a second option when standard positioning is not effective.
Using two defibrillators
During standard defibrillation, one pad is placed on the right side of the chest just below the collarbone. A second pad is placed below the left armpit. Shocks are given every two minutes.
Early defibrillation can dramatically improve the likelihood of surviving a cardiac arrest. However, around 20% of patients whose cardiac arrest is caused by “ventricular fibrillation” or “pulseless ventricular tachycardia” do not respond to the standard defibrillation approach. Both conditions are characterised by abnormal activity in the heart ventricles.
DSED is a novel method that provides rapid sequential shocks to the heart using two defibrillators. The pads are attached in two different locations: one on the front and side of the chest, the other on the front and back.
A single operator activates the defibrillators in sequence, with one hand moving from the first to the second. According to a recent randomised trial in Canada, this approach could more than double the chances of survival for patients with ventricular fibrillation or pulseless ventricular tachycardia who are not responding to standard shocks.
The second shock is thought to improve the chances of eliminating persistent abnormal electrical activity. It delivers more total energy to the heart, travelling along a different pathway closer to the heart’s left ventricle.
Evidence of success
New Zealand ambulance data from 2020 to 2023 identified about 1,390 people who could potentially benefit from novel defibrillation methods. This group has a current survival rate of only 14%.
Recognising the potential for DSED to dramatically improve survival for these patients, the National Ambulance Sector Clinical Working Group updated the clinical procedures and guidelines for emergency medical services personnel.
The guidelines now specify that if ventricular fibrillation or pulseless ventricular tachycardia persist after two shocks with standard defibrillation, the DSED method should be administered. Two defibrillators need to be available, and staff must be trained in the new approach.
Though the existing evidence for DSED is compelling, until recently it was based on theory and a small number of potentially biased observational studies. The Canadian trial was the first to directly compare DSED to standard treatment.
From a total of 261 patients, 30.4% treated with this strategy survived, compared to 13.3% when standard resuscitation protocols were followed.
The design of the trial minimised the risk of other factors confounding results. It provides confidence that survival improvements were due to the defibrillation approach and not regional differences in resources and training.
The study also corroborates and builds on existing theoretical and clinical scientific evidence. As the trial was stopped early due to the COVID-19 pandemic, however, the researchers could recruit fewer than half of the numbers planned for the study.
Despite these and other limitations, the international group of experts that advises on best practice for resuscitation updated its recommendations in 2023 in response to the trial results. It suggested (with caution) that emergency medical services consider DSED for patients with ventricular fibrillation or pulseless ventricular tachycardia who are not responding to standard treatment.
Training and implementation
Although the evidence is still emerging, implementation of DSED by emergency services in New Zealand has implications beyond the care of patients nationally. It is also a key step in advancing knowledge about optimal resuscitation strategies globally.
There are always concerns when translating an intervention from a controlled research environment to the relative disorder of the real world. But the balance of evidence was carefully considered before making the decision to change procedures for a group of patients who have a low likelihood of survival with current treatment.
Before using DSED, emergency medical personnel undergo mandatory education, simulation and training. Implementation is closely monitored to determine its impact.
Hospitals and emergency departments have been informed of the protocol changes and been given opportunities to ask questions and give feedback. As part of the implementation, the St John ambulance service will perform case reviews in addition to wider monitoring to ensure patient safety is prioritised.
Ultimately, those involved are optimistic this change to cardiac arrest management in New Zealand will have a positive impact on survival for affected patients.
Vinuli Withanarachchie, PhD candidate, College of Health, Massey University; Bridget Dicker, Associate Professor of Paramedicine, Auckland University of Technology, and Sarah Maessen, Research Associate, Auckland University of Technology
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Rushing Woman’s Syndrome – by Dr. Libby Weaver
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s well-known that very many women suffer from “the triple burden” of professional work, housework, and childcare. And it’s not even necessarily that we resent any of those things or feel like they’re a burden; we (hopefully) love our professions, homes, children. But, here’s the thing: no amount of love will add extra hours to the day!
On the psychological level, a lot is about making more conscious decisions and fewer automatic reactions. For example, everyone wants everything from us right now, if not by yesterday, but when do they need it? And, is it even our responsibility? Not everything is, and many of us take on more than we should in our effort to be “enough”.
On the physical level, she covers hormones, including the menstrual/menopausal and the metabolic, as well as liver health, digestive issues, and sleep.
The style is direct and friendly, making frequent references to science but not getting deep into it.
It’s worth noting that while she acknowledges other demographics exist, she’s writing mainly for an audience of otherwise healthy straight white women with children and at least moderate financial resources, so if you fall outside of those things, there may be things that society will penalize you for and expect more from you in return for less, so that is a limitation of the book.
Bottom line: if the above describes you, you will probably get value out of this book.
Click here to check out Rushing Woman’s Syndrome, and take care of yourself too!
Share This Post
-
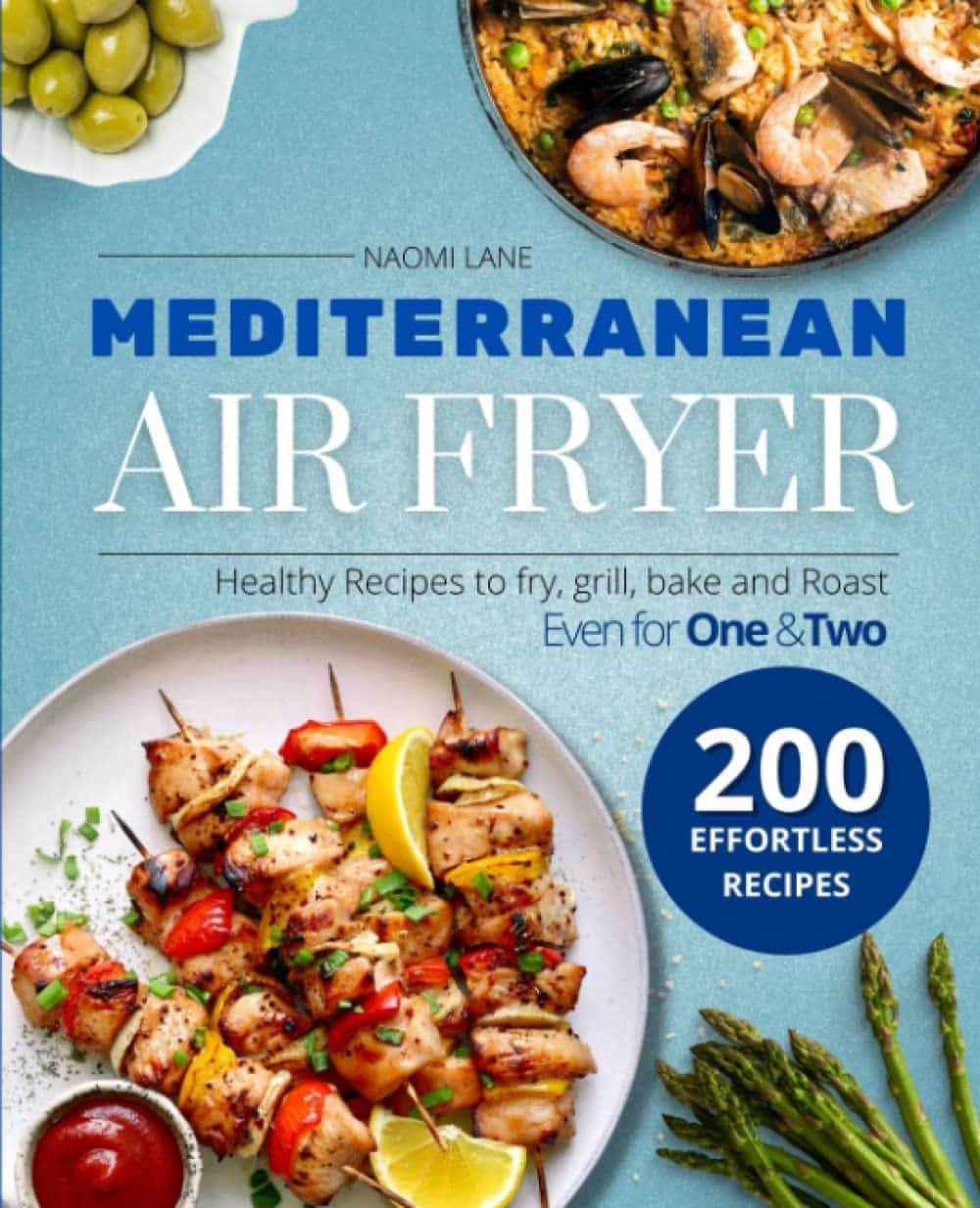
Mediterranean Air Fryer Cookbook – by Naomi Lane
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
There are Mediterranean Diet cookbooks, and there are air fryer cookbooks. And then there are (a surprisingly large intersection of!) Mediterranean Diet air fryer cookbooks. We wanted to feature one of them in today’s newsletter… And as part of the selection process, looked through quite a stack of them, and honestly, were quite disappointed with many. This one, however, was one of the ones that stood out for its quality of both content and clarity, and after a more thorough reading, we now present it to you:
Naomi Lane is a professional dietician, chef, recipe developer, and food writer… And it shows, on all counts.
She covers what the Mediterranean diet is, and she covers far more than this reviewer knew it was even possible to know about the use of an air fryer. That alone would make the book a worthy purchase already.
The bulk of the book is the promised 200 recipes. They cover assorted dietary requirements (gluten-free, dairy-free, etc) while keeping to the Mediterranean Diet.
The recipes are super clear, just what you need to know, no reading through a nostalgic storytime first to find things. Also no pictures, which will be a plus for some readers and a minus for others. The recipes also come complete with nutritional information for each meal (including sodium), so you don’t have to do your own calculations!
Bottom line: this is the Mediterranean Diet air fryer cook book. Get it, thank us later!
Get your copy of “Mediterranean Air Fryer Cookbook” on Amazon today!
Share This Post
-
Undoing The Damage Of Life’s Hard Knocks
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Sometimes, What Doesn’t Kill Us Makes Us Insecure
We’ve written before about Complex PTSD, which is much more common than the more popularly understood kind:
Given that C-PTSD affects so many people (around 1 in 5, but really, do read the article above! It explains it better than we have room to repeat today), it seems like a good idea to share tips for managing it.
(Last time, we took all the space for explaining it, so we just linked to some external resources at the end)
What happened to you?
PTSD has (as a necessity, as part of its diagnostic criteria) a clear event that caused it, which makes the above question easy to answer.
C-PTSD often takes more examination to figure out what tapestry of circumstances (and likely but not necessarily: treatment by other people) caused it.
Often it will feel like “but it can’t be that; that’s not that bad”, or “everyone has things like that” (in which case, you’re probably one of the one in five).
The deeper questions
Start by asking yourself: what are you most afraid of, and why? What are you most ashamed of? What do you fear that other people might say about you?
Often there is a core pattern of insecurity that can be summed up in a simple, harmful, I-message, e.g:
- I am a bad person
- I am unloveable
- I am a fake
- I am easy to hurt
- I cannot keep my loved ones safe
…and so forth.
For a bigger list of common insecurities to see what resonates, check out:
Basic Fears/Insecurities, And Their Corresponding Needs/Desires
Find where they came from
You probably learned bad beliefs, and consequently bad coping strategies, because of bad circumstances, and/or bad advice.
- When a parent exclaimed in anger about how stupid you are
- When a partner exclaimed in frustration that always mess everything up
- When an employer told you you weren’t good enough
…or maybe they told you one thing, and showed you the opposite. Or maybe it was entirely non-verbal circumstances:
- When you gambled on a good idea and lost everything
- When you tried so hard at some important endeavour and failed
- When you thought someone could be trusted, and learned the hard way that you were wrong
These are “life’s difficult bits”, but when we’ve lived through a whole stack of them, it’s less like a single shattering hammer-blow of PTSD, and more like the consistent non-stop tap tap tap that ends up doing just as much damage in the long run.
Resolve them
That may sound a bit like a “and quickly create world peace” level of task, but we have tools:
Ask yourself: what if…
…it had been different? Take some time and indulge in a full-blown fantasy of a life that was better. Explore it. How would those different life lessons, different messages, have impacted who you are, your personality, your behaviour?
This is useful, because the brain is famously bad at telling real memories from false ones. Consciously, you’ll know that one was an exploratory fantasy, but to your brain, it’s still doing the appropriate rewiring. So, little by little, neuroplasticity will do its thing.
Tell yourself a better lie
We borrowed this one from the title of a very good book which we’ve reviewed previously.
This idea is not about self-delusion, but rather that we already express our own experiences as a sort of narrative, and that narrative tends to contain value judgements that are often not useful, e.g. “I am stupid”, “I am useless”, and all the other insecurities we mentioned earlier. Some simple examples might be:
- “I had a terrible childhood” → “I have come so far”
- “I should have known better” → “I am wiser now”
- “I have lost so much” → “I have experienced so much”
So, replacing that self-talk can go a long way to re-writing how secure we feel, and therefore how much trauma-response (ideally: none!) we have to stimuli that are not really as threatening as we sometimes feel they are (a hallmark of PTSD in general).
Here’s a guide to more ways:
How To Get Your Brain On A More Positive Track (Without Toxic Positivity)
Take care!
Share This Post
Related Posts
-
Why a common asthma drug will now carry extra safety warnings about depression
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Australia’s Therapeutic Goods Administration (TGA) recently issued a safety alert requiring extra warnings to be included with the asthma and hay fever drug montelukast.
The warnings are for users and their families to look for signs of serious behaviour and mood-related changes, such as suicidal thoughts and depression. The new warnings need to be printed at the start of information leaflets given to both patients and health-care providers (sometimes called a “boxed” warning).
So why did the TGA issue this warning? And is there cause for concern if you or a family member uses montelukast? Here’s what you need to know.
First, what is montelukast?
Montelukast is a prescription drug also known by its brand names which include Asthakast, Lukafast, Montelair and Singulair. It’s used to manage the symptoms of mild-to-moderate asthma and seasonal hay fever in children and adults.
Asthma occurs when the airways tighten and produce extra mucus, which makes it difficult to get air into the lungs. Likewise, the runny nose characteristic of hay fever occurs due to the overproduction of mucus.
Leukotrienes are an important family of chemicals found throughout the airways and involved in both mucus production and airway constriction. Montelukast is a cysteinyl leukotriene receptor antagonist, meaning it blocks the site in the airways where the leukotrienes work.
Montelukast can’t be used to treat acute asthma (an asthma attack), as it takes time for the tablet to be broken down in the stomach and for it to be absorbed into the body. Rather, it’s taken daily to help prevent asthma symptoms or seasonal hay fever.
It can be used alongside asthma puffers that contain corticosteriods and drugs like salbutamol (Ventolin) in the event of acute attacks.
What is the link to depression and suicide?
The possibility that this drug may cause behavioural changes is not new information. Manufacturers knew this as early as 2007 and issued warnings for possible side-effects including depression, suicidality and anxiousness.
The United Kingdom’s Medicines and Healthcare products Regulatory Agency has required a warning since 2008 but mandated a more detailed warning in 2019. The United States’ Food and Drug Administration has required boxed warnings for the drug since 2020.
Montelukast can help children and adults with asthma. adriaticfoto/Shutterstock Montelukast is known to potentially induce a number of behaviour and mood changes, including agitation, anxiety, depression, irritability, obsessive-compulsive symptoms, and suicidal thoughts and actions.
Initially a 2009 study that analysed data from 157 clinical trials involving more than 20,000 patients concluded there were no completed suicides due to taking the drug, and only a rare risk of suicide thoughts or attempts.
The most recent study, published in November 2024, examined data from more than 100,000 children aged 3–17 with asthma or hay fever who either took montelukast or used only inhaled corticosteroids.
It found montelukast use was associated with a 32% higher incidence of behavioural changes. The behaviour change with the strongest association was sleep disturbance, but montelukast use was also linked to increases in anxiety and mood disorders.
In the past ten years, around 200 incidences of behavioural side-effects have been reported to the TGA in connection with montelukast. This includes 57 cases of depression, 60 cases of suicidal thoughts and 17 suicide attempts or incidents of intentional self-injury. There were seven cases where patients taking the drug did complete a suicide.
This is of course tragic. But these numbers need to be seen in the context of the number of people taking the drug. Over the same time period, more than 200,000 scripts for montelukast have been filled under the Pharmaceutical Benefits Scheme.
Overall, we don’t know conclusively that montelukast causes depression and suicide, just that it seems to increase the risk for some people.
We’re still not sure how the drug can act on the brain to lead to behaviour changes. Elif Bayraktar/Shutterstock And if it does change behaviour, we don’t fully understand how this happens. One hypothesis is that the drug and its breakdown products (or metabolites) affect brain chemistry.
Specifically, it might interfere with how the brain detoxifies the antioxidant glutathione or alter the regulation of other brain chemicals, such as neurotransmitters.
Why is the TGA making this change now?
The new risk warning requirement comes from a meeting of the Australian Advisory Committee on Medicines where they were asked to provide advice on ways to minimise the risk for the drug given current international recommendations.
Even though the 2024 review didn’t highlight any new risks, to align with international recommendations, and help address consumer concerns, the advisory committee recommended a boxed warning be added to drug information sheets.
If you have asthma and take montelukast (or your child does), you should not just stop taking the drug, because this could put you at risk of an attack that could be life threatening. If you’re concerned, speak to your doctor who can discuss the risks and benefits of the medication for you, and, if appropriate, prescribe a different medication.
If this article has raised issues for you, or if you’re concerned about someone you know, call Lifeline on 13 11 14.
Nial Wheate, Professor of Pharmaceutical Chemistry, Macquarie University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Greek Yogurt vs Cottage Cheese – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing Greek yogurt to cottage cheese, we picked the yogurt.
Why?
These are both dairy products popularly considered healthy, mostly for their high-protein, low-carb, low-fat profile. We’re going to assume that both were made without added sugars. Thus, their macro profiles are close to identical, and nothing between them there.
In the category of vitamins, both are a good source of some B vitamins, and neither are good source of much else. The B-vitamins they have most of, B2 and B12, Greek yogurt has more.
We’ll call this a small win for Greek yogurt.
As they are dairy products, you might have expected them to contain vitamin D—however (unless they have been artificially fortified, as is usually done with plant-based equivalents) they contain none or trace amounts only.
When it comes to minerals, both are reasonable sources of calcium, selenium, and phosphorus. Of these, they’re equal on the selenium, while cottage cheese has more phosphorus and Greek yogurt has more calcium.
Since it’s also a mineral (even if it’s usually one we’re more likely to be trying to get less of), it’s also worth noting here that cottage cheese is quite high in sodium, while Greek yogurt is not.
Another win for Greek yogurt.
Beyond those things, we’d be remiss not to mention that Greek yogurt contains plenty of probiotic bacteria, while cottage cheese does not.
Want to learn more?
You might like to read:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
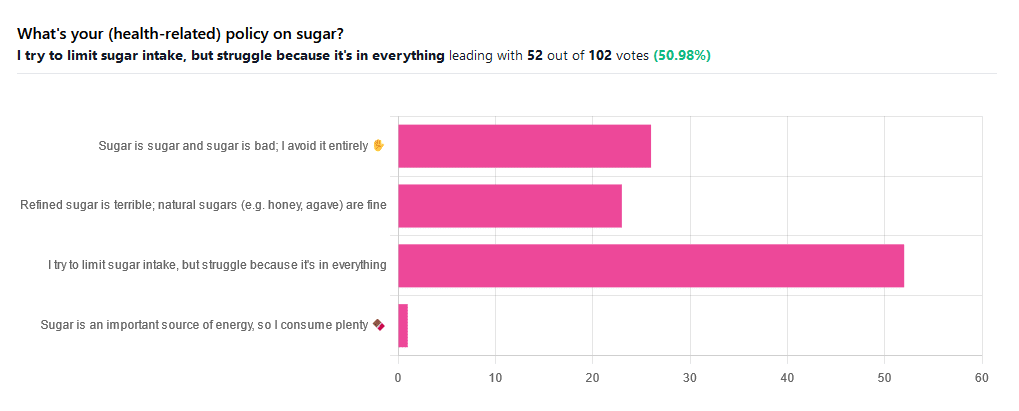
Which Sugars Are Healthier, And Which Are Just The Same?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
From Apples to Bees, and High-Fructose Cs
We asked you for your (health-related) policy on sugar. The trends were as follows:
- About half of all respondents voted for “I try to limit sugar intake, but struggle because it’s in everything”
- About a quarter of all respondents voted for “Refined sugar is terrible; natural sugars (e.g. honey, agave) are fine”
- About a quarter of all respondents voted for “Sugar is sugar and sugar is bad; I avoid it entirely”
- One (1) respondent voted for “Sugar is an important source of energy, so I consume plenty”
Writer’s note: I always forget to vote in these, but I’d have voted for “I try to limit sugar intake, but struggle because it’s in everything”.
Sometimes I would like to make my own [whatever] to not have the sugar, but it takes so much more time, and often money too.
So while I make most things from scratch (and typically spend about an hour cooking each day), sometimes store-bought is the regretfully practical timesaver/moneysaver (especially when it comes to condiments).
So, where does the science stand?
There has, of course, been a lot of research into the health impact of sugar.
Unfortunately, a lot of it has been funded by sugar companies, which has not helped. Conversely, there are also studies funded by other institutions with other agendas to push, and some of them will seek to make sugar out to be worse than it is.
So for today’s mythbusting overview, we’ve done our best to quality-control studies for not having financial conflicts of interest. And of course, the usual considerations of favoring high quality studies where possible Large sample sizes, good method, human subjects, that sort of thing.
Sugar is sugar and sugar is bad: True or False?
False and True, respectively.
- Sucrose is sucrose, and is generally bad.
- Fructose is fructose, and is worse.
Both ultimately get converted into glycogen (if not used immediately for energy), but for fructose, this happens mostly* in the liver, which a) taxes it b) goes very unregulated by the pancreas, causing potentially dangerous blood sugar spikes.
This has several interesting effects:
- Because fructose doesn’t directly affect insulin levels, it doesn’t cause insulin insensitivity (yay)
- Because fructose doesn’t directly affect insulin levels, this leaves hyperglycemia untreated (oh dear)
- Because fructose is metabolized by the liver and converted to glycogen which is stored there, it’s one of the main contributors to non-alcoholic fatty liver disease (at this point, we’re retracting our “yay”)
Read more: Fructose and sugar: a major mediator of non-alcoholic fatty liver disease
*”Mostly” in the liver being about 80% in the liver. The remaining 20%ish is processed by the kidneys, where it contributes to kidney stones instead. So, still not fabulous.
Fructose is very bad, so we shouldn’t eat too much fruit: True or False?
False! Fruit is really not the bad guy here. Fruit is good for you!
Fruit does contain fructose yes, but not actually that much in the grand scheme of things, and moreover, fruit contains (unless you have done something unnatural to it) plenty of fiber, which mitigates the impact of the fructose.
- A medium-sized apple (one of the most sugary fruits there is) might contain around 11g of fructose
- A tablespoon of high-fructose corn syrup can have about 27g of fructose (plus about 3g glucose)
Read more about it: Effects of high-fructose (90%) corn syrup on plasma glucose, insulin, and C-peptide in non-insulin-dependent diabetes mellitus and normal subjects
However! The fiber content (in fruit) mitigates the impact of the fructose almost entirely anyway.
And if you take fruits that are high in sugar and/but high in polyphenols, like berries, they now have a considerable net positive impact on glycemic health:
- Polyphenols and Glycemic Control
- Polyphenols and their effects on diabetes management: A review
- Dietary polyphenols as antidiabetic agents: Advances and opportunities
You may be wondering: what was that about “unless you have done something unnatural to it”?
That’s mostly about juicing. Juicing removes much (or all) of the fiber, and if you do that, you’re basically back to shooting fructose into your veins:
- Effect of Fruit Juice on Glucose Control and Insulin Sensitivity in Adults: A Meta-Analysis of 12 Randomized Controlled Trials
- Intake of Fruit, Vegetables, and Fruit Juices and Risk of Diabetes in Women
Natural sugars like honey, agave, and maple syrup, are healthier than refined sugars: True or False?
True… Sometimes, and sometimes marginally.
This is partly because of the glycemic index and glycemic load. The glycemic index scores tail off thus:
- table sugar = 65
- maple syrup = 54
- honey = 46
- agave syrup = 15
So, that’s a big difference there between agave syrup and maple syrup, for example… But it might not matter if you’re using a very small amount, which means it may have a high glycemic index but a low glycemic load.
Note, incidentally, that table sugar, sucrose, is a disaccharide, and is 50% glucose and 50% fructose.
The other more marginal health benefits come from that fact that natural sugars are usually found in foods high in other nutrients. Maple syrup is very high in manganese, for example, and also a fair source of other minerals.
But… Because of its GI, you really don’t want to be relying on it for your nutrients.
Wait, why is sugar bad again?
We’ve been covering mostly the more “mythbusting” aspects of different forms of sugar, rather than the less controversial harms it does, but let’s give at least a cursory nod to the health risks of sugar overall:
- Obesity and associated metabolic risk
- Main contributor to non-alcoholic fatty liver disease
- Increased risk of heart disease
- Insulin resistance and diabetes risk
- Cellular aging (shortened telomeres)
- 95% increased cancer risk
That last one, by the way, was a huge systematic review of 37 large longitudinal cohort studies. Results varied depending on what, specifically, was being examined (e.g. total sugar, fructose content, sugary beverages, etc), and gave up to 200% increased cancer risk in some studies on sugary beverages, but 95% increased risk is a respectable example figure to cite here, pertaining to added sugars in foods.
And finally…
The 56 Most Common Names for Sugar (Some Are Tricky)
How many did you know?
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: