Is fluoride really linked to lower IQ, as a recent study suggested? Here’s why you shouldn’t worry
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Fluoride is a common natural element found in water, soil, rocks and food. For the past several decades, fluoride has also been a cornerstone of dentistry and public health, owing to its ability to protect against tooth decay.
Water fluoridation is a population-based program where a precise, small amount of fluoride is added to public drinking water systems. Water fluoridation began in Australia in the 1950s. Today more than 90% of Australia’s population has access to fluoridated tap water.
But a recently published review found higher fluoride exposure is linked to lower intelligence quotient (IQ) in children. So how can we interpret the results?
Much of the data analysed in this review is poor quality. Overall, the findings don’t give us reason to be concerned about the fluoride levels in our water supplies.

Not a new controversy
Tooth decay (also known as caries or cavities) can have negative effects on dental health, overall health and quality of life. Fluoride strengthens our teeth, making them more resistant to decay. There is scientific consensus water fluoridation is a safe, effective and equitable way to improve oral health.
Nonetheless, water fluoridation has historically been somewhat controversial.
A potential link between fluoride and IQ (and cognitive function more broadly) has been a contentious topic for more than a decade. This started with reports from studies in China and India.
But it’s important to note these studies were limited by poor methodology, and water in these countries had high levels of natural fluoride when the studies were conducted – many times higher than the levels recommended for water fluoridation programs. Also, the studies did not control for other contaminants in the water supply.
Recent reviews focusing on the level of fluoride used in water fluoridation have concluded fluoride is not linked to lower IQ.
Despite this, some have continued to raise concerns. The United States National Toxicology Program conducted a review of the potential link. However, this review did not pass the quality assessment by the US National Academies of Sciences, Engineering and Medicine due to significant limitations in the conduct of the review.
The authors followed through with their study and published it as an independent publication in the journal JAMA Paediatrics last week. This is the study which has been generating media attention in recent days.
What the study did
This study was a systematic review and meta-analysis, where the researchers evaluated 74 studies from different parts of the world.
A total of 52 studies were rated as having a high risk of bias, and 64 were cross-sectional studies, which often can’t provide evidence of causal relationship.
Most of the studies were conducted in developing countries, such as China (45), India (12), Iran (4), Mexico (4) and Pakistan (2). Only a few studies were conducted in developed countries with established public water systems, where regular monitoring and treatment of drinking water ensures it’s free from contaminants.
The vast majority of studies were conducted in populations with high to very high levels of natural fluoride and without water fluoridation programs, where fluoride levels are controlled within recommended levels.
The study concluded there was an inverse association between fluoride levels and IQ in children. This means those children who had a higher intake of fluoride had lower IQ scores than their counterparts.

Limitations to consider
While this review combined many studies, there are several limitations that cast serious doubt over its conclusion. Scientists immediately raised concerns about the quality of the review, including in a linked editorial published in JAMA.
The low quality of the majority of included studies is a major concern, rendering the quality of the review equally low. Importantly, most studies were not relevant to the recommended levels of fluoride in water fluoridation programs.
Several included studies from countries with controlled public water systems (Canada, New Zealand, Taiwan) showed no negative effects. Other recent studies from comparable populations (such as Spain and Denmark) also have not shown any negative effect of fluoride on IQ, but they were not included in the meta-analysis.
For context, the review found there was no significant association with IQ when fluoride was measured at less than 1.5mg per litre in water. In Australia, the recommended levels of fluoride in public water supplies range from 0.6 to 1.1 mg/L.
Also, the primary outcome, IQ score, is difficult to collect. Most included studies varied widely on the methods used to collect IQ data and did not specify their focus on ensuring reliable and consistent IQ data. Though this is a challenge in most research on this topic, the significant variations between studies in this review raise further doubts about the combined results.
No cause for alarm
Although no Australian studies were included in the review, Australia has its own studies investigating a potential link between fluoride exposure in early childhood and child development.
I’ve been involved in population-based longitudinal studies investigating a link between fluoride and child behavioural development and executive functioning and between fluoride and IQ. The IQ data in the second study were collected by qualified, trained psychologists – and calibrated against a senior psychologist – to ensure quality and consistency. Both studies have provided strong evidence fluoride exposure in Australia does not negatively impact child development.
This new review is not a reason to be concerned about fluoride levels in Australia and other developed countries with water fluoridation programs. Fluoride remains important in maintaining the public’s dental health, particularly that of more vulnerable groups.
That said, high and uncontrolled levels of fluoride in water supplies in less developed countries warrant attention. There are programs underway in a range of countries to reduce natural fluoride to the recommended level.
Loc Do, Professor of Dental Public Health, The University of Queensland
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Slow-Cooker Moroccan Tagine
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Tagine (طاجين) (tā-jīn) is a traditional dish named after, well, the traditional dish that it’s cooked in. Here’s an example tagine pot on Amazon. It’s a very nifty bit of kit, and while it’s often used for cooking over charcoal, one of its features is that if you have a hot sunny day, you can just leave it out in the sun and it will cook the contents nicely. Today though, we’re going to assume you don’t have one of these, and are going to give instructions for cooking a tagine-style dish with a slow cooker, which we’re going to assume you do have.
You will need
- 2 large red onions, finely chopped
- 2 large red peppers, cut into 1″ chunks
- 2 large zucchini, cut into ½” chunks
- 1 large eggplant, cut into ½” chunks
- 3 cups tomato passata
- 2 cups cooked chickpeas
- 16 pitted Medjool dates, chopped
- ½ bulb garlic, finely chopped
- 1 tbsp ras el-hanout
- A little extra virgin olive oil
Method
(we suggest you read everything at least once before doing anything)
1) Let your slow cooker heat up while you chop the things that need chopping
2) Add a splash of olive oil to the slow cooker; ensure the base is coated and there’s a little oil spare in there too; a thin coat to the base plus a couple of tbsp should do it nicely.
3) Add the onions and garlic, and leave for an hour.
4) Add the passata, dates, ras el-hanout, stir it and leave for an hour.
5) Add the chickpeas, peppers, and eggplant; stir it and leave for an hour.
6) Add the zucchini, stir it and leave for an hour.
7) Serve—it goes great with its traditional pairing of wholegrain couscous, but if you prefer, you can use our tasty versatile rice. In broader culinary terms, serving it with any carb is fine.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Level-Up Your Fiber Intake! (Without Difficulty Or Discomfort)
- What Matters Most For Your Heart? Eat More (Of This) For Lower Blood Pressure
- Our Top 5 Spices: How Much Is Enough For Benefits?
Take care!
Share This Post
-
How To Manage Your Mood With Food (8 Ways)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It is hard to be mentally healthy for long without good diet. Food can not only affect our mood directly, but also indirectly because of how our brain works (or doesn’t, if we don’t have the right nutrients, or it is being sabotaged in some other dietary fashion).
Selecting the food for setting the mood
Mind, the mental health charity, have these advices to share (with some bonus notes of our own):
- Eat regularly: blood sugar peaks and troughs can heighten feelings of tiredness, irritability, or depression. Instead, enjoy foods that are high in energy but low in glycemic index, such as nuts, seeds, and oats—that way you’ll have plenty of energy, that lasts longer.
- Choose the right fats: omega-3 fatty acids are essential for the brain. So are omega-6 fatty acids, but it is rare to have a deficiency in omega-6, and indeed, many people have the ratio of omega-3 to omega-6 far too imbalanced in omega-6’s favor. So, focussing on getting more omega-3 fatty acids is important. Nuts and seeds are again great, as are avocados, eggs, and oily fish.
- Get a healthy amount of protein: and importantly, with a good mix of amino acids—so a variety of sources of protein is best. In particular, if you are vegan, paying attention to ensure you get a full spread of amino acids is critical, as not many plants have all the ones we need (soy does, though). The reason this is important for mood is because many of those amino acids double up as the building blocks of neurotransmitters, so they’re not entirely interchangeable.
- Stay hydrated: our bodies are famously made of mostly water, and our brain will not work well if it’s dehydrated. The human body can squeeze water out of almost anything that has water in it, but water from food (such as fruit, or soups) is best. If enjoying actual drinks, then herbal teas are excellent for hydration.
- Eat a rainbow of fruits and vegetables: these have many nutrients that are important for brain health, and the point of the colors is that most of those pigments are themselves nutrients. Additionally, the fiber content of fruits and vegetables is of topmost important for your heart, and as you’ll remember (we say it often, because it’s true): what’s good for your heart is good for your brain.
- Limit caffeine intake: for many people, excess caffeine can lead to feelings of anxiety, disrupt your sleep, and for everyone who has developed an addiction to it, it will cause withdrawal symptoms if stopped abruptly. Cutting back on caffeine, or even eliminating it, may improve your mood and sleep quality. Note, however, that if you have ADHD, then your brain’s physiological relationship with caffeine is a little different, and stimulants will be more beneficial (and less deleterious) for you than for most people. If unsure, speak with your doctor about this one.
- Support your gut health: because of the gut-brain axis (via the vagal nerve), and also because nearly all of our endogenous serotonin is made in the gut (along with other neurotransmitters/hormones), getting plenty of fiber is important, and probiotics can help too.
- Consider food intolerances: if you know you have one, then keep that in mind and tailor your diet accordingly. If you suspect you have one, seek a nutritionist’s help to find out for sure. These can affect many aspects of health, including mood, so should not be dismissed as a triviality.
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
The 6 Pillars Of Nutritional Psychiatry
Take care!
Share This Post
-
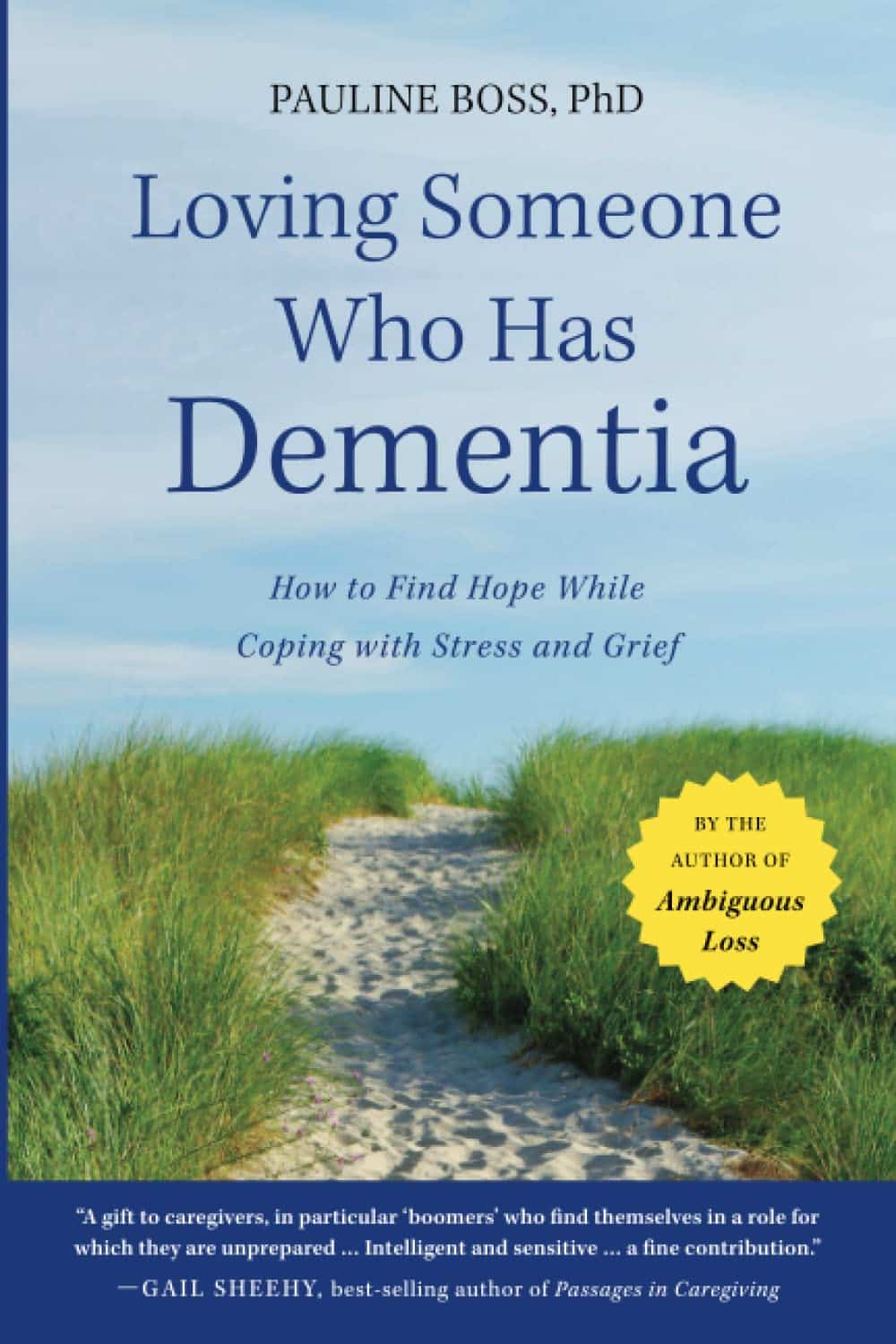
Loving Someone Who Has Dementia – by Dr. Pauline Boss
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We previously reviewed Dr. Boss’s excellent book “Loss, Trauma, and Resilience: Therapeutic Work With Ambiguous Loss”, which partially overlaps in ideas with this one. In that case, it was about grief when a loved one is “gone, but are they really?”, which can include missing persons, people killed in ways that weren’t 100% confirmed (e.g. no body to bury), and in contrast, people who are present in body but not entirely present mentally: perhaps in a coma, for example. It also includes people are for other reasons not entirely present in the way they used to be, which includes dementia. And that latter case is what this book focuses on.
In the case of dementia, we cannot, of course, simply focus on ourselves. Well, not if we care about the person with dementia, anyway. Much like with the other kinds of ambiguous loss, we cannot fully come to terms with things while on the cusp of presence and absence, and we cannot, as such, “give up” on our loved one.
What then, of hope? The author makes the case for—in absence of any kind of closure—making our peace with the situation as it is, making our peace with the uncertainty of things. And that means not only “at any moment could come a more clearly complete loss”, but also on the flipside at least a faint candle of hope, that we should not grasp with both hands (that is not how to treat a candle, literally or metaphorically), but rather, hold gently, and enjoy its gentle light.
Dr. Boss also covers more practical considerations; family rituals, celebrations, gatherings, and the idea of “the good-enough relationship”. Particularly helpfully, she gives her “seven guidelines for the journey”, which even if one decides against adopting them all, are definitely all good things to at least have considered.
The style is much more tailored to the lay reader than the other book of hers that we reviewed, which was intended more for clinicians, but useful also for those of us who have been hit by such kinds of grief. In this case, however, her intention is first and foremost for the family of a person who has dementia—there are still footnotes throughout though, for those who still want to read scientific papers that support the various ideas discussed in the book.
Bottom line: if a loved one has dementia or that seems a likely possibility for you, this book can help a lot!
Share This Post
Related Posts
-
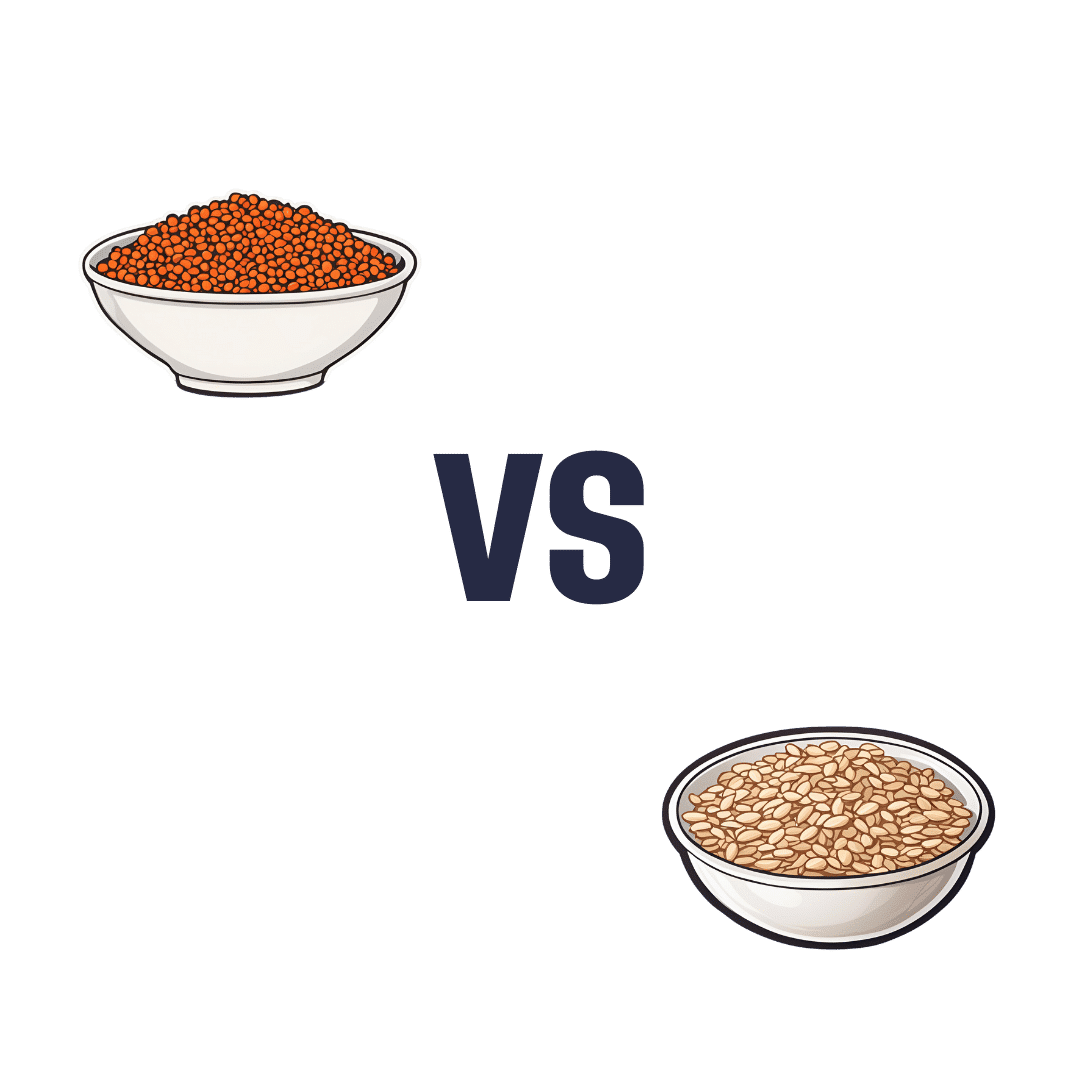
Red Lentils vs Oats – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing red lentils to oats, we picked the oats.
Why?
In terms of macros, oats have more protein, carbs, fiber, and even a little fat—mostly healthy mono- and polyunsaturated fats, thus making them the more nutritionally dense. That said, red lentils have the lower glycemic index, (low GI compared to oats’ medium GI) which offsets that, so we’ll call this category a tie.
In the category of vitamins, red lentils have more of vitamins B6, B9, and choline, while oats have more of vitamins B1, B2, and B5. Another tie!
When it comes to minerals, however, we have a tiebreaker category: red lentils have more selenium, while oats have more calcium, copper, iron, magnesium, manganese, phosphorus, potassium, and zinc. An easy win for oats this time!
So, thanks to the minerals, oats are the clear winner in total. But by all means, enjoy either or both; diversity is good!
Want to learn more?
You might like to read:
The Best Kind Of Fiber For Overall Health? ← it’s β-glucan, the kind find in oats!
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Coughing/Wheezing After Dinner?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The After-Dinner Activities You Don’t Want
A quick note first: our usual medical/legal disclaimer applies here, and we are not here to diagnose you or treat you; we are not doctors, let alone your doctors. Do see yours if you have any reason to believe there may be cause for concern.
Coughing and/or wheezing after eating is more common the younger or older someone is. Lest that seem contradictory: it’s a U-shaped bell-curve.
It can happen at any age and for any of a number of reasons, but there are patterns to the distribution:
Mostly affects younger people:
Allergies, asthma
Young people are less likely to have a body that’s fully adapted to all foods yet, and asthma can be triggered by certain foods (for example sulfites, a common preservative additive):
Adverse reactions to the sulphite additives
Foods/drinks that commonly contain sulfites include soft drinks, wines and beers, and dried fruit
As for the allergies side of things, you probably know the usual list of allergens to watch out for, e.g: dairy, fish, crustaceans, eggs, soy, wheat, nuts.
However, that’s far from an exhaustive list, so it’s good to see an allergist if you suspect it may be an allergic reaction.
Affects young and old people equally:
Again, there’s a dip in the middle where this doesn’t tend to affect younger adults so much, but for young and old people:
Dysphagia (difficulty swallowing)
For children, this can be a case of not having fully got used to eating yet if very small, and when growing, can be a case of “this body is constantly changing and that makes things difficult”.
For older people, this can can come from a variety of reasons, but common culprits include neurological disorders (including stroke and/or dementia), or a change in saliva quality and quantity—a side-effect of many medications:
Hyposalivation in Elderly Patients
(particularly useful in the article above is the table of drugs that are associated with this problem, and the various ways they may affect it)
Managing this may be different depending on what is causing your dysphagia (as it could be anything from antidepressants to cancer), so this is definitely one to see your doctor about. For some pointers, though:
NHS Inform | Dysphagia (swallowing problems)
Affects older people more:
Gastroesophagal reflux disease (GERD)
This is a kind of acid reflux, but chronic, and often with a slightly different set of symptoms.
GERD has no known cure once established, but its symptoms can be managed (or avoided in the first place) by:
- Healthy eating (Mediterranean diet is, as usual, great)
- Weight loss (if and only if obese)
- Avoiding trigger foods
- Eating smaller meals
- Practicing mindful eating
- Staying upright for 3–4 hours after eating
And of course, don’t smoke, and ideally don’t drink alcohol.
You can read more about this (and the different ways it can go from there), here:
NICE | Gastro-oesophageal reflux disease
Note: this above page refers to it as “GORD”, because of the British English spelling of “oesophagus” rather than “esophagus”. It’s the exact same organ and condition, just a different spelling.
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How to Stop Negative Thinking – by Daniel Paul
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Just think positive thoughts” is all well and good, but it doesn’t get much mileage in the real world, does it?
What Daniel Paul offers is a lot better than that. Taking a CBT approach, he recommends tips and tricks, gives explanations and exercises, and in short, puts tools in the reader’s toolbox.
But it doesn’t stop at just stopping negative thinking. Rather, it takes a holistic approach to also improve your general life…
- Bookending your day with a good start and finish
- Scheduling a time for any negative thinking that does need to occur (again with the useful realism!)
- Inviting the reader to take on small challenges, of the kind that’ll have knock-on effects that add and multiply and compound as we go
The format is very easy-reading, and we love that there are clear section headings and chapter summaries, too.
Bottom line: definitely a book with the potential to improve your life from day one, and that’ll keep you coming back to it as a cheatsheet and references source.
Get your copy of “How to Stop Negative Thinking” from Amazon today!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: