Cordyceps: Friend Or Foe?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Cordyceps: friend or foe?
Cordyceps is a famously frightening fungus. It’s the one responsible for “zombie ants” and other zombie creatures, and it’s the basis for the existential threat to humanity in the TV show The Last of Us.
It’s a parasitic fungus that controls the central and peripheral nervous systems of its host, slowly replacing the host’s body, as well as growing distinctive spines that erupt out of the host’s body. Taking over motor functions, it compels the host to do two main things, which are to eat more food, and climb to a position that will be good to release spores from.
Fortunately, none of that matters to humans. Cordyceps does not (unlike in the TV show) affect humans that way.
What does Cordyceps do in humans?
Cordyceps (in various strains) is enjoyed as a health supplement, based on a long history of use in Traditional Chinese Medicine, and nowadays it’s coming under a scientific spotlight too.
The main health claims for it are:
- Against inflammation
- Against aging
- Against cancer
- For blood sugar management
- For heart health
- For exercise performance
Sounds great! What does the science say?
There’s a lot more science for the first three (which are all closely related to each other, and often overlapping in mechanism and effect).
So let’s take a look:
Against inflammation
The science looks promising for this, but studies so far have either been in vitro (cell cultures in petri dishes), or else murine in vivo (mouse studies), for example:
- Anti-inflammatory effects of Cordyceps mycelium in murine macrophages
- Cordyceps sinensis as an immunomodulatory agent
- Immunomodulatory functions of extracts from Cordyceps cicadae
- Cordyceps pruinosa inhibits in vitro and in vivo inflammatory mediators
In summary: we can see that it has anti-inflammatory properties for mice and in the lab; we’d love to see the results of studies done on humans, though. Also, while it has anti-inflammatory properties, it performed less well than commonly-prescribed anti-inflammatory drugs, for example:
❝C. militaris can modulate airway inflammation in asthma, but it is less effective than prednisolone or montelukast.❞
Against aging
Because examining the anti-aging effects of a substance requires measuring lifespans and repeating the experiment, anti-aging studies do not tend to be done on humans, because they would take lifetimes to perform. To this end, it’s inconvenient, but not a criticism of Cordyceps, that studies have been either mouse studies (short lifespan, mammals like us) or fruit fly studies (very short lifespan, genetically surprisingly similar to us).
The studies have had positive results, with typical lifespan extensions of 15–20%:
- The lifespan-extending effect of Cordyceps sinensis in normal mice
- Cordyceps sinensis oral liquid prolongs the lifespan of the fruit fly, Drosophila melanogaster
- Anti-aging activity of polysaccharides from Cordyceps militaris
- Anti-aging effect of Cordyceps sinensis extract
Against cancer
Once again, the studies here have been in vitro, or murine in vivo. They do look good though:
In vitro (human cell cultures in a lab):
In vivo (mouse studies):
Summary of these is: Cordyceps quite reliably inhibits tumor growth in vitro (human cell cultures) and in vivo (mouse studies). However, trials in human cancer patients are so far conspicuous by their absence.
For blood sugar management
Cordyceps appears to mimic the action of insulin, without triggering insulin sensitivity. For example:
The anti-hyperglycemic activity of the fruiting body of Cordyceps in diabetic rats
There were some other rat/mouse studies with similar results. No studies in humans yet.
For heart health
Cordyceps contains adenosine. You may remember that caffeine owes part of its stimulant effect to blocking adenosine, the hormone that makes us feel sleepy. So in this way, Cordyceps partially does the opposite of what caffeine does, and may be useful against arrhythmia:
Cardiovascular protection of Cordyceps sinensis act partially via adenosine receptors
For exercise performance
A small (30 elderly participants) study found that Cordyceps supplementation improved VO2 max by 7% over the course of six weeks:
However, another small study (22 young athletes) failed to reproduce those results:
Cordyceps Sinensis supplementation does not improve endurance exercise performance
In summary…
Cordyceps almost certainly has anti-inflammation, anti-aging, and anti-cancer benefits.
Cordyceps may have other benefits too, but the evidence is thinner on the ground for those, so far.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Safe Effective Sleep Aids For Seniors
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Safe Efective Sleep Aids For Seniors
Choosing a safe, effective sleep aid can be difficult, especially as we get older. Take for example this research review, which practically says, when it comes to drugs, “Nope nope nope nope nope, definitely not, we don’t know, wow no, useful in one (1) circumstance only, definitely not, fine if you must”:
Review of Safety and Efficacy of Sleep Medicines in Older Adults
Let’s break it down…
What’s not so great
Tranquilizers aren’t very healthy ways to get to sleep, and are generally only well-used as a last resort. The most common of these are benzodiazepines, which is the general family of drugs with names usually ending in –azepam and –azolam.
Their downsides are many, but perhaps their biggest is their tendency to induce tolerance, dependence, and addiction.
Non-benzo hypnotics aren’t fabulous either. Z-drugs such as zolpidem tartrate (popularly known by the brand name Ambien, amongst others), comes with warnings that it shouldn’t be prescribed if you have sleep apnea (i.e., one of the most common causes of insomnia), and should be used only with caution in patients who have depression or are elderly, as it may cause protracted daytime sedation and/or ataxia.
See also: Benzodiazepine and z-drug withdrawal
(and here’s a user-friendly US-based resource for benzodiazepine addiction specifically)
Antihistamines are commonly sold as over-the-counter sleep aids, because they can cause drowsiness, but a) they often don’t b) they may reduce your immune response that you may actually need for something. They’re still a lot safer than tranquilizers, though.
What about cannabis products?
We wrote about some of the myths and realities of cannabis use yesterday, but it does have some medical uses beyond pain relief, and use as a sleep aid is one of them—but there’s another caveat.
How it works: CBD, and especially THC, reduces REM sleep, causing you to spend longer in deep sleep. Deep sleep is more restorative and restful. And, if part of your sleep problem was nightmares, they can only occur during REM sleep, so you’ll be skipping those, too. However, REM sleep is also necessary for good brain health, and missing too much of it will result in cognitive impairment.
Opting for a CBD product that doesn’t contain THC may improve sleep with less (in fact, no known) risk of long-term impairment.
See: Cannabis, Cannabinoids, and Sleep: a Review of the Literature
Melatonin: a powerful helper with a good safety profile
We did a main feature on this recently, so we won’t take up too much space here, but suffice it to say: melatonin is our body’s own natural sleep hormone, and our body is good at scrubbing it when we see white/blue light (so, look at such if you feel groggy upon awakening, and it should clear up quickly), so that and its very short elimination half-life again make it quite safe.
Unlike tranquilizers, we don’t develop a tolerance to it, let alone dependence or addiction, and unlike cannabis, it doesn’t produce long-term adverse effects (after all, our brains are supposed to have melatonin in them every night). You can read our previous main feature (including a link to get melatonin, if you want) here:
Melatonin: A Safe Natural Sleep Supplement
Herbal options: which really work?
Valerian? Probably not, but it seems safe to try. Data on this is very inconsistent, and many studies supporting it had poor methodology. Shinjyo et al. also hypothesized that the inconsistency may be due to the highly variable quality of the supplements, and lack of regulation, as they are provided “based on traditional use only”.
Chamomile? Given the fame of chamomile tea as a soothing, relaxing bedtime drink, there’s surprisingly little research out there for this specifically (as opposed to other medicinal features of chamomile, of which there are plenty).
But here’s one study that found it helped significantly:
The effects of chamomile extract on sleep quality among elderly people: A clinical trial
Unlike valerian, which is often sold as tablets, chamomile is most often sold as a herbal preparation for making chamomile tea, so the quality is probably quite consistent. You can also easily grow your own in most places!
Technological interventions
We may not have sci-fi style regeneration alcoves just yet, but white noise machines, or better yet, pink noise machines, help:
White Noise Is Good; Pink Noise Is Better
Note: the noise machine can be a literal physical device purchased to do that (most often sold as for babies, but babies aren’t the only ones who need to sleep!), but it can also just be your phone playing an appropriate audio file (there are apps available) or YouTube video.
We reviewed some sleep apps; you might like those too:
The Head-To-Head Of Google and Apple’s Top Apps For Getting Your Head Down
Enjoy, and rest well!
Share This Post
-
Ex-Cyclone Alfred has left flooding in its wake. Here’s how floods affect our health
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Ex-Cyclone Alfred is bringing significant rainfall to southeast Queensland and the Northern Rivers of New South Wales. Flooding has hit Lismore, Ballina, Grafton, Brisbane and Hervey Bay, which received 150 mm of rainfall in two hours this morning.
Tragically, a 61-year-old man died after being swept away in floodwaters near Dorrigo in northern New South Wales.
More heavy rain and flash flooding is expected in the coming days as the weather system moves inland and weakens.
Climate change is making these weather events more intense and frequent. Earlier this year, far north Queensland experienced major flooding. As residents of the Northern Rivers, this latest disaster is especially tough because only three years ago we faced the catastrophic 2022 floods.
We’ve studied the impact of floods on human health and wellbeing, and found floods are linked to a range of physical and mental health effects in both the short- and long-term.
So what might you experience if you live in an area affected by these floods?
We reviewed the evidence
We recently reviewed research on the physical and mental health impacts of floods across mainland Australia. We included 69 studies in our review, published over 70 years. The majority were from the past ten years, examining the effects of floods in Queensland and NSW.
These studies suggest people can expect a range of health impacts. Immediate physical health effects of floods include drowning, falls and injuries.
Chronic diseases such as diabetes or renal disease can also worsen due to factors such as reduced access to transport, health-care services, medications and hospitals.
Exposure to contaminated floodwaters can lead to skin infections, while respiratory problems can occur due to mould and damp housing in the aftermath of floods.
Floods also create ideal conditions for mosquito borne infections such as Ross River virus and Murray Valley encephalitis, while also spreading infectious diseases including leptospirosis, a bacterial infection from contaminated soil.
There are mental health consequences too
Our review showed floods also affect mental health. The more you’re exposed to floodwaters in your home or business, the worse the mental health impacts are likely to be.
The After the Flood study examined mental health and wellbeing outcomes six months after the 2017 flood in the Northern Rivers. It found people who had floodwater in their home, yard or business, or who were displaced from their home for a more than six months, were much more likely to have probable post-traumatic stress disorder, anxiety or depression, compared to those who didn’t experience flooding or weren’t displaced.
Repeated natural disasters could compound these mental health consequences. Southeast Queensland and the Northern Rivers in NSW have experienced multiple disasters over recent years. The Northern Rivers faced major flooding in 2017, bushfires in 2020, further major floods in 2022, and now Cyclone Alfred in 2025. These repeated disasters have taken a toll on our community, creating a seemingly never-ending cycle of recovery, rebuilding and preparation for the next disaster.
Our understanding of the unique challenges faced by communities which experience multiple disasters is still growing. However, a recent Australian study showed exposure to repeated disasters has a compounding effect on people’s mental health, leading to worse mental health outcomes compared to people who experience a single disaster.
Mums and babies
The health effects of floods extend far beyond the initial emergency and beyond the infections and mental health consequences you might expect.
The Queensland Flood Study tracked pregnant women exposed to the 2011 Brisbane floods. Researchers assessed mothers’ stress related to the flood and tracked them and their children at six weeks old, six months, 16 months, 2.5 years, four and six years. It found some links between prenatal stress and developmental outcomes in children.
Some evidence suggests maternal stress from floods can affect children’s development. Nastyaofly/Shutterstock While the health effects after flooding are diverse, the research to date is not comprehensive. We need to learn more about how floods contribute to or exacerbate existing chronic illnesses, disability and long-term mental health issues.
The impacts are inequitable
Flooding exposes and worsens existing inequalities. Socially vulnerable groups are more likely to be exposed to flooding in their homes and have less access to resources to respond and recover from these events, putting some groups at higher risk of negative health impacts afterwards.
Some research has looked at the disproportionate impacts on people with disabilities and their carers, First Nations communities and people from disadvantaged backgrounds.
After the 2017 Northern Rivers floods, for example, people with disability and their carers were more likely than others to:
- experience disrupted access to food, support networks and essentials such as health care and social services
- continue to be distressed about the flood six months after it happened
- be at relatively high risk of post-traumatic stress disorder six months after the flood.
However, targeted flood research exploring the experiences of these vulnerable groups in Australia is limited.
Moving forward, it’s vital we examine the varied impacts of flood events for more vulnerable groups, so we can better support them in the wake of devastating events such as Cyclone Alfred.
If this article has raised issues for you, or if you’re concerned about someone you know, call Lifeline on 13 11 14.
Jodie Bailie, Senior Research Fellow, The University Centre for Rural Health and The Centre for Disability Research and Policy, University of Sydney; Jo Longman, Senior Research Fellow, The University Centre for Rural Health, University of Sydney; Rebecca McNaught, Research Fellow, Rural and Remote Health, University of Sydney, and Ross Bailie, School of Public Health, Honorary Professor, University of Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
What’s the difference between burnout and depression?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
If your summer holiday already feels like a distant memory, you’re not alone. Burnout – a state of emotional, physical and mental exhaustion following prolonged stress – has been described in workplaces since a 5th century monastery in Egypt.
Burnout and depression can look similar and are relatively common conditions. It’s estimated that 30% of the Australian workforce is feeling some level of burnout, while almost 20% of Australians are diagnosed with depression at some point in their lives.
So what’s the difference between burnout and depression?
Burnout is marked by helplessness and depression by hopelessness. They can have different causes and should also be managed differently.
Yuri A/Shutterstock What is burnout?
The World Health Organization defines burnout as an “occupational phenomenon” resulting from excessively demanding workload pressures. While it is typically associated with the workplace, carers of children or elderly parents with demanding needs are also at risk.
Our research created a set of burnout symptoms we captured in the Sydney Burnout Measure to assist self-diagnosis and clinicians undertaking assessments. They include:
- exhaustion as the primary symptom
- brain fog (poor concentration and memory)
- difficulty finding pleasure in anything
- social withdrawal
- an unsettled mood (feeling anxious and irritable)
- impaired work performance (this may be result of other symptoms such as fatigue).
People can develop a “burning out” phase after intense work demands over only a week or two. A “burnout” stage usually follows years of unrelenting work pressure.
What is depression?
A depressive episode involves a drop in self-worth, increase in self-criticism and feelings of wanting to give up. Not everyone with these symptoms will have clinical depression, which requires a diagnosis and has an additional set of symptoms.
Clinically diagnosed depression can vary by mood, how long it lasts and whether it comes back. There are two types of clinical depression:
- melancholic depression has genetic causes, with episodes largely coming “out of the blue”
- non-melancholic depression is caused by environmental factors, often triggered by significant life events which cause a drop in self-worth.
When we created our burnout measure, we compared burnout symptoms with these two types of depression.
Burnout shares some features with melancholic depression, but they tend to be general symptoms, such as feeling a loss of pleasure, energy and concentration skills.
We found there were more similarities between burnout and non-melancholic (environmental) depression. This included a lack of motivation and difficulties sleeping or being cheered up, perhaps reflecting the fact both have environmental causes.
Looking for the root cause
The differences between burnout and depression become clearer when we look at why they happen.
Personality comes into play. Our work suggests a trait like perfectionism puts people at a much higher risk of burnout. But they may be less likely to become depressed as they tend to avoid stressful events and keep things under control.
Excessive workloads can contribute to burnout. tartanparty/Shutterstock Those with burnout generally feel overwhelmed by demands or deadlines they can’t meet, creating a sense of helplessness.
On the other hand, those with depression report lowered self-esteem. So rather than helpless they feel that they and their future is hopeless.
However it is not uncommon for someone to experience both burnout and depression at once. For example, a boss may place excessive work demands on an employee, putting them at risk of burnout. At the same time, the employer may also humiliate that employee and contribute to an episode of non-melancholic depression.
What can you do?
A principal strategy in managing burnout is identifying the contributing stressors. For many people, this is the workplace. Taking a break, even a short one, or scheduling some time off can help.
Australians now have the right to disconnect, meaning they don’t have to answer work phone calls or emails after hours. Setting boundaries can help separate home and work life.
Burnout can be also be caused by compromised work roles, work insecurity or inequity. More broadly, a dictatorial organisational structure can make employees feel devalued. In the workplace, environmental factors, such as excessive noise, can be a contributor. Addressing these factors can help prevent burnout.
As for managing symptoms, the monks had the right idea. Strenuous exercise, meditation and mindfulness are effective ways to deal with everyday stress.
Regular exercise can help manage symptoms of burnout. alexei_tm/Shutterstock Deeper contributing factors, including traits such as perfectionism, should be managed by a skilled clinical psychologist.
For melancholic depression, clinicians will often recommend antidepressant medication.
For non-melancholic depression, clinicians will help address and manage triggers that are the root cause. Others will benefit from antidepressants or formal psychotherapy.
While misdiagnosis between depression and burnout can occur, burnout can mimic other medical conditions such as anemia or hypothyroidism.
For the right diagnosis, it’s best to speak to your doctor or clinician who should seek to obtain a sense of “the whole picture”. Only then, once a burnout diagnosis has been affirmed and other possible causes ruled out, should effective support strategies be put in place.
If this article has raised issues for you, or if you’re concerned about someone you know, call Lifeline on 13 11 14.
Correction: This article originally stated that depression is marked by helplessness and burnout by hopelessness, when in fact it is vice versa. This has been amended.
Gordon Parker, Scientia Professor of Psychiatry, UNSW Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
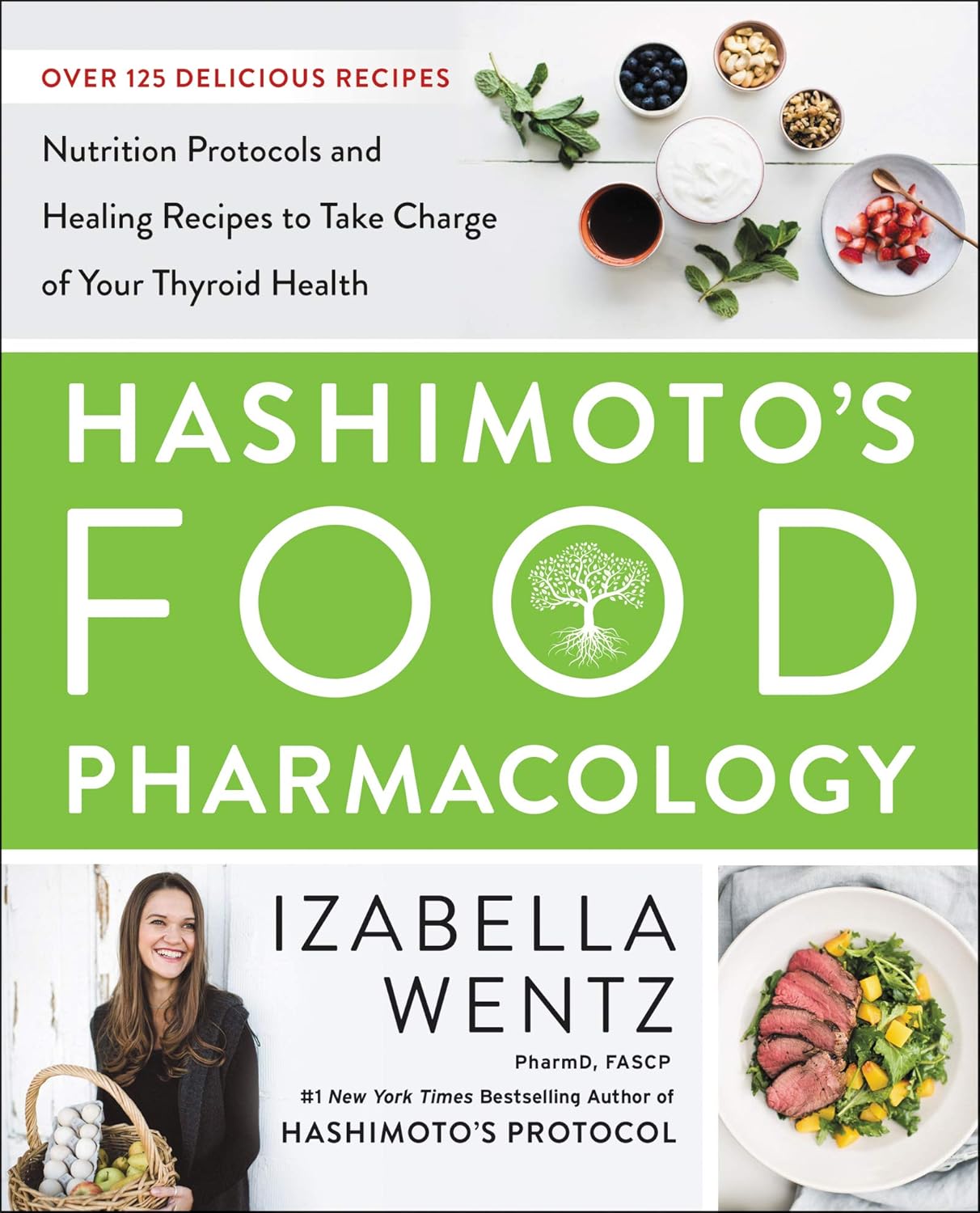
Hashimoto’s Food Pharmacology – by Dr. Izabella Wentz
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The author is a doctor of pharmacology, and we’ve featured her before as an expert on Hashimoto’s, which she has. She has recommendations about specific blood tests and medications, but in this book she’s mainly focussing on what she calls the “three Rs” of managing hypothyroidism:
- Remove the causes and triggers of your hypothyroidism, so far as possible
- Repair the damage caused to your body, especially your gut
- Replace the thyroid hormones and related things in which your body has become deficient
To this end, she provides recipes that avoid processed meats and unfermented dairy, and include plenty of nutrient-dense whole foods specifically tailored to meet the nutritional needs of someone with hypothyroidism.
A nice bonus of the presentation of recipes (of which there are 125, if we include things like “mint tea” and “tomato sauce” and “hot lemon water” as recipes) is explaining the thyroid-supporting elements of each recipe.
A downside for some will be that if you are vegetarian/vegan, this book is very much not, and since many recipes are paleo-style meat dishes, substitutions will change the nutritional profile completely.
Bottom line: if you have hypothyroidism (especially if: Hashimoto’s) and like meat, this will be a great recipe book for you.
Click here to check out Hashimoto’s Food Pharmacology, and get cooking!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Play Bold – by Magnus Penker
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This book is very different to what you might expect, from the title.
We often see: “play bold, believe in yourself, the universe rewards action” etc… Instead, this one is more: “play bold, pay attention to the data, use these metrics, learn from what these businesses did and what their results were”, etc.
We often see: “here’s an anecdote about a historical figure and/or celebrity who made a tremendous bluff and it worked out well so you should too” etc… Instead, this one is more: “see how what we think of as safety is actually anything but! And how by embracing change quickly (or ideally: proactively), we can stay ahead of disaster that may otherwise hit us”.
Penker’s background is also relevant here. He has decades of experience, having “launched 10 start-ups and acquired, turned around, and sold over 30 SMEs all over Europe”. Importantly, he’s also “still in the game”… So, unlike many authors whose last experience in the industry was in the 1970s and who wonder why people aren’t reaping the same rewards today!
Penker is the therefore opposite of many who advocate to “play bold” but simply mean “fail fast, fail often”… While quietly relying on their family’s capital and privilege to leave a trail of financial destruction behind them, and simultaneously gloating about their imagined business expertise.
In short: boldness does not equate to foolhardiness, and foolhardiness does not equate to boldness.
As for telling the difference? Well, for that we recommend reading the book—It’s a highly instructive one.
Take The First Bold Step Of Checking Out This Book On Amazon!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How To Reduce The Harm Of Festive Drinking (Without Abstaining)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How To Reduce The Harm Of Festive Drinking
Not drinking alcohol is—of course—the best way to avoid the harmful effects of alcohol. However, not everyone wants to abstain, especially at this time of year, so today we’re going to be focusing on harm reduction without abstinence.
If you do want to quit (or even reduce) drinking, you might like our previous article about that:
For everyone else, let’s press on with harm reduction:
Before You Drink
A common (reasonable, but often unhelpful) advice is “set yourself a limit”. The problem with this is that when we’re sober, “I will drink no more than n drinks” is easy. After the first drink, we start to feel differently about it.
So: delay your first drink of the day for as long as possible
That’s it, that’s the tip. The later you start drinking, not only will you likely drink less, but also, your liver will have had longer to finish processing whatever you drank last night, so it’s coming at the new drink(s) fresh.
On that note…
Watch your meds! Often, especially if we are taking medications that also tax our liver (acetaminophen / paracetamol / Tylenol is a fine example of this), we are at risk of having a bit of a build-up, like an office printer that still chewing on the last job while you’re trying to print the next.
Additionally: do indeed eat before you drink.
While You Drink
Do your best to drink slowly. While this can hit the same kind of problem as the “set yourself a limit” idea, in that once you start drinking you forget to drink slowly, it’s something to try for.
If your main reason for drinking is the social aspect, then merely having a drink in your hand is generally sufficient. You don’t need to be keeping pace with anyone.
It is further good to alternate your drinks with water. As in, between each alcoholic drink, have a glass of water. This helps in several ways:
- Hydrates you, which is good for your body’s recovery abilities
- Halves the amount of time you spend drinking
- Makes you less thirsty; it’s easy to think “I’m thirsty” and reach for an alcoholic drink that won’t actually help. So, it may slow down your drinking for that reason, too.
At the dinner table especially, it’s very reasonable to have two glasses, one filled with water. Nobody will be paying attention to which glass you drink from more often.
After You Drink
Even if you are not drunk, assume that you are.
Anything you wouldn’t let a drunk person in your care do, don’t do. Now is not the time to drive, have a shower, or do anything you wouldn’t let a child do in the kitchen.
Hospital Emergency Rooms, every year around this time, get filled up with people who thought they were fine and then had some accident.
The biggest risks from alcohol are:
- Accidents
- Heart attacks
- Things actually popularly associated with alcohol, e.g. alcohol poisoning etc
So, avoiding accidents is as important as, if not more important than, avoiding damage to your liver.
Drink some water, and eat something.
Fruit is great, as it restocks you on vitamins, minerals, and water, while being very easy to digest.
Go to bed.
There is a limit to how much trouble you can get into there. Sleep it off.
In the morning, do not do “hair of the dog”; drinking alcohol will temporarily alleviate a hangover, but only because it kicks your liver back into an earlier stage of processing the alcohol—it just prolongs the inevitable.
Have a good breakfast, instead. Remember, fruit is your friend (as explained above).
Want to know more?
Here’s a great service with a lot of further links to a lot more resources:
With You | How to safely detox from alcohol at home
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: