How Your Brain Chooses What To Remember
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
During the day, your brain is simply too busy to encode memories without interfering with normal processing. At night, however…
The filing system
The brain decides which memories to keep based on significance, using sharp brain wave ripples as an internal bookmarking system. Everyday memories fade, while important events are tagged in this manner for consolidation during sleep.
How does it do this? It starts in the hippocampus, which records experiences during wakefulness and replays them repeatedly at high speed during sleep, preparing them for transfer to the neocortex.
How do we know? Uniform Manifold Approximation & Projection (UMAP) for dimension reduction is a tool that condenses 400-dimensional neural activity data into 3D for visualization. Mice navigating a maze showed hippocampal activity encoding location and learning progression; it also showed neural patterns reflecting maze layout and task mastery.
What this means in practical terms: you need to get good sleep if you don’t want to lose your memories!
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
How To Boost Your Memory Immediately (Without Supplements)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Cupping: How It Works (And How It Doesn’t)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Good Health By The Cup?
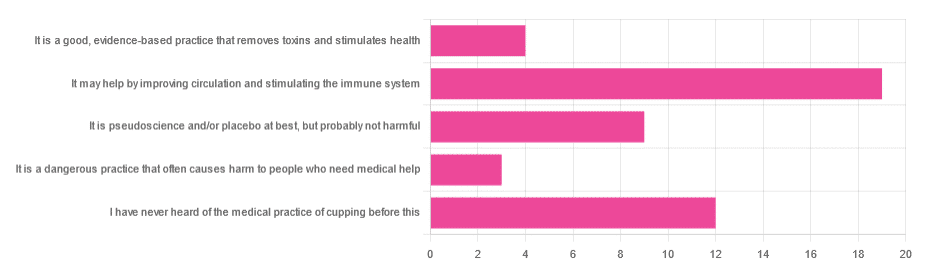
In Tuesday’s newsletter, we asked you for your opinion of cupping (the medical practice), and got the above-depicted, below-described, set of responses:
- About 40% said “It may help by improving circulation and stimulating the immune system”
- About 26% said “I have never heard of the medical practice of cupping before this”
- About 19% said “It is pseudoscience and/or placebo at best, but probably not harmful
- About 9% said “It is a good, evidence-based practice that removes toxins and stimulates health”
- About 6% said “It is a dangerous practice that often causes harm to people who need medical help”
So what does the science say?
First, a quick note for those unfamiliar with cupping: it is the practice of placing a warmed cup on the skin (open side of the cup against the skin). As the warm air inside cools, it reduces the interior air pressure, which means the cup is now (quite literally) a suction cup. This pulls the skin up into the cup a little. The end result is visually, and physiologically, the same process as what happens if someone places the nozzle of a vacuum cleaner against their skin. For that matter, there are alternative versions that simply use a pump-based suction system, instead of heated cups—but the heated cups are most traditional and seem to be most popular. See also:
National Center for Complementary and Integrative Health | Cupping
It is a dangerous practice that often causes harm to people who need medical help: True or False?
False, for any practical purposes.
- Directly, it can (and usually does) cause minor superficial harm, much like many medical treatments, wherein the benefits are considered to outweigh the harm, justifying the treatment. In the case of cupping, the minor harm is usually a little bruising, but there are other risks; see the link we gave just above.
- Indirectly, it could cause harm by emboldening a person to neglect a more impactful treatment for their ailment.
But, there’s nothing for cupping akin to the “the most common cause of death is when someone gets a vertebral artery fatally severed” of chiropractic, for example.
It is a good, evidence-based practice that removes toxins and stimulates health: True or False?
True and False in different parts. This one’s on us; we included four claims in one short line. But let’s look at them individually:
- Is it good? Well, those who like it, like it. It legitimately has some mild health benefits, and its potential for harm is quite small. We’d call this a modest good, but good nonetheless.
- Is it evidence-based? Somewhat, albeit weakly; there are some papers supporting its modest health claims, although the research is mostly only published in journals of alternative medicine, and any we found were in journals that have been described by scientists as pseudoscientific.
- Does it remove toxins? Not directly, at least. There is also a version that involves making a small hole in the skin before applying the cup, the better to draw out the toxins (called “wet cupping”). This might seem a little medieval, but this is because it is from early medieval times (wet cupping’s first recorded use being in the early 7th century). However, the body’s response to being poked, pierced, sucked, etc is to produce antibodies, and they will do their best to remove toxins. So, indirectly, there’s an argument.
- Does it stimulate health? Yes! We’ll come to that shortly. But first…
It is pseudoscience and/or placebo at best, but probably not harmful: True or False?
True in that its traditionally-proposed mechanism of action is a pseudoscience and placebo almost certainly plays a strong part, and also in that it’s generally not harmful.
On it being a pseudoscience: we’ve talked about this before, but it bears repeating; just because something’s proposed mechanism of action is pseudoscience, doesn’t necessarily mean it doesn’t work by some other mechanism of action. If you tell a small child that “eating the rainbow” will improve their health, and they believe this is some sort of magical rainbow power imbuing them with health, then the mechanism of action that they believe in is a pseudoscience, but eating a variety of colorful fruit and vegetables will still be healthy.
In the case of cupping, its proposed mechanism of action has to do withbalancing qi, yin and yang, etc (for which scientific evidence does not exist), in combination with acupuncture lore (for which some limited weak scientific evidence exists). On balancing qi, yin and yang etc, this is a lot like Europe’s historically popular humorism, which was based on the idea of balancing the four humors (blood, yellow bile, black bile, phlegm). Needless to say, humorism was not only a pseudoscience, but also eventually actively disproved with the advent of germ theory and modern medicine. Cupping therapy is not more scientifically based than humorism.
On the placebo side of things, there probably is a little more to it than that; much like with acupuncture, a lot of it may be a combination of placebo and using counter-irritation, a nerve-tricking method to use pain to reduce pain (much like pressing with one’s nail next to an insect bite).
Here’s one of the few studies we found that’s in what looks, at a glance, to be a reputable journal:
Cupping therapy and chronic back pain: systematic review and meta-analysis
It may help by improving circulation and stimulating the immune system: True or False?
True! It will improve local circulation by forcing blood into the area, and stimulate the immune system by giving it a perceived threat to fight.
Again, this can be achieved by many other means; acupuncture (or just “dry needling”, which is similar but without the traditional lore), a cold shower, and/or exercise (and for that matter, sex—which combines exercise, physiological arousal, and usually also foreign bodies to respond to) are all options that can improve circulation and stimulate the immune system.
You can read more about using some of these sorts of tricks for improving health in very well-evidenced, robustly scientific ways here:
The Stress Prescription (Against Aging!)
Take care!
Share This Post
-
Feta Cheese vs Mozzarella – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing feta to mozzarella, we picked the mozzarella.
Why?
There are possible arguments for both, but there are a couple of factors that we think tip the balance.
In terms of macronutrients, feta has more fat, of which, more saturated fat, and more cholesterol. Meanwhile, mozzarella has about twice the protein, which is substantial for a cheese. So this section’s a fair win for mozzarella.
In the category of vitamins, however, feta wins with more of vitamins B1, B2, B3, B6, B9, B12, D, & E. In contrast, mozzarella boasts only a little more vitamin A and choline. An easy win for feta in this section.
When it comes to minerals, the matter is decided, we say. Mozzarella has more calcium, magnesium, phosphorus, and potassium, while feta has more copper, iron, and (which counts against it) sodium. A win for mozzarella.
About that sodium… A cup of mozzarella contains about 3% of the RDA of sodium, while a cup of feta contains about 120% of the RDA of sodium. You see the problem? So, while mozzarella was already winning based on adding up the previous categories, the sodium content alone is a reason to choose mozzarella for your salad rather than feta.
That settles it, but just before we close, we’ll mention that they do both have great gut-healthy properties, containing healthy probiotics.
In short: if it weren’t for the difference in sodium content, this would be a narrow win for mozzarella. As it is, however, it’s a clear win.
Want to learn more?
You might like to read:
- Making Friends With Your Gut (You Can Thank Us Later)
- Is Dairy Scary? ← the answer is “it can be, but it depends on the product, and some are healthy; the key is in knowing which”
- How Too Much Salt May Lead To Organ Failure
Take care!
Share This Post
-
An Elegant Defense – by Matt Richtel
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In a way, Richtel got the best and worst of the publication date lottery. This book, which he’d obviously been working on for however long, was published in March 2020. Yes, that March 2020. So, it obviously got a huge boost in sales that launced it to bestseller status, and/but it doesn’t actually discuss COVID at all.
What it does discuss, is—as one might expect—the immune system. Or really, the immune systems, plural, several systems working alongside each other. How we got to have such, how our immune functions work, where all the various immune cells come from and what part they play. What pathogens can do to fight and/or confuse (or even co-opt) our immune response, and what modern medicine can do to counteract the pathogens’ anti-countermeasure countermeasures. And how it can still go wrong.
The “Four Lives” promised in the subtitle are stories, and Richtel explains the immune system through specific people’s specific battles. In particular, a friend of his who had quite a remarkable battle against cancer, which was of course terrible for him, but illustrative for us.
The style of the book is very readably journalistic. The author is a Pulitzer-winning NYT journalist, and not normally a science writer. Here at 10almonds, “we like big bibliographies and we cannot lie”, and we didn’t get to enjoy that in this case. The book contained no bibliography (nor appropriate inline citations, nor equivalent footnotes). Maybe a future addition will include this.
Bottom line: there’s a lot of “science for the lay reader” here. While the lack of references is a big oversight, the book does give a very good overview of what both sides (immune response and pathogenic invasion) bring to the battle of your body.
Click here to check out Elegant Defense, and demystify immunology!
Share This Post
Related Posts
-
As the U.S. Struggles With a Stillbirth Crisis, Australia Offers a Model for How to Do Better
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
ProPublica is a Pulitzer Prize-winning investigative newsroom. Sign up for The Big Story newsletter to receive stories like this one in your inbox.
Series: Stillbirths:When Babies Die Before Taking Their First Breath
The U.S. has not prioritized stillbirth prevention, and American parents are losing babies even as other countries make larger strides to reduce deaths late in pregnancy.
The stillbirth of her daughter in 1999 cleaved Kristina Keneally’s life into a before and an after. It later became a catalyst for transforming how an entire country approaches stillbirths.
In a world where preventing stillbirths is typically far down the list of health care priorities, Australia — where Keneally was elected as a senator — has emerged as a global leader in the effort to lower the number of babies that die before taking their first breaths. Stillbirth prevention is embedded in the nation’s health care system, supported by its doctors, midwives and nurses, and touted by its politicians.
In 2017, funding from the Australian government established a groundbreaking center for research into stillbirths. The next year, its Senate established a committee on stillbirth research and education. By 2020, the country had adopted a national stillbirth plan, which combines the efforts of health care providers and researchers, bereaved families and advocacy groups, and lawmakers and government officials, all in the name of reducing stillbirths and supporting families. As part of that plan, researchers and advocates teamed up to launch a public awareness campaign. All told, the government has invested more than $40 million.
Meanwhile, the United States, which has a far larger population, has no national stillbirth plan, no public awareness campaign and no government-funded stillbirth research center. Indeed, the U.S. has long lagged behind Australia and other wealthy countries in a crucial measure: how fast the stillbirth rate drops each year.
According to the latest UNICEF report, the U.S. was worse than 151 countries in reducing its stillbirth rate between 2000 and 2021, cutting it by just 0.9%. That figure lands the U.S. in the company of South Sudan in Africa and doing slightly better than Turkmenistan in central Asia. During that period, Australia’s reduction rate was more than double that.
Definitions of stillbirth vary by country, and though both Australia and the U.S. mark stillbirths as the death of a fetus at 20 weeks or more of pregnancy, to fairly compare countries globally, international standards call for the use of the World Health Organization definition that defines stillbirth as a loss after 28 weeks. That puts the U.S. stillbirth rate in 2021 at 2.7 per 1,000 total births, compared with 2.4 in Australia the same year.
Every year in the United States, more than 20,000 pregnancies end in a stillbirth. Each day, roughly 60 babies are stillborn. Australia experiences six stillbirths a day.
Over the past two years, ProPublica has revealed systemic failures at the federal and local levels, including not prioritizing research, awareness and data collection, conducting too few autopsies after stillbirths and doing little to combat stark racial disparities. And while efforts are starting to surface in the U.S. — including two stillbirth-prevention bills that are pending in Congress — they lack the scope and urgency seen in Australia.
“If you ask which parts of the work in Australia can be done in or should be done in the U.S., the answer is all of it,” said Susannah Hopkins Leisher, a stillbirth parent, epidemiologist and assistant professor in the stillbirth research program at the University of Utah Health. “There’s no physical reason why we cannot do exactly what Australia has done.”
Australia’s goal, which has been complicated by the pandemic, is to, by 2025, reduce the country’s rate of stillbirths after 28 weeks by 20% from its 2020 rate. The national plan laid out the target, and it is up to each jurisdiction to determine how to implement it based on their local needs.
The most significant development came in 2019, when the Stillbirth Centre of Research Excellence — the headquarters for Australia’s stillbirth-prevention efforts — launched the core of its strategy, a checklist of five evidence-based priorities known as the Safer Baby Bundle. They include supporting pregnant patients to stop smoking; regular monitoring for signs that the fetus is not growing as expected, which is known as fetal growth restriction; explaining the importance of acting quickly if fetal movement changes or decreases; advising pregnant patients to go to sleep on their side after 28 weeks; and encouraging patients to talk to their doctors about when to deliver because in some cases that may be before their due date.
Officials estimate that at least half of all births in the country are covered by maternity services that have adopted the bundle, which focuses on preventing stillbirths after 28 weeks.
“These are babies whose lives you would expect to save because they would survive if they were born alive,” said Dr. David Ellwood, a professor of obstetrics and gynecology at Griffith University, director of maternal-fetal medicine at Gold Coast University Hospital and a co-director of the Stillbirth Centre of Research Excellence.
Australia wasn’t always a leader in stillbirth prevention.
In 2000, when the stillbirth rate in the U.S. was 3.3 per 1,000 total births, Australia’s was 3.7. A group of doctors, midwives and parents recognized the need to do more and began working on improving their data classification and collection to better understand the problem areas. By 2014, Australia published its first in-depth national report on stillbirth. Two years later, the medical journal The Lancet published the second report in a landmark series on stillbirths, and Australian researchers applied for the first grant from the government to create the stillbirth research center.
But full federal buy-in remained elusive.
As parent advocates, researchers, doctors and midwives worked to gain national support, they didn’t yet know they would find a champion in Keneally.
Keneally’s improbable journey began when she was born in Nevada to an American father and Australian mother. She grew up in Ohio, graduating from the University of Dayton before meeting the man who would become her husband and moving to Australia.
When she learned that her daughter, who she named Caroline, would be stillborn, she remembers thinking, “I’m smart. I’m educated. How did I let this happen? And why did nobody tell me this was a possible outcome?”
A few years later, in 2003, Keneally decided to enter politics. She was elected to the lower house of state parliament in New South Wales, of which Sydney is the capital. In Australia, newly elected members are expected to give a “first speech.” She was able to get through just one sentence about Caroline before starting to tear up.
As a legislator, Keneally didn’t think of tackling stillbirth as part of her job. There wasn’t any public discourse about preventing stillbirths or supporting families who’d had one. When Caroline was born still, all Keneally got was a book titled “When a Baby Dies.”
In 2009, Keneally became New South Wales’ first woman premier, a role similar to that of an American governor. Another woman who had suffered her own stillbirth and was starting a stillbirth foundation learned of Keneally’s experience. She wrote to Keneally and asked the premier to be the foundation’s patron.
What’s the point of being the first female premier, Keneally thought, if I can’t support this group?
Like the U.S., Australia had previously launched an awareness campaign that contributed to a staggering reduction in sudden infant death syndrome, or SIDS. But there was no similar push for stillbirths.
“If we can figure out ways to reduce SIDS,” Keneally said, “surely it’s not beyond us to figure out ways to reduce stillbirth.”
She lost her seat after two years and took a break from politics, only to return six years later. In 2018, she was selected to serve as a senator at Australia’s federal level.
Keneally saw this as her second chance to fight for stillbirth prevention. In the short period between her election and her inaugural speech, she had put everything in place for a Senate inquiry into stillbirth.
In her address, Keneally declared stillbirth a national public health crisis. This time, she spoke at length about Caroline.
“When it comes to stillbirth prevention,” she said, “there are things that we know that we’re not telling parents, and there are things we don’t know, but we could, if we changed how we collected data and how we funded research.”
The day of her speech, March 27, 2018, she and her fellow senators established the Select Committee on Stillbirth Research and Education.
Things moved quickly over the next nine months. Keneally and other lawmakers traveled the country holding hearings, listening to testimony from grieving parents and writing up their findings in a report released that December.
“The culture of silence around stillbirth means that parents and families who experience it are less likely to be prepared to deal with the personal, social and financial consequences,” the report said. “This failure to regard stillbirth as a public health issue also has significant consequences for the level of funding available for research and education, and for public awareness of the social and economic costs to the community as a whole.”
It would be easy to swap the U.S. for Australia in many places throughout the report. Women of Aboriginal and Torres Strait Islander backgrounds experienced double the rate of stillbirth of other Australian women; Black women in America are more than twice as likely as white women to have a stillbirth. Both countries faced a lack of coordinated research and corresponding funding, low autopsy rates following a stillbirth and poor public awareness of the problem.
The day after the report’s release, the Australian government announced that it would develop a national plan and pledged $7.2 million in funding for prevention. Nearly half was to go to education and awareness programs for women and their health care providers.
In the following months, government officials rolled out the Safer Baby Bundle and pledged another $26 million to support parents’ mental health after a loss.
Many in Australia see Keneally’s first speech as senator, in 2018, as the turning point for the country’s fight for stillbirth prevention. Her words forced the federal government to acknowledge the stillbirth crisis and launch the national action plan with bipartisan support.
Australia’s assistant minister for health and aged care, Ged Kearney, cited Keneally’s speech in an email to ProPublica where she noted that Australia has become a world leader in stillbirth awareness, prevention and supporting families after a loss.
“Kristina highlighted the power of women telling their story for positive change,” Kearney said, adding, “As a Labor Senator Kristina Keneally bravely shared her deeply personal story of her daughter Caroline who was stillborn in 1999. Like so many mothers, she helped pave the way for creating a more compassionate and inclusive society.”
Keneally, who is now CEO of Sydney Children’s Hospitals Foundation, said the number of stillbirths a day in Australia spurred the movement for change.
“Six babies a day,” Keneally said. “Once you hear that fact, you can’t unhear it.”
Australia’s leading stillbirth experts watched closely as the country moved closer to a unified effort. This was the moment for which they had been waiting.
“We had all the information needed, but that’s really what made it happen.” said Vicki Flenady, a perinatal epidemiologist, co-director of the Stillbirth Centre of Research Excellence based at the Mater Research Institute at the University of Queensland, and a lead author on The Lancet’s stillbirth series. “I don’t think there’s a person who could dispute that.”
Flenady and her co-director Ellwood had spent more than two decades focused on stillbirths. After establishing the center in 2017, they were now able to expand their team. As part of their work with the International Stillbirth Alliance, they reached out to other countries with a track record of innovation and evidence-based research: the United Kingdom, the Netherlands, Ireland. They modeled the Safer Baby Bundle after a similar one in the U.K., though they added some elements.
In 2019, the state of Victoria, home to Melbourne, was the first to implement the Safer Baby Bundle. But 10 months into the program, the effort had to be paused for several months because of the pandemic, which forced other states to cancel their launches altogether.
“COVID was a major disruption. We stopped and started,” Flenady said.
Still, between 2019 and 2021, participating hospitals across Victoria were able to reduce their stillbirth rate by 21%. That improvement has yet to be seen at the national level.
A number of areas are still working on implementing the bundle. Westmead Hospital, one of Australia’s largest hospitals, planned to wrap that phase up last month. Like many hospitals, Westmead prominently displays the bundle’s key messages in the colorful posters and flyers hanging in patient rooms and in the hallways. They include easy-to-understand slogans such as, “Big or small. Your baby’s growth matters,” and, “Sleep on your side when baby’s inside.”
As patients at Westmead wait for their names to be called, a TV in the waiting room plays a video on stillbirth prevention, highlighting the importance of fetal movement. If a patient is concerned their baby’s movements have slowed down, they are instructed to come in to be seen within two hours. The patient’s chart gets a colorful sticker with a 16-point checklist of stillbirth risk factors.
Susan Heath, a senior clinical midwife at Westmead, came up with the idea for the stickers. Her office is tucked inside the hospital’s maternity wing, down a maze of hallways. As she makes the familiar walk to her desk, with her faded hospital badge bouncing against her navy blue scrubs, it’s clear she is a woman on a mission. The bundle gives doctors and midwives structure and uniform guidance, she said, and takes stillbirth out of the shadows. She reminds her staff of how making the practices a routine part of their job has the power to change their patients’ lives.
“You’re trying,” she said, “to help them prevent having the worst day of their life.”
Christine Andrews, a senior researcher at the Stillbirth Centre who is leading an evaluation of the program’s effectiveness, said the national stillbirth rate beyond 28 weeks has continued to slowly improve.
“It is going to take a while until we see the stillbirth rate across the whole entire country go down,” Andrews said. “We are anticipating that we’re going to start to see a shift in that rate soon.”
As officials wait to receive and standardize the data from hospitals and states, they are encouraged by a number of indicators.
For example, several states are reporting increases in the detection of babies that aren’t growing as they should, a major factor in many late-gestation stillbirths. Many also have seen an increase in the number of pregnant patients who stopped smoking. Health care providers also are more consistently offering post-stillbirth investigations, such as autopsies.
In addition to the Safer Baby Bundle, the national plan also calls for raising awareness and reducing racial disparities. The improvements it recommends for bereavement care are already gaining global attention.
To fulfill those directives, Australia has launched a “Still Six Lives” public awareness campaign, has implemented a national stillbirth clinical care standard and has spent two years developing a culturally inclusive version of the Safer Baby Bundle for First Nations, migrant and refugee communities. Those resources, which were recently released, incorporated cultural traditions and used terms like Stronger Bubba Born for the bundle and “sorry business babies,” which is how some Aboriginal and Torres Strait Islander women refer to stillbirth. There are also audio versions for those who can’t or prefer not to read the information.
In May, nearly 50 people from the state of Queensland met in a large hotel conference room. Midwives, doctors and nurses sat at round tables with government officials, hospital administrators and maternal and infant health advocates. Some even wore their bright blue Safer Baby T-shirts.
One by one, they discussed their experiences implementing the Safer Baby Bundle. One midwifery group was able to get more than a third of its patients to stop smoking between their first visit and giving birth.
Officials from a hospital in one of the fastest-growing areas in the state discussed how they carefully monitored for fetal growth restriction.
And staff from another hospital, which serves many low-income and immigrant patients, described how 97% of pregnant patients who said their baby’s movements had decreased were seen for additional monitoring within two hours of voicing their concern.
As the midwives, nurses and doctors ticked off the progress they were seeing, they also discussed the fear of unintended consequences: higher rates of premature births or increased admissions to neonatal intensive care units. But neither, they said, has materialized.
“The bundle isn’t causing any harm and may be improving other outcomes, like reducing early-term birth,” Flenady said. “I think it really shows a lot of positive impact.”
As far behind as the U.S. is in prioritizing stillbirth prevention, there is still hope.
Dr. Bob Silver, who co-authored a study that estimated that nearly 1 in 4 stillbirths are potentially preventable, has looked to the international community as a model. Now, he and Leisher — the University of Utah epidemiologist and stillbirth parent — are working to create one of the first stillbirth research and prevention centers in the U.S. in partnership with stillbirth leaders from Australia and other countries. They hope to launch next year.
“There’s no question that Australia has done a better job than we have,” said Silver, who is also chair of the University of Utah Health obstetrics and gynecology department. “Part of it is just highlighting it and paying attention to it.”
It’s hard to know what parts of Australia’s strategy are making a difference — the bundle as a whole, just certain elements of it, the increased stillbirth awareness across the country, or some combination of those things. Not every component has been proven to decrease stillbirth.
The lack of U.S. research on the issue has made some cautious to adopt the bundle, Silver said, but it is clear the U.S. can and should do more.
There comes a point when an issue is so critical, Silver said, that people have to do the best they can with the information that they have. The U.S. has done that with other problems, such as maternal mortality, he said, though many of the tactics used to combat that problem have not been proven scientifically.
“But we’ve decided this problem is so bad, we’re going to try the things that we think are most likely to be helpful,” Silver said.
After more than 30 years of working on stillbirth prevention, Silver said the U.S. may be at a turning point. Parents’ voices are getting louder and starting to reach lawmakers. More doctors are affirming that stillbirths are not inevitable. And pressure is mounting on federal institutions to do more.
Of the two stillbirth prevention bills in Congress, one already sailed through the Senate. The second bill, the Stillbirth Health Improvement and Education for Autumn Act, includes features that also appeared in Australia’s plan, such as improving data, increasing awareness and providing support for autopsies.
And after many years, the National Institutes of Health has turned its focus back to stillbirths. In March, it released a report with a series of recommendations to reduce the nation’s stillbirth rate that mirror ProPublica’s reporting about some of the causes of the crisis. Since then, it has launched additional groups to begin to tackle three critical angles: prevention, data and bereavement. Silver co-chairs the prevention group.
In November, more than 100 doctors, parents and advocates gathered for a symposium in New York City to discuss everything from improving bereavement care in the U.S to tackling racial disparities in stillbirth. In 2022, after taking a page out of the U.K.’s book, the city’s Mount Sinai Hospital opened the first Rainbow Clinic in the U.S., which employs specific protocols to care for people who have had a stillbirth.
But given the financial resources in the U.S. and the academic capacity at American universities and research institutions, Leisher and others said federal and state governments aren’t doing nearly enough.
“The U.S. is not pulling its weight in relation either to our burden or to the resources that we have at our disposal,” she said. “We’ve got a lot of babies dying, and we’ve got a really bad imbalance of who those babies are as well. And yet we look at a country with a much smaller number of stillbirths who is leading the world.”
“We can do more. Much more. We’re just not,” she added. “It’s unacceptable.”
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Get Past Executive Dysfunction
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In mathematics, there is a thing called the “travelling salesman problem”, and it is hard. Not just subjectively; it is classified in mathematical terms as an “NP-hard problem”, wherein NP stands for “nondeterministic polynomial”.
The problem is: a travelling salesman must visit a certain list of cities, order undetermined, by the shortest possible route that visits them all.
To work out what the shortest route is involves either very advanced mathematics, or else solving it by brute force, which means measuring every possible combination order (which number gets exponentially larger very quickly after the first few cities) and then selecting the shortest.
Why are we telling you this?
Executive dysfunction’s analysis paralysis
Executive dysfunction is the state of knowing you have things to do, wanting to do them, intending to do them, and then simply not doing them.
Colloquially, this can be called “analysis paralysis” and is considered a problem of planning and organizing, as much as it is a problem of initiating tasks.
Let’s give a simple example:
You wake up in the morning, and you need to go to the bathroom. But the bathroom will be cold, so you’ll want to get dressed first. However, it will be uncomfortable to get dressed while you still need to use the bathroom, so you contemplate doing that first. Those two items are already a closed loop now. You’re thirsty, so you want to have a drink, but the bathroom is calling to you. Sitting up, it’s colder than under the covers, so you think about getting dressed. Maybe you should have just a sip of water first. What else do you need to do today anyway? You grab your phone to check, drink untouched, clothes unselected, bathroom unvisited.
That was a simple example; now apply that to other parts of your day that have much more complex planning possible.
This is like the travelling salesman problem, except that now, some things are better if done before or after certain other things. Sometimes, possibly, they are outright required to be done before or after certain other things.
So you have four options:
- Solve the problem of your travelling-salesman-like tasklist using advanced mathematics (good luck if you don’t have advanced mathematics)
- Solve the problem by brute force, calculating all possible variations and selecting the shortest (good luck getting that done the same day)
- Go with a gut feeling and stick to it (people without executive dysfunction do this)
- Go towards the nearest item, notice another item on the way, go towards that, notice a different item on the way there, and another one, get stuck for a while choosing between those two, head towards one, notice another one, and so on until you’ve done a very long scenic curly route that has narrowly missed all of your targetted items (this is the executive dysfunction approach).
So instead, just pick one, do it, pick another one, do it, and so forth.
That may seem “easier said than done”, but there are tools available…
Task zero
We’ve mentioned this before in the little section at the top of our daily newsletter that we often use for tips.
One of the problems that leads to executive function is a shortage of “working memory”, like the RAM of a computer, so it’s easy to get overwhelmed with lists of things to do.
So instead, hold only two items in your mind:
- Task zero: the thing you are doing right now
- Task one: the thing you plan to do next
When you’ve completed task zero, move on to task one, renaming it task zero, and select a new task one.
With this approach, you will never:
- Think “what did I come into this room for?”
- Get distracted by alluring side-quests
Do not get corrupted by the cursed artefact
In fantasy, and occasionally science fiction, there is a trope: an item that people are drawn towards, but which corrupts them, changes their motivations and behaviors for the worse, as well as making them resistant to giving the item up.
An archetypal example of this would be the One Ring from The Lord of the Rings.
It’s easy to read/watch and think “well I would simply not be corrupted by the cursed artefact”.
And then pick up one’s phone to open the same three apps in a cycle for the next 40 minutes.
This is because technology that is designed to be addictive hijacks our dopamine processing, and takes advantage of executive dysfunction, while worsening it.
There are some ways to mitigate this:
Rebalancing Dopamine (Without “Dopamine Fasting”)
…but one way to avoid it entirely is to mentally narrate your choices. It’s a lot harder to make bad choices with an internal narrator going:
- “She picked up her phone absent-mindedly, certain that this time it really would be only a few seconds”
- “She picked up her phone for the eleventy-third time”
- “Despite her plan to put her shoes on, she headed instead for the kitchen”
This method also helps against other bad choices aside from those pertaining to executive dysfunction, too:
- “Abandoning her plan to eat healthily, she lingered in the confectionary aisle, scanning the shelves for sugary treats”
- “Monday morning will be the best time to start my new exercise regime”, she thought, for the 35th week so far this year
Get pharmaceutical or nutraceutical help
While it’s not for everyone, many people with executive dysfunction benefit from ADHD meds. However, they have their pros and cons (perhaps we’ll do a run-down one of these days).
There are also gentler options that can significantly ameliorate executive dysfunction, for example:
Bacopa Monnieri: A Well-Evidenced Cognitive Enhancer For Focus & More
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Stretching Scientifically – by Thomas Kurz
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
People stretching incorrectly can, even if they don’t injure themselves, lose countless hours for negligible flexibility gains, and put the failure down to their body rather than the method. You can have better.
This book’s all about what works, and not only that, but what works with specific goals in mind, beyond the generic “do the splits” and “touch your toes” etc, which are laudable goals but quite basic. A lot of the further goals he has in mind have to do not just with flexibility, but also functional dynamic strength and mobility, because it’s of less versatile use to have the flexibility only to get folded like laundry and not actually actively do the things you want to.
He does also cover “regardless of age”, so no more worrying that you should have been trained for the ballet when you were eight and now all is lost. It isn’t.
As for the writing style… The author, a physical fitness and rehabilitation coach and writer, wrote this book while at the Academy of Physical Education in Warsaw during the Soviet period, and it shows. It is very much straight-to-the-point, no nonsense, no waffle. Everything is direct and comes with a list of research citations and clear instructions.
Bottom line: if you’ve been trying to improve your flexibility and not succeeding, let this old Soviet instructor have a go.
Click here to check out Stretching Scientifically, and stretch scientifically!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: