Rushing Woman’s Syndrome – by Dr. Libby Weaver
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s well-known that very many women suffer from “the triple burden” of professional work, housework, and childcare. And it’s not even necessarily that we resent any of those things or feel like they’re a burden; we (hopefully) love our professions, homes, children. But, here’s the thing: no amount of love will add extra hours to the day!
On the psychological level, a lot is about making more conscious decisions and fewer automatic reactions. For example, everyone wants everything from us right now, if not by yesterday, but when do they need it? And, is it even our responsibility? Not everything is, and many of us take on more than we should in our effort to be “enough”.
On the physical level, she covers hormones, including the menstrual/menopausal and the metabolic, as well as liver health, digestive issues, and sleep.
The style is direct and friendly, making frequent references to science but not getting deep into it.
It’s worth noting that while she acknowledges other demographics exist, she’s writing mainly for an audience of otherwise healthy straight white women with children and at least moderate financial resources, so if you fall outside of those things, there may be things that society will penalize you for and expect more from you in return for less, so that is a limitation of the book.
Bottom line: if the above describes you, you will probably get value out of this book.
Click here to check out Rushing Woman’s Syndrome, and take care of yourself too!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Walking can prevent low back pain, a new study shows
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Do you suffer from low back pain that recurs regularly? If you do, you’re not alone. Roughly 70% of people who recover from an episode of low back pain will experience a new episode in the following year.
The recurrent nature of low back pain is a major contributor to the enormous burden low back pain places on individuals and the health-care system.
In our new study, published today in The Lancet, we found that a program combining walking and education can effectively reduce the recurrence of low back pain.
PeopleImages.com – Yuri A/Shutterstock The WalkBack trial
We randomly assigned 701 adults who had recently recovered from an episode of low back pain to receive an individualised walking program and education (intervention), or to a no treatment group (control).
Participants in the intervention group were guided by physiotherapists across six sessions, over a six-month period. In the first, third and fifth sessions, the physiotherapist helped each participant to develop a personalised and progressive walking program that was realistic and tailored to their specific needs and preferences.
The remaining sessions were short check-ins (typically less than 15 minutes) to monitor progress and troubleshoot any potential barriers to engagement with the walking program. Due to the COVID pandemic, most participants received the entire intervention via telehealth, using video consultations and phone calls.
Low back pain can be debilitating. Karolina Kaboompics/Pexels The program was designed to be manageable, with a target of five walks per week of roughly 30 minutes daily by the end of the six-month program. Participants were also encouraged to continue walking independently after the program.
Importantly, the walking program was combined with education provided by the physiotherapists during the six sessions. This education aimed to give people a better understanding of pain, reduce fear associated with exercise and movement, and give people the confidence to self-manage any minor recurrences if they occurred.
People in the control group received no preventative treatment or education. This reflects what typically occurs after people recover from an episode of low back pain and are discharged from care.
What the results showed
We monitored the participants monthly from the time they were enrolled in the study, for up to three years, to collect information about any new recurrences of low back pain they may have experienced. We also asked participants to report on any costs related to their back pain, including time off work and the use of health-care services.
The intervention reduced the risk of a recurrence of low back pain that limited daily activity by 28%, while the recurrence of low back pain leading participants to seek care from a health professional decreased by 43%.
Participants who received the intervention had a longer average period before they had a recurrence, with a median of 208 days pain-free, compared to 112 days in the control group.
In our study, regular walking appeared to help with low back pain. PeopleImages.com – Yuri A/Shutterstock Overall, we also found this intervention to be cost-effective. The biggest savings came from less work absenteeism and less health service use (such as physiotherapy and massage) among the intervention group.
This trial, like all studies, had some limitations to consider. Although we tried to recruit a wide sample, we found that most participants were female, aged between 43 and 66, and were generally well educated. This may limit the extent to which we can generalise our findings.
Also, in this trial, we used physiotherapists who were up-skilled in health coaching. So we don’t know whether the intervention would achieve the same impact if it were to be delivered by other clinicians.
Walking has multiple benefits
We’ve all heard the saying that “prevention is better than a cure” – and it’s true. But this approach has been largely neglected when it comes to low back pain. Almost all previous studies have focused on treating episodes of pain, not preventing future back pain.
A limited number of small studies have shown that exercise and education can help prevent low back pain. However, most of these studies focused on exercises that are not accessible to everyone due to factors such as high cost, complexity, and the need for supervision from health-care or fitness professionals.
On the other hand, walking is a free, accessible way to exercise, including for people in rural and remote areas with limited access to health care.
Walking has a variety of advantages. Cast Of Thousands/Shutterstock Walking also delivers many other health benefits, including better heart health, improved mood and sleep quality, and reduced risk of several chronic diseases.
While walking is not everyone’s favourite form of exercise, the intervention was well-received by most people in our study. Participants reported that the additional general health benefits contributed to their ongoing motivation to continue the walking program independently.
Why is walking helpful for low back pain?
We don’t know exactly why walking is effective for preventing back pain, but possible reasons could include the combination of gentle movements, loading and strengthening of the spinal structures and muscles. It also could be related to relaxation and stress relief, and the release of “feel-good” endorphins, which block pain signals between your body and brain – essentially turning down the dial on pain.
It’s possible that other accessible and low-cost forms of exercise, such as swimming, may also be effective in preventing back pain, but surprisingly, no studies have investigated this.
Preventing low back pain is not easy. But these findings give us hope that we are getting closer to a solution, one step at a time.
Tash Pocovi, Postdoctoral research fellow, Department of Health Sciences, Macquarie University; Christine Lin, Professor, Institute for Musculoskeletal Health, University of Sydney; Mark Hancock, Professor of Physiotherapy, Macquarie University; Petra Graham, Associate Professor, School of Mathematical and Physical Sciences, Macquarie University, and Simon French, Professor of Musculoskeletal Disorders, Macquarie University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Healthy Habits for Managing & Reversing Prediabetes – by Dr. Marie Feldman
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The book doesn’t assume prior knowledge, and does explain the science of diabetes, prediabetes, the terms and the symptoms, what’s going on inside, etc—before getting onto the main meat of the book, the tips.
The promised 100 tips are varied in their application; they range from diet and exercise, to matters of sleep, stress, and even love.
There are bonus tips too! For example, an appendix covers “tips for healthier eating out” (i.e. in restaurants etc) and a grocery list to ensure your pantry is good for defending you against prediabetes.
The writing style is very accessible pop-science; this isn’t like reading some dry academic paper—though it does cite its sources for claims, which we always love to see.
Bottom line: if you’d like to proof yourself against prediabetes, and are looking for “small things that add up” habits to get into to achieve that, this book is an excellent first choice.
Share This Post
-
We looked at over 166,000 psychiatric records. Over half showed people were admitted against their will
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Picture two people, both suffering from a serious mental illness requiring hospital admission. One was born in Australia, the other in Asia.
Hopefully, both could be treated on a voluntary basis, taking into account their individual needs, preferences and capacity to consent. If not, you might imagine they should be equally likely to receive treatment against their will (known colloquially as being “sectioned” or “scheduled”).
However, our research published in British Journal of Psychiatry Open suggests this is not the case.
In the largest study globally of its kind, we found Australians are more likely to be treated in hospital for their acute mental illness against their will if they are born overseas, speak a language other than English or are unemployed.
What we did and what we found
We examined more than 166,000 episodes of voluntary and involuntary psychiatric care in New South Wales public hospitals between 2016 and 2021. Most admissions (54%) included at least one day of involuntary care.
Being brought to hospital via legal means, such as by police or via a court order, was strongly linked to involuntary treatment.
While our study does not show why this is the case, it may be due to mental health laws. In NSW, which has similar laws to most jurisdictions in Australia, doctors may treat a person on an involuntary basis if they present with certain symptoms indicating serious mental illness (such as hallucinations and delusions) which cause them to require protection from serious harm, and there is no other less-restrictive care available. Someone who has been brought to hospital by police or the courts may be more likely to meet the legal requirement of requiring protection from serious harm.
The likelihood of involuntary care was also linked to someone’s diagnosis. A person with psychosis or organic brain diseases, such as dementia and delirium, were about four times as likely to be admitted involuntarily compared to someone with anxiety or adjustment disorders (conditions involving a severe reaction to stressors).
However, our data suggest non-clinical factors contribute to the decision to impose involuntary care.
Compared with people born in Australia, we found people born in Asia were 42% more likely to be treated involuntarily.
People born in Africa or the Middle East were 32% more likely to be treated this way.
Overall, people who spoke a language other than English were 11% more likely to receive involuntary treatment compared to those who spoke English as their first language.
Some international researchers have suggested higher rates of involuntary treatment seen in people born overseas might be due to higher rates of psychotic illness. But our research found a link between higher rates of involuntary care in people born overseas or who don’t speak English regardless of their diagnosis.
We don’t know why this is happening. It is likely to reflect a complex interplay of factors about both the people receiving treatment and the way services are provided to them.
People less likely to be treated involuntarily included those who hold private health insurance, and those referred through a community health centre or outpatients unit.
Our findings are in line with international studies. These show higher rates of involuntary treatment among people from Black and ethnic minority groups, and people living in areas of higher socioeconomic disadvantage.
A last resort? Or should we ban it?
Both the NSW and Australian mental health commissions have called involuntary psychiatric care an avoidable harm that should only be used as a last resort.
Despite this, one study found Australia’s rate of involuntary admissions has increased by 3.4% per year and it has one of the highest rates of involuntary admissions in the world.
Involuntary psychiatric treatment is also under increasing scrutiny globally.
When Australia signed up to the UN Convention on the Rights of Persons with Disabilities, it added a declaration noting it would allow for involuntary treatment of people with mental illness where such treatments are “necessary, as a last resort and subject to safeguards”.
However, the UN has rejected this, saying it is a fundamental human right “to be free from involuntary detention in a mental health facility and not to be forced to undergo mental health treatment”.
Others question if involuntary treatment could ever be removed entirely.
Where to from here?
Our research not only highlights concerns regarding how involuntary psychiatric treatment is implemented, it’s a first step towards decreasing its use. Without understanding how and when it is used it will be difficult to create effective interventions to reduce it.
But Australia is still a long way from significantly reducing involuntary treatment.
We need to provide more care options outside hospital, ones accessible to all Australians, including those born overseas, who don’t speak English, or who come from disadvantaged communities. This includes intervening early enough that people are supported to not become so unwell they end up being referred for treatment via police or the criminal justice system.
More broadly, we need to do more to reduce stigma surrounding mental illness and to ensure poverty and discrimination are tackled to help prevent more people becoming unwell in the first place.
Our study also shows we need to do more to respect the autonomy of someone with serious mental illness to choose if they are treated. That’s whether they are in NSW or other jurisdictions.
And legal reform is required to ensure more states and territories more fully reflect the principal that people who have the capacity to make such decisions should have the right to decline mental health treatment in the same way they would any other health care.
If this article has raised issues for you, or if you’re concerned about someone you know, call Lifeline on 13 11 14.
Amy Corderoy, Medical doctor and PhD candidate studying involuntary psychiatric treatment, School of Psychiatry, UNSW Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
The Coffee-Cortisol Connection, And Two Ways To Tweak It For Health
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Health opinions on coffee vary from “it’s an invigorating, healthful drink” to “it will leave you a shaking frazzled wreck”. So, what’s the truth and can we enjoy it healthily? Dr. Alan Mandell weighs in:
Enjoy it, but watch out!
Dr. Mandell is speaking only for caffeinated coffee in this video, and to this end, he’s conflating the health effects of coffee and caffeine. A statistically reasonable imprecision, since most people drink coffee with its natural caffeine in, but we’ll make some adjustment to his comments below, to disambiguate which statements are true for coffee generally, and which are true for caffeine:
- Drinking
coffeecaffeine first thing in the morning may not be ideal due to dehydration from overnight water loss. Coffeecaffeine is a diuretic, which means an increase in urination, thus further dehydrating the body.- Coffee contains great antioxidants, which are of course beneficial for the health in general.
- Cortisol, the body’s stress hormone, is generally at its peak in the morning. This is, in and of itself, good and correct—it’s how we wake up.
Coffeecaffeine consumption raises cortisol levels even more, leading to increased alertness and physical readiness, but it is possible to have too much of a good thing, and in this case, problems can arise because…- Elevated cortisol from early
coffeecaffeine drinking can build tolerance, leading to the need for morecoffeecaffeine over time. - It’s better, therefore, to defer drinking
coffeecaffeine until later in the morning when cortisol levels naturally drop. - All of this means that drinking
coffeecaffeine first thing can disrupt the neuroendocrine system, leading to fatigue, depression, and general woe. - Hydrate first thing in the morning before consuming
coffeecaffeine to keep the body balanced and healthy.
What you can see from this is that coffee and caffeine are not, in fact, interchangeable words, but the basic message is clear and correct: while a little spike of cortisol in the morning is good, natural, and even necessary, a big spike is none of those things, and caffeine can cause a big spike, and since for most people caffeine is easy to build tolerance to, there will indeed consistently be a need for more, worsening the problem.
In terms of hydration, it’s good to have water (or better yet, herbal tea) on one’s nightstand to drink when one wakes up.
If coffee is an important morning ritual for you, consider finding a good decaffeinated version for at least your first cup (this writer is partial to Lavazza’s “Dek Intenso”—which is not the same as their main decaf line, by the way, so do hold out for the “Dek Intenso” if you want to try my recommendation).
Decaffeinated coffee is hydrating and will not cause a cortisol spike (unless for some reason you find coffee as a concept very stressful in which case, yes, the stressor will cause a stress response).
Anyway, for more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
- Drinking
-
Bird flu has been detected in a pig in the US. Why does that matter?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The United States Department of Agriculture last week reported that a pig on a backyard farm in Oregon was infected with bird flu.
As the bird flu situation has evolved, we’ve heard about the A/H5N1 strain of the virus infecting a range of animals, including a variety of birds, wild animals and dairy cattle.
Fortunately, we haven’t seen any sustained spread between humans at this stage. But the detection of the virus in a pig marks a worrying development in the trajectory of this virus.
David MG/Shutterstock How did we get here?
The most concerning type of bird flu currently circulating is clade 2.3.4.4b of A/H5N1, a strain of influenza A.
Since 2020, A/H5N1 2.3.4.4b has spread to a vast range of birds, wild animals and farm animals that have never been infected with bird flu before.
While Europe is a hotspot for A/H5N1, attention is currently focused on the US. Dairy cattle were infected for the first time in 2024, with more than 400 herds affected across at least 14 US states.
Bird flu has enormous impacts on farming and commercial food production, because infected poultry flocks have to be culled, and infected cows can result in contaminated diary products. That said, pasteurisation should make milk safe to drink.
While farmers have suffered major losses due to H5N1 bird flu, it also has the potential to mutate to cause a human pandemic.
Birds and humans have different types of receptors in their respiratory tract that flu viruses attach to, like a lock (receptors) and key (virus). The attachment of the virus allows it to invade a cell and the body and cause illness. Avian flu viruses are adapted to birds, and spread easily among birds, but not in humans.
So far, human cases have mainly occurred in people who have been in close contact with infected farm animals or birds. In the US, most have been farm workers.
The concern is that the virus will mutate and adapt to humans. One of the key steps for this to happen would be a shift in the virus’ affinity from the bird receptors to those found in the human respiratory tract. In other words, if the virus’ “key” mutated to better fit with the human “lock”.
A recent study of a sample of A/H5N1 2.3.4.4b from an infected human had worrying findings, identifying mutations in the virus with the potential to increase transmission between human hosts.
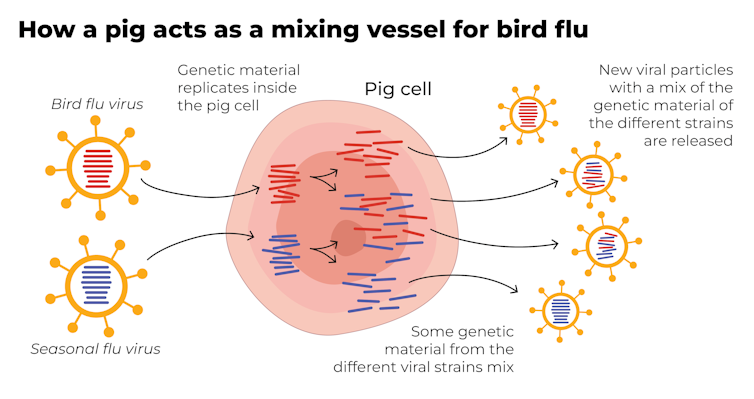
Why are pigs a problem?
A human pandemic strain of influenza can arise in several ways. One involves close contact between humans and animals infected with their own specific flu viruses, creating opportunities for genetic mixing between avian and human viruses.
Pigs are the ideal genetic mixing vessel to generate a human pandemic influenza strain, because they have receptors in their respiratory tracts which both avian and human flu viruses can bind to.
This means pigs can be infected with a bird flu virus and a human flu virus at the same time. These viruses can exchange genetic material to mutate and become easily transmissible in humans.
The Conversation, CC BY-SA Interestingly, in the past pigs were less susceptible to A/H5N1 viruses. However, the virus has recently mutated to infect pigs more readily.
In the recent case in Oregon, A/H5N1 was detected in a pig on a non-commercial farm after an outbreak occurred among the poultry housed on the same farm. This strain of A/H5N1 was from wild birds, not the one that is widespread in US dairy cows.
The infection of a pig is a warning. If the virus enters commercial piggeries, it would create a far greater level of risk of a pandemic, especially as the US goes into winter, when human seasonal flu starts to rise.
How can we mitigate the risk?
Surveillance is key to early detection of a possible pandemic. This includes comprehensive testing and reporting of infections in birds and animals, alongside financial compensation and support measures for farmers to encourage timely reporting.
Strengthening global influenza surveillance is crucial, as unusual spikes in pneumonia and severe respiratory illnesses could signal a human pandemic. Our EPIWATCH system looks for early warnings of such activity, which can speed up vaccine development.
If a cluster of human cases occurs, and influenza A is detected, further testing (called subtyping) is essential to ascertain whether it’s a seasonal strain, an avian strain from a spillover event, or a novel pandemic strain.
Early identification can prevent a pandemic. Any delay in identifying an emerging pandemic strain enables the virus to spread widely across international borders.
Australia’s first human case of A/H5N1 occurred in a child who acquired the infection while travelling in India, and was hospitalised with illness in March 2024. At the time, testing revealed Influenza A (which could be seasonal flu or avian flu), but subtyping to identify A/H5N1 was delayed.
This kind of delay can be costly if a human-transmissible A/H5N1 arises and is assumed to be seasonal flu because the test is positive for influenza A. Only about 5% of tests positive for influenza A are subtyped further in Australia and most countries.
In light of the current situation, there should be a low threshold for subtyping influenza A strains in humans. Rapid tests which can distinguish between seasonal and H5 influenza A are emerging, and should form part of governments’ pandemic preparedness.
A higher risk than ever before
The US Centers for Disease Control and Prevention states that the current risk posed by H5N1 to the general public remains low.
But with H5N1 now able to infect pigs, and showing worrying mutations for human adaptation, the level of risk has increased. Given the virus is so widespread in animals and birds, the statistical probability of a pandemic arising is higher than ever before.
The good news is, we are better prepared for an influenza pandemic than other pandemics, because vaccines can be made in the same way as seasonal flu vaccines. As soon as the genome of a pandemic influenza virus is known, the vaccines can be updated to match it.
Partially matched vaccines are already available, and some countries such as Finland are vaccinating high-risk farm workers.
C Raina MacIntyre, Professor of Global Biosecurity, NHMRC L3 Research Fellow, Head, Biosecurity Program, Kirby Institute, UNSW Sydney and Haley Stone, Research Associate, Biosecurity Program, Kirby Institute & CRUISE lab, Computer Science and Engineering, UNSW Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
A new government inquiry will examine women’s pain and treatment. How and why is it different?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Victorian government has announced an inquiry into women’s pain. Given women are disproportionately affected by pain, such a thorough investigation is long overdue.
The inquiry, the first of its kind in Australia and the first we’re aware of internationally, is expected to take a year. It aims to improve care and services for Victorian girls and women experiencing pain in the future.
The gender pain gap
Globally, more women report chronic pain than men do. A survey of over 1,750 Victorian women found 40% are living with chronic pain.
Approximately half of chronic pain conditions have a higher prevalence in women compared to men, including low back pain and osteoarthritis. And female-specific pain conditions, such as endometriosis, are much more common than male-specific pain conditions such as chronic prostatitis/chronic pelvic pain syndrome.
These statistics are seen across the lifespan, with higher rates of chronic pain being reported in females as young as two years old. This discrepancy increases with age, with 28% of Australian women aged over 85 experiencing chronic pain compared to 18% of men.
It feels worse
Women also experience pain differently to men. There is some evidence to suggest that when diagnosed with the same condition, women are more likely to report higher pain scores than men.
Similarly, there is some evidence to suggest women are also more likely to report higher pain scores during experimental trials where the same painful pressure stimulus is applied to both women and men.
Pain is also more burdensome for women. Depression is twice as prevalent in women with chronic pain than men with chronic pain. Women are also more likely to report more health care use and be hospitalised due to their pain than men.
Women seem to feel pain more acutely and often feel ignored by doctors.
ShutterstockMedical misogyny
Women in pain are viewed and treated differently to men. Women are more likely to be told their pain is psychological and dismissed as not being real or “all in their head”.
Hollywood actor Selma Blair recently shared her experience of having her symptoms repeatedly dismissed by doctors and put down to “menstrual issues”, before being diagnosed with multiple sclerosis in 2018.
It’s an experience familiar to many women in Australia, where medical misogyny still runs deep. Our research has repeatedly shown Australian women with pelvic pain are similarly dismissed, leading to lengthy diagnostic delays and serious impacts on their quality of life.
Misogyny exists in research too
Historically, misogyny has also run deep in medical research, including pain research. Women have been viewed as smaller bodied men with different reproductive functions. As a result, most pre-clinical pain research has used male rodents as the default research subject. Some researchers say the menstrual cycle in female rodents adds additional variability and therefore uncertainty to experiments. And while variability due to the menstrual cycle may be true, it may be no greater than male-specific sources of variability (such as within-cage aggression and dominance) that can also influence research findings.
The exclusion of female subjects in pre-clinical studies has hindered our understanding of sex differences in pain and of response to treatment. Only recently have we begun to understand various genetic, neurochemical, and neuroimmune factors contribute to sex differences in pain prevalence and sensitivity. And sex differences exist in pain processing itself. For instance, in the spinal cord, male and female rodents process potentially painful stimuli through entirely different immune cells.
These differences have relevance for how pain should be treated in women, yet many of the existing pharmacological treatments for pain, including opioids, are largely or solely based upon research completed on male rodents.
When women seek care, their pain is also treated differently. Studies show women receive less pain medication after surgery compared to men. In fact, one study found while men were prescribed opioids after joint surgery, women were more likely to be prescribed antidepressants. In another study, women were more likely to receive sedatives for pain relief following surgery, while men were more likely to receive pain medication.
So, women are disproportionately affected by pain in terms of how common it is and sensitivity, but also in how their pain is viewed, treated, and even researched. Women continue to be excluded, dismissed, and receive sub-optimal care, and the recently announced inquiry aims to improve this.
What will the inquiry involve?
Consumers, health-care professionals and health-care organisations will be invited to share their experiences of treatment services for women’s pain in Victoria as part of the year-long inquiry. These experiences will be used to describe the current service delivery system available to Victorian women with pain, and to plan more appropriate services to be delivered in the future.
Inquiry submissions are now open until March 12 2024. If you are a Victorian woman living with pain, or provide care to Victorian women with pain, we encourage you to submit.
The state has an excellent track record of improving women’s health in many areas, including heart, sexual, and reproductive health, but clearly, we have a way to go with women’s pain. We wait with bated breath to see the results of this much-needed investigation, and encourage other states and territories to take note of the findings.
Jane Chalmers, Senior Lecturer in Pain Sciences, University of South Australia and Amelia Mardon, PhD Candidate, University of South Australia
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: