Taurine’s Benefits For Heart Health And More
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Taurine: Research Review
First, what is taurine, beyond being an ingredient in many energy drinks?
It’s an amino acid that many animals, including humans, can synthesize in our bodies. Some other animals—including obligate carnivores such as cats (but not dogs, who are omnivorous by nature) cannot synthesize taurine and must get it from food.
So, as humans are very versatile omnivorous frugivores by nature, we have choices:
- Synthesize it—no need for any conscious action; it’ll just happen
- Eat it—by eating meat, which contains taurine
- Supplement it—by taking supplements, including energy drinks, which generally (but not always) use a bioidentical lab-made taurine. Basically, lab-made taurine is chemically identical to the kind found in meat, it’s just cheaper and doesn’t involve animals as a middleman.
What does it do?
Taurine does a bunch of essential things, including:
- Maintaining hydration/electrolyte balance in cells
- Regulating calcium/magnesium balance in cells
- Forming bile salts, which are needed for digestion
- Supporting the integrity of the central nervous system
- Regulating the immune system and antioxidative processes
Thus, a shortage of taurine can lead to such issues as kidney problems, eye tissue damage (since the eyes are a particularly delicate part of the CNS), and cardiomyopathy.
If you want to read more, here’s an academic literature review:
Taurine: A “very essential” amino acid
On the topic of eye health, a 2014 study found that taurine is the most plentiful amino acid in the eye, and helps protect against retinal degeneration, in which they say:
❝We here review the evidence for a role of taurine in retinal ganglion cell survival and studies suggesting that this compound may be involved in the pathophysiology of glaucoma or diabetic retinopathy. Along with other antioxidant molecules, taurine should therefore be seriously reconsidered as a potential treatment for such retinal diseases❞
Read more: Taurine: the comeback of a neutraceutical in the prevention of retinal degenerations
Taurine for muscles… In more than sports!
We’d be remiss not to mention that taurine is enjoyed by athletes to enhance athletic performance; indeed, it’s one of its main selling-points:
See: Taurine in sports and exercise
But! It’s also useful for simply maintaining skeleto-muscular health in general, and especially in the context of age-related decline and chronic disease:
Taurine: the appeal of a safe amino acid for skeletal muscle disorders
On the topic of safety… How safe is it?
There’s an interesting answer to that question. Within safe dose ranges (we’ll get to that), taurine is not only relatively safe, but also, studies that looked to explore its risks found new benefits in the process. Specifically of interest to us were that it appears to promote better long-term memory, especially as we get older (as taurine levels in the brain decline with age):
Taurine, Caffeine, and Energy Drinks: Reviewing the Risks to the Adolescent Brain
^Notwithstanding the title, we assure you, the research got there; they said:
❝Interestingly, the levels of taurine in the brain decreased significantly with age, which led to numerous studies investigating the potential neuroprotective effects of supplemental taurine in several different experimental models❞
What experimental models were those? These ones:
- Taurine protects cerebellar neurons of the external granular layer
- Effects of taurine on alterations of neurobehavior and neurodevelopment key proteins expression
- Neuroprotective role of taurine in developing offspring affected by maternal alcohol consumption
…which were all animal studies, however.
The same systematic review also noted that not only was more research needed on humans, but also, existing studies have had a strong bias to male physiology (in both human and assorted other animal studies), so more diverse study is needed too.
What are the safe dose ranges?
Before we get to toxicity, let’s look at some therapeutic doses. In particular, some studies that found that 500mg 3x daily, i.e. 1.5g total daily, had benefits for heart health:
- Taurine and atherosclerosis
- The Anti-Inflammatory Effect of Taurine on Cardiovascular Disease
- Taurine supplementation has anti-atherogenic and anti-inflammatory effects before and after incremental exercise in heart failure
- Taurine Supplementation Lowers Blood Pressure and Improves Vascular Function in Prehypertension
- Taurine improves the vascular tone through the inhibition of TRPC3 function in the vasculature
Bottom line on safety: 3g/day has been found to be safe:
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Dates vs Figs – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing dates to figs, we picked the dates.
Why?
Dates are higher in sugar, but also have a lower glycemic index than figs, which makes the sugar content much healthier. On the flipside, figs do have around 3x more fiber.
So far, so balanced.
When it comes to micronutrients though, dates take the prize much more clearly.
Dates have slightly more of most vitamins, and a lot more of most minerals.
In particular, dates are several times higher in copper, iron, magnesium, manganese, phosphorus, selenium, and zinc.
As for other phytochemical benefits going on:
- both are good against diabetes for reasons beyond the macros
- both have anti-inflammatory properties
- dates have anticancer properties
- dates have kidney-protecting properties
So in this last case, another win for dates.
Both are still great though, so do enjoy both!
Want to learn more?
You might like to read:
Which Sugars Are Healthier, And Which Are Just The Same?
Take care!
Share This Post
-
Celery vs Chard – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing celery to chard, we picked the chard.
Why?
In terms of macros, chard has more fiber, carbs, and protein, making it the more nutrient-dense option and thus the winner of the macros category.
In the category of vitamins, celery has more of vitamins B5 and B9, while chard has more of vitamins A, B1, B2, B3, B6, C, E, K, and choline—another win for chard.
When it comes to minerals, celery is not higher in any minerals, while chard has more calcium, copper, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc. One more very clear win for chard!
Looking at polyphenols, celery has very little to boast, about 3mg/100g furanocoumarins and nothing else, while chard has an impressive array of polyphenols, with 9mg/100g kaempferol and 7.5mg/100g quercetin atop the list of 12 polyphenols. Yet another win for chard.
Adding up the sections is not difficult arithmetic today: chard sweeps every category. But by all means enjoy either or both; diversity is good!
Want to learn more?
You might like:
Dr. Greger’s Daily Dozen ← the “dozen” in question includes getting a good amount of of leafy greens per day
Enjoy!
Share This Post
-
Nutritional Profiles to Recipes
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝I like the recipes. Most don’t seem to include nutritional profile. would lilke to see that. Macro/micro world…. Thank you❞
We’re glad you’re enjoying them! There are a couple of reasons why we don’t, but the reasons can be aggregated into one (admittedly rare) concept: honesty
To even try to give you these figures, we’d first need to use the metric system (or at least, a strictly mass-based system) which would likely not go well with our largely American readership, because “half a bulb of garlic, or more if you like”, and “1 cucumber” or “1 cup chopped carrot” could easily way half or twice as much, depending on the sizes of the vegetables or the chopping involved, and in the case of chopped vegetables measured by the cup, even the shape of the cup (because of geometry and the spaces left; it’s like Tetris in there). We can say “4 cups low-sodium broth” but we can’t say how much sodium is in your broth. And so on.
And that’s without getting into the flexibility we offer with substitutions, often at a rate of several per recipe.
We’d also need to strictly regulate your portion sizes for you, because we (with few exceptions, such as when they are a given number of burger patties, or a dessert-in-a-glass, etc) give you a recipe for a meal and leave it to you how you divide it and whether there’s leftovers.
Same goes for things like “Extra virgin olive oil for frying”; a recipe could say to use “2 tbsp” but let’s face it, you’re going to use what you need to use, and that’s going to change based on the size of your pan, how quickly it’s absorbed into the specific ingredients that you got, which will change depending on how fresh they are, and things like that.
By the time we’ve factored in your different kitchen equipment, how big your vegetables are, the many factors effecting how much oil you need, substitutions per recipe per making something dairy-free, or gluten-free, or nut-free, etc, how big your portion size is (we all know that “serves 4” is meaningless in reality)… Even an estimated average would be wildly misleading.
So, in a sea of recipes saying “500 kcal per serving” from the same authors who say you can caramelize onions in 4–5 minutes “or until caramelized” and then use the 4–5 minutes figure for calculating the overall recipe time… We prefer to stay honest.
PS: for any wondering, caramelizing onions takes closer to 45 minutes than 4–5 minutes, and again will depend on many factors, including the onions, how finely you chopped them, the size and surface of your pan, the fat you’re using, whether you add sugar, what kind, how much you stir them, the mood of your hob,
and the phase of the moon. Under very favorable circumstances, it could conceivably be rushed in 20 minutes or so, but it could also take 60. Slow-cooking them (i.e. in a crock pot) over 3–4 hours is a surprisingly viable “cheat” option, by the way. It’ll take longer, obviously, but provided you plan in advance, they’ll be ready when you need them, and perfectly done (the same claim cannot be made if you budgeted 4–5 minutes because you trusted a wicked and deceitful author who wants to poop your party).Take care!
Share This Post
Related Posts
-
If You’re Poor, Fertility Treatment Can Be Out of Reach
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Mary Delgado’s first pregnancy went according to plan, but when she tried to get pregnant again seven years later, nothing happened. After 10 months, Delgado, now 34, and her partner, Joaquin Rodriguez, went to see an OB-GYN. Tests showed she had endometriosis, which was interfering with conception. Delgado’s only option, the doctor said, was in vitro fertilization.
“When she told me that, she broke me inside,” Delgado said, “because I knew it was so expensive.”
Delgado, who lives in New York City, is enrolled in Medicaid, the federal-state health program for low-income and disabled people. The roughly $20,000 price tag for a round of IVF would be a financial stretch for lots of people, but for someone on Medicaid — for which the maximum annual income for a two-person household in New York is just over $26,000 — the treatment can be unattainable.
Expansions of work-based insurance plans to cover fertility treatments, including free egg freezing and unlimited IVF cycles, are often touted by large companies as a boon for their employees. But people with lower incomes, often minorities, are more likely to be covered by Medicaid or skimpier commercial plans with no such coverage. That raises the question of whether medical assistance to create a family is only for the well-to-do or people with generous benefit packages.
“In American health care, they don’t want the poor people to reproduce,” Delgado said. She was caring full-time for their son, who was born with a rare genetic disorder that required several surgeries before he was 5. Her partner, who works for a company that maintains the city’s yellow cabs, has an individual plan through the state insurance marketplace, but it does not include fertility coverage.
Some medical experts whose patients have faced these issues say they can understand why people in Delgado’s situation think the system is stacked against them.
“It feels a little like that,” said Elizabeth Ginsburg, a professor of obstetrics and gynecology at Harvard Medical School who is president-elect of the American Society for Reproductive Medicine, a research and advocacy group.
Whether or not it’s intended, many say the inequity reflects poorly on the U.S.
“This is really sort of standing out as a sore thumb in a nation that would like to claim that it cares for the less fortunate and it seeks to do anything it can for them,” said Eli Adashi, a professor of medical science at Brown University and former president of the Society for Reproductive Endocrinologists.
Yet efforts to add coverage for fertility care to Medicaid face a lot of pushback, Ginsburg said.
Over the years, Barbara Collura, president and CEO of the advocacy group Resolve: The National Infertility Association, has heard many explanations for why it doesn’t make sense to cover fertility treatment for Medicaid recipients. Legislators have asked, “If they can’t pay for fertility treatment, do they have any idea how much it costs to raise a child?” she said.
“So right there, as a country we’re making judgments about who gets to have children,” Collura said.
The legacy of the eugenics movement of the early 20th century, when states passed laws that permitted poor, nonwhite, and disabled people to be sterilized against their will, lingers as well.
“As a reproductive justice person, I believe it’s a human right to have a child, and it’s a larger ethical issue to provide support,” said Regina Davis Moss, president and CEO of In Our Own Voice: National Black Women’s Reproductive Justice Agenda, an advocacy group.
But such coverage decisions — especially when the health care safety net is involved — sometimes require difficult choices, because resources are limited.
Even if state Medicaid programs wanted to cover fertility treatment, for instance, they would have to weigh the benefit against investing in other types of care, including maternity care, said Kate McEvoy, executive director of the National Association of Medicaid Directors. “There is a recognition about the primacy and urgency of maternity care,” she said.
Medicaid pays for about 40% of births in the United States. And since 2022, 46 states and the District of Columbia have elected to extend Medicaid postpartum coverage to 12 months, up from 60 days.
Fertility problems are relatively common, affecting roughly 10% of women and men of childbearing age, according to the National Institute of Child Health and Human Development.
Traditionally, a couple is considered infertile if they’ve been trying to get pregnant unsuccessfully for 12 months. Last year, the ASRM broadened the definition of infertility to incorporate would-be parents beyond heterosexual couples, including people who can’t get pregnant for medical, sexual, or other reasons, as well as those who need medical interventions such as donor eggs or sperm to get pregnant.
The World Health Organization defined infertility as a disease of the reproductive system characterized by failing to get pregnant after a year of unprotected intercourse. It terms the high cost of fertility treatment a major equity issue and has called for better policies and public financing to improve access.
No matter how the condition is defined, private health plans often decline to cover fertility treatments because they don’t consider them “medically necessary.” Twenty states and Washington, D.C., have laws requiring health plans to provide some fertility coverage, but those laws vary greatly and apply only to companies whose plans are regulated by the state.
In recent years, many companies have begun offering fertility treatment in a bid to recruit and retain top-notch talent. In 2023, 45% of companies with 500 or more workers covered IVF and/or drug therapy, according to the benefits consultant Mercer.
But that doesn’t help people on Medicaid. Only two states’ Medicaid programs provide any fertility treatment: New York covers some oral ovulation-enhancing medications, and Illinois covers costs for fertility preservation, to freeze the eggs or sperm of people who need medical treatment that will likely make them infertile, such as for cancer. Several other states also are considering adding fertility preservation services.
In Delgado’s case, Medicaid covered the tests to diagnose her endometriosis, but nothing more. She was searching the internet for fertility treatment options when she came upon a clinic group called CNY Fertility that seemed significantly less expensive than other clinics, and also offered in-house financing. Based in Syracuse, New York, the company has a handful of clinics in upstate New York cities and four other U.S. locations.
Though Delgado and her partner had to travel more than 300 miles round trip to Albany for the procedures, the savings made it worthwhile. They were able do an entire IVF cycle, including medications, egg retrieval, genetic testing, and transferring the egg to her uterus, for $14,000. To pay for it, they took $7,000 of the cash they’d been saving to buy a home and financed the other half through the fertility clinic.
She got pregnant on the first try, and their daughter, Emiliana, is now almost a year old.
Delgado doesn’t resent people with more resources or better insurance coverage, but she wishes the system were more equitable.
“I have a medical problem,” she said. “It’s not like I did IVF because I wanted to choose the gender.”
One reason CNY is less expensive than other clinics is simply that the privately owned company chooses to charge less, said William Kiltz, its vice president of marketing and business development. Since the company’s beginning in 1997, it has become a large practice with a large volume of IVF cycles, which helps keep prices low.
At this point, more than half its clients come from out of state, and many earn significantly less than a typical patient at another clinic. Twenty percent earn less than $50,000, and “we treat a good number who are on Medicaid,” Kiltz said.
Now that their son, Joaquin, is settled in a good school, Delgado has started working for an agency that provides home health services. After putting in 30 hours a week for 90 days, she’ll be eligible for health insurance.
One of the benefits: fertility coverage.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
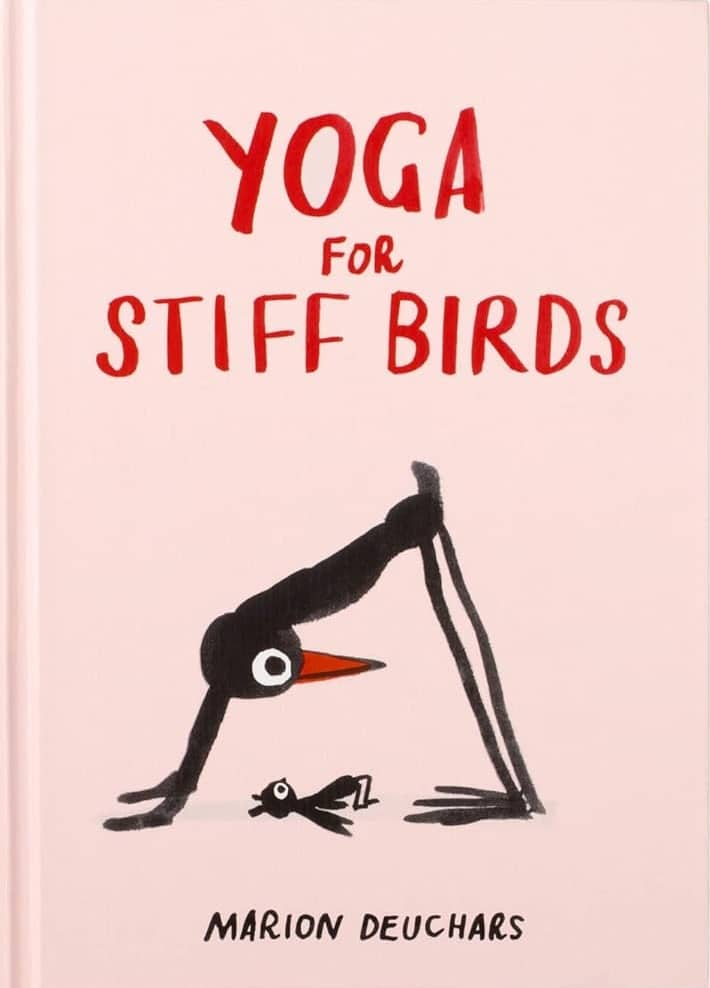
Yoga For Stiff Birds – by Marion Deuchars
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Quick show of hands, who here practices yoga in some fashion, but does not necessarily always look Instagrammable while doing it? Yep, same here.
This book is a surprisingly practical introduction to yoga for newcomers, and inspirational motivator for those of us who feel like we should do more.
Rather than studio photography of young models in skimpy attire, popular artist (and well-practised yogi) Marion Deuchars offers in a few brushstrokes what we need to know for each asana, and how to approach it if we’re not so supple yet as we’d like to be.
Bottom line: whether for yourself or as a gift for a loved one (or both!) this is a very charming introduction to (or refresher of) yoga.
Click here to check out Yoga For Stiff Birds, and get yours going!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Having an x-ray to diagnose knee arthritis might make you more likely to consider potentially unnecessary surgery
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Osteoarthritis is a leading cause of chronic pain and disability, affecting more than two million Australians.
Routine x-rays aren’t recommended to diagnose the condition. Instead, GPs can make a diagnosis based on symptoms and medical history.
Yet nearly half of new patients with knee osteoarthritis who visit a GP in Australia are referred for imaging. Osteoarthritis imaging costs the health system A$104.7 million each year.
Our new study shows using x-rays to diagnose knee osteoarthritis can affect how a person thinks about their knee pain – and can prompt them to consider potentially unnecessary knee replacement surgery.
pikselstock/Shutterstock What happens when you get osteoarthritis?
Osteoarthritis arises from joint changes and the joint working extra hard to repair itself. It affects the entire joint, including the bones, cartilage, ligaments and muscles.
It is most common in older adults, people with a high body weight and those with a history of knee injury.
Many people with knee osteoarthritis experience persistent pain and have difficulties with everyday activities such as walking and climbing stairs.
How is it treated?
In 2021–22, more than 53,000 Australians had knee replacement surgery for osteoarthritis.
Hospital services for osteoarthritis, primarily driven by joint replacement surgery, cost $3.7 billion in 2020–21.
While joint replacement surgery is often viewed as inevitable for osteoarthritis, it should only be considered for those with severe symptoms who have already tried appropriate non-surgical treatments. Surgery carries the risk of serious adverse events, such as blood clot or infection, and not everyone makes a full recovery.
Most people with knee osteoarthritis can manage it effectively with:
- education and self-management
- exercise and physical activity
- weight management (if necessary)
- medicines for pain relief (such as paracetamol and non-steroidal anti-inflammatory drugs).
Debunking a common misconception
A common misconception is that osteoarthritis is caused by “wear and tear”.
However, research shows the extent of structural changes seen in a joint on an x-ray does not reflect the level of pain or disability a person experiences, nor does it predict how symptoms will change.
Some people with minimal joint changes have very bad symptoms, while others with more joint changes have only mild symptoms. This is why routine x-rays aren’t recommended for diagnosing knee osteoarthritis or guiding treatment decisions.
Instead, guidelines recommend a “clinical diagnosis” based on a person’s age (being 45 years or over) and symptoms: experiencing joint pain with activity and, in the morning, having no joint-stiffness or stiffness that lasts less than 30 minutes.
Despite this, many health professionals in Australia continue to use x-rays to diagnose knee osteoarthritis. And many people with osteoarthritis still expect or want them.
What did our study investigate?
Our study aimed to find out if using x-rays to diagnose knee osteoarthritis affects a person’s beliefs about osteoarthritis management, compared to a getting a clinical diagnosis without x-rays.
We recruited 617 people from across Australia and randomly assigned them to watch one of three videos. Each video showed a hypothetical consultation with a general practitioner about knee pain.
People with knee osteoarthritis can have difficulties getting down stairs. beeboys/Shutterstock One group received a clinical diagnosis of knee osteoarthritis based on age and symptoms, without being sent for an x-ray.
The other two groups had x-rays to determine their diagnosis (the doctor showed one group their x-ray images and not the other).
After watching their assigned video, participants completed a survey about their beliefs about osteoarthritis management.
What did we find?
People who received an x-ray-based diagnosis and were shown their x-ray images had a 36% higher perceived need for knee replacement surgery than those who received a clinical diagnosis (without x-ray).
They also believed exercise and physical activity could be more harmful to their joint, were more worried about their condition worsening, and were more fearful of movement.
Interestingly, people were slightly more satisfied with an x-ray-based diagnosis than a clinical diagnosis.
This may reflect the common misconception that osteoarthritis is caused by “wear and tear” and an assumption that the “damage” inside the joint needs to be seen to guide treatment.
What does this mean for people with osteoarthritis?
Our findings show why it’s important to avoid unnecessary x-rays when diagnosing knee osteoarthritis.
While changing clinical practice can be challenging, reducing unnecessary x-rays could help ease patient anxiety, prevent unnecessary concern about joint damage, and reduce demand for costly and potentially unnecessary joint replacement surgery.
It could also help reduce exposure to medical radiation and lower health-care costs.
Previous research in osteoarthritis, as well as back and shoulder pain, similarly shows that when health professionals focus on joint “wear and tear” it can make patients more anxious about their condition and concerned about damaging their joints.
If you have knee osteoarthritis, know that routine x-rays aren’t needed for diagnosis or to determine the best treatment for you. Getting an x-ray can make you more concerned and more open to surgery. But there are a range of non-surgical options that could reduce pain, improve mobility and are less invasive.
Belinda Lawford, Senior Research Fellow in Physiotherapy, The University of Melbourne; Kim Bennell, Professor of Physiotherapy, The University of Melbourne; Rana Hinman, Professor in Physiotherapy, The University of Melbourne, and Travis Haber, Postdoctoral Research Fellow in Physiotherapy, The University of Melbourne
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: