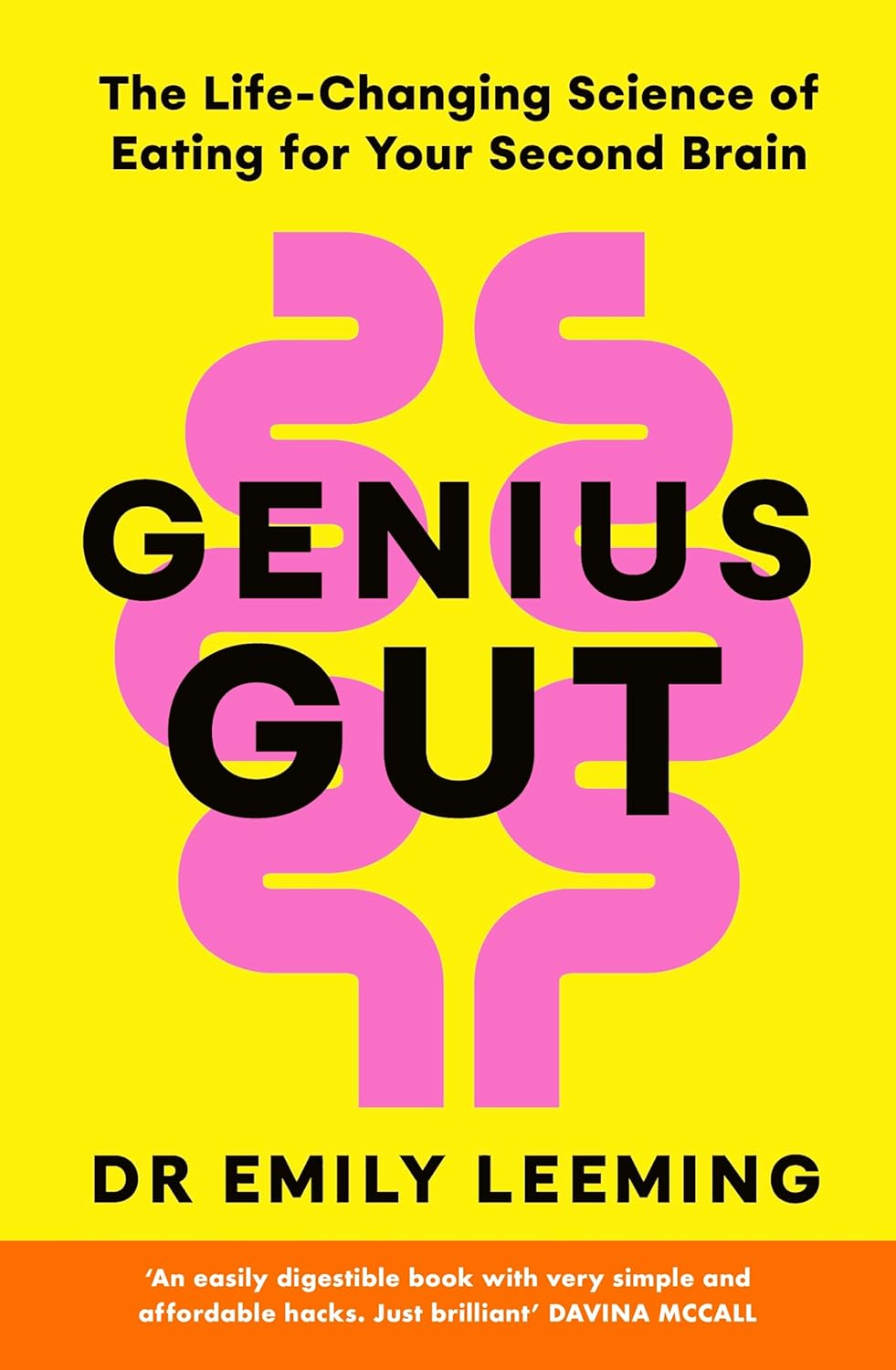
Genius Gut – by Dr. Emily Leeming
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When it comes to the gut-brain information interchange, 90% of it is the gut talking to the brain (the brain is a good listener). As such, one of the best things we can do for our brain is ensure our gut has good things to say.
Dr. Leeming talks us through doing a quick initial assessment to judge the general goodness/badness of our current gut situation (based on output, not input, so it’s about the actual goodness/badness, not what we expect it should be), before going on to explain a lot of the anatomy and physiology at hand.
The hacks themselves may be, in their titles, things you already know—but where the real value of this book lies is in all the data and science collated under each of those hacks, allowing the reader to optimize everything rather than just guessing. Which can mean optimize by doing things as close to perfectly as possible, or it can mean optimize by doing/using the things that get the best results for the minimum effort. It’s up to you!
The style is very casual and friendly, even conversational, while not skimping on science (and indeed, citations are frequently provided for such).
Bottom line: if you’d like to improve your gut health, especially with the goal of improving your brain health, this is an excellent book for that.
Click here to check out Genius Gut, and make yours better for you!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:

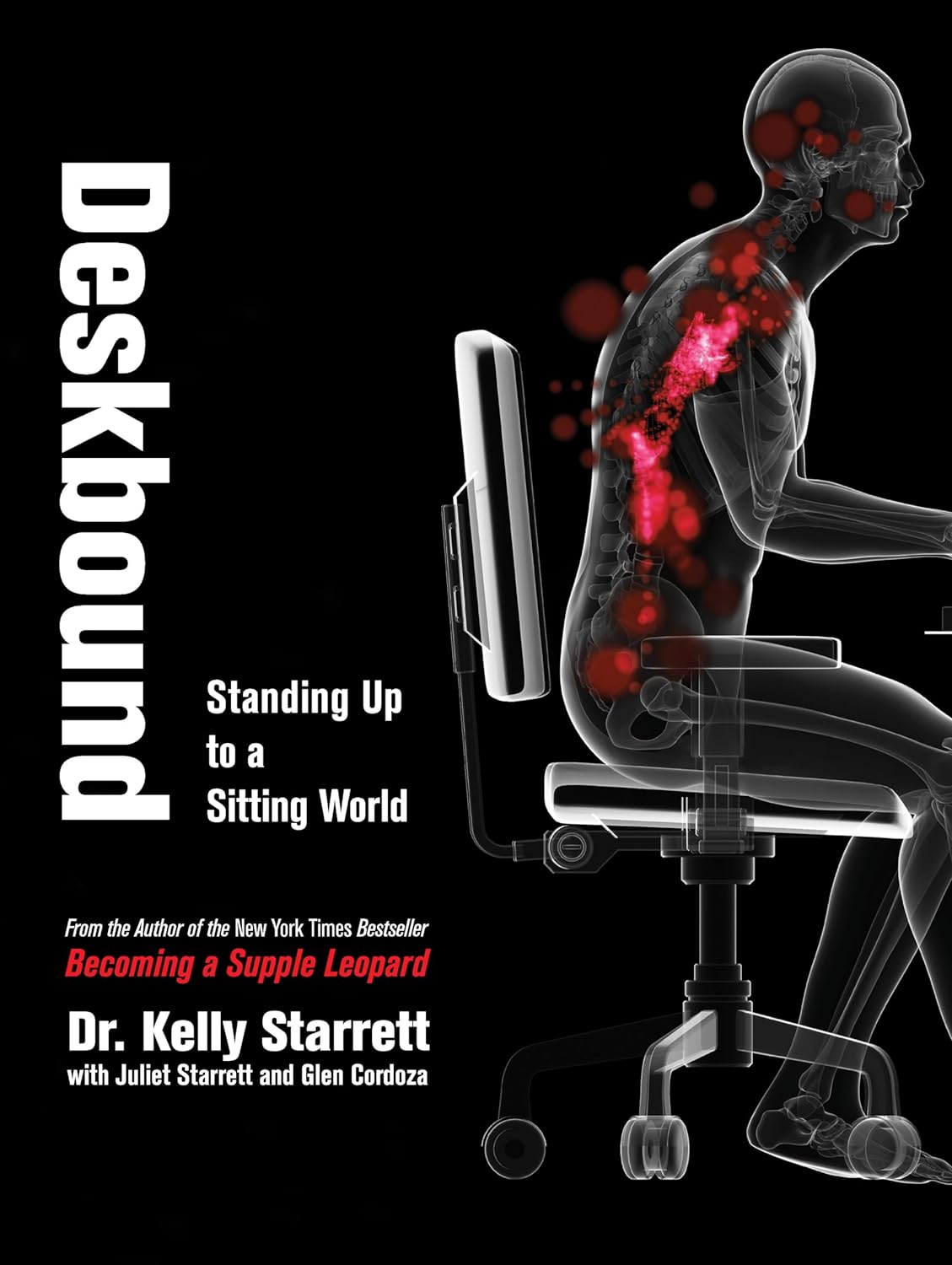
Deskbound – by Kelly Starrett and Glen Cordoza
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve all heard that “sitting is the new smoking”, and whether or not that’s an exaggeration (the jury’s out), one thing that is clear is that sitting is very bad.
Popular advice is “here’s how to sit with good posture and stretch your neck sometimes”… but that advice tends to come from companies that pay people to sit for a long time. They might not be the a very unbiased source.
Starrett and Cordoza offer better. After one opening chapter covering the multifarious ways sitting ruins our health, the rest of the book is all advice, covering:
- The principles of how the body is supposed to be
- The most important movements that we should be doing
- A dynamic workstation setup
- This is great, because “get a standing desk” tends to present more questions than answers, and can cause as much harm as good if done wrong
- The authors also cover how to progressively cut down on sitting, rather than try to go cold-turkey.
- They also recognize that not everyone can stand at all, and…
- Optimizing the sitting position, for when we must sit
- Exercises to maintain our general mobility and compensate about as well as we can for the body-unfriendly nature of modern life.
The book is mostly explanations, so at 682 pages, you can imagine it’s not just “get up, lazybones!”. Rather, things are explained in such detail (and with many high-quality medical diagrams) so that we can truly understand them.
Most of us have gone through life knowing we should have “better posture” and “move more”… but without the details, that can be hard to execute correctly, and worse, we can even sabotage our bodies unknowingly with incorrect form.
This book straightens all that out very comprehensively, and we highly recommend it.
Share This Post

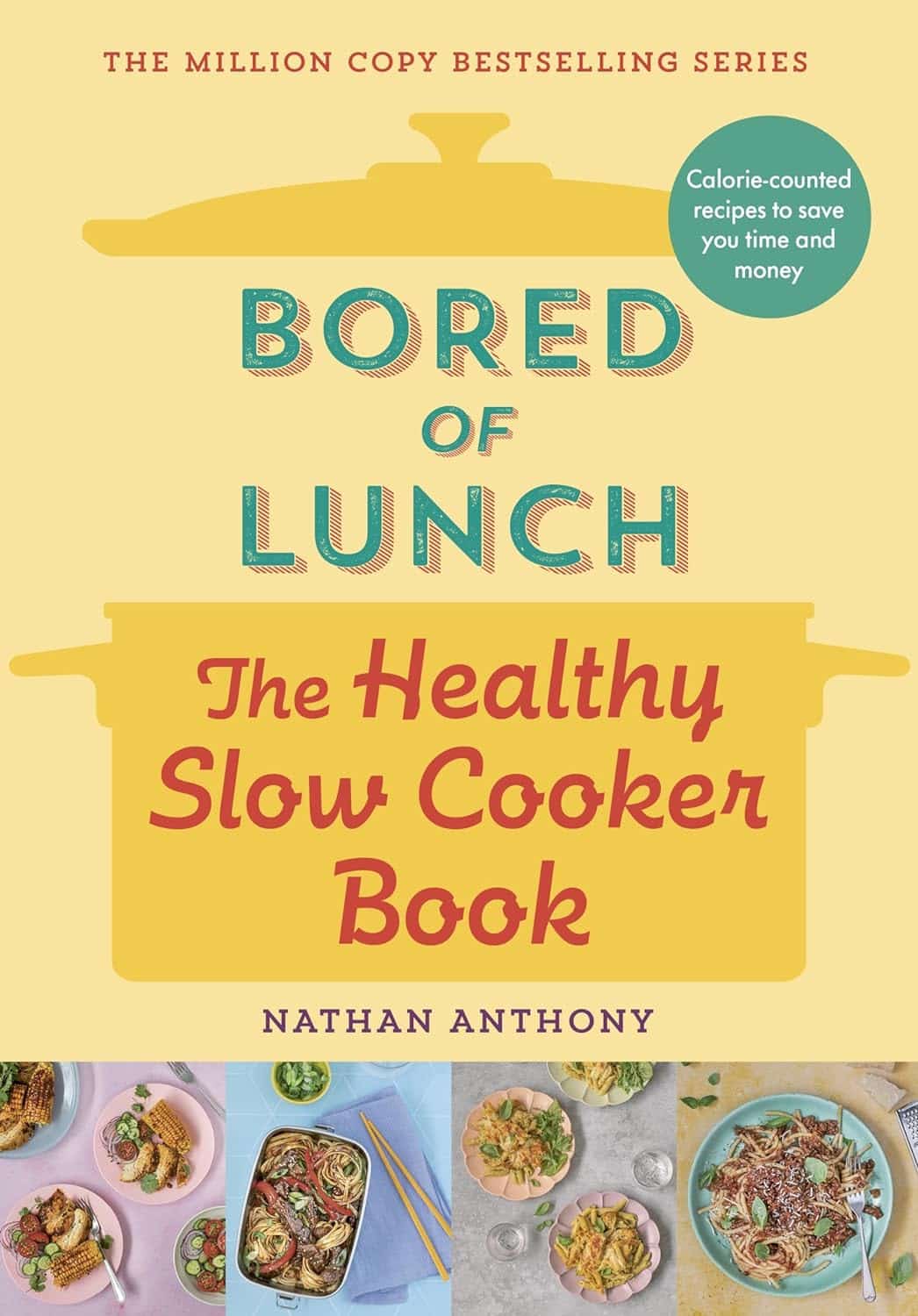
Bored of Lunch – by Nathan Anthony
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Cooking with a slow cooker is famously easy, but often we settle down on a few recipes and then don’t vary. This book brings a healthy dose of inspiration and variety.
The recipes themselves range from comfort food to fancy entertaining, pasta dishes to risottos, and even what the author categorizes as “fakeaways” (a play on the British English “takeaway”, cf. AmE “takeout”), so indulgent nights in have never been healthier!
For each recipe, you’ll see a nice simple clear layout of all you’d expect (ingredients, method, etc) plus calorie count, so that you can have a rough idea of how much food each meal is.
In terms of dietary restrictions you may have, there’s quite a variety here so it’ll be easy to find things for all needs, and in addition to that, optional substitutions are mostly quite straightforward too.
Bottom line: if you have a slow cooker but have been cooking only the same three things in it for the past ten years, this is the book to liven things up, while staying healthy!
Share This Post

What is pathological demand avoidance – and how is it different to ‘acting out’?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
“Charlie” is an eight-year-old child with autism. Her parents are worried because she often responds to requests with insults, aggression and refusal. Simple demands, such as being asked to get dressed, can trigger an intense need to control the situation, fights and meltdowns.
Charlie’s parents find themselves in a constant cycle of conflict, trying to manage her and their own reactions, often unsuccessfully. Their attempts to provide structure and consequences are met with more resistance.
What’s going on? What makes Charlie’s behaviour – that some are calling “pathological demand avoidance” – different to the defiance most children show their parents or carers from time-to-time?
What is pathological demand avoidance?
British developmental psychologist Elizabeth Newson coined the term “pathological demand avoidance” (commonly shortened to PDA) in the 1980s after studying groups of children in her practice.
A 2021 systematic review noted features of PDA include resistance to everyday requests and strong emotional and behavioural reactions.
Children with PDA might show obsessive behaviour, struggle with persistence, and seek to control situations. They may struggle with attention and impulsivity, alongside motor and coordination difficulties, language delay and a tendency to retreat into role play or fantasy worlds.
PDA is also known as “extreme demand avoidance” and is often described as a subtype of autism. Some people prefer the term persistent drive for autonomy or pervasive drive for autonomy.
What does the evidence say?
Every clinician working with children and families recognises the behavioural profile described by PDA. The challenging question is why these behaviours emerge.
PDA is not currently listed in the two diagnostic manuals used in psychiatry and psychology to diagnose mental health and developmental conditions, the current Diagnostic and Statistical Manual of Mental Disorders (DSM-5) and the World Health Organization’s International Classification of Diseases (ICD-11).
Researchers have reported concerns about the science behind PDA. There are no clear theories or explanations of why or how the profile of symptoms develop, and little inclusion of children or adults with lived experience of PDA symptoms in the studies. Environmental, family or other contextual factors that may contribute to behaviour have not been systematically studied.
A major limitation of existing PDA research and case studies is a lack of consideration of overlapping symptoms with other conditions, such as autism, attention deficit hyperactivity disorder (ADHD), oppositional defiant disorder, anxiety disorder, selective mutism and other developmental disorders. Diagnostic labels can have positive and negative consequences and so need to be thoroughly investigated before they are used in practice.
Classifying a “new” condition requires consistency across seven clinical and research aspects: epidemiological data, long-term patient follow-up, family inheritance, laboratory findings, exclusion from other conditions, response to treatment, and distinct predictors of outcome. At this stage, these domains have not been established for PDA. It is not clear whether PDA is different from other formal diagnoses or developmental differences.

When a child is stressed, demands or requests might tip them into fight, flight or freeze mode. Shutterstock Finding the why
Debates over classification don’t relieve distress for a child or those close to them. If a child is “intentionally” engaged in antisocial behaviour, the question is then “why?”
Beneath the behaviour is almost always developmental difference, genuine distress and difficulty coping. A broad and deep understanding of developmental processes is required.
Interestingly, while girls are “under-represented” in autism research, they are equally represented in studies characterising PDA. But if a child’s behaviour is only understood through a “pathologising” or diagnostic lens, there is a risk their agency may be reduced. Underlying experiences of distress, sensory overload, social confusion and feelings of isolation may be missed.
So, what can be done to help?
There are no empirical studies to date regarding PDA treatment strategies or their effectiveness. Clinical advice and case studies suggest strategies that may help include:
- reducing demands
- giving multiple options
- minimising expectations to avoid triggering avoidance
- engaging with interests to support regulation.
Early intervention in the preschool and primary years benefits children with complex developmental differences. Clinical care that involves a range of medical and allied health clinicians and considers the whole person is needed to ensure children and families get the support they need.
It is important to recognise these children often feel as frustrated and helpless as their caregivers. Both find themselves stuck in a repetitive cycle of distress, frustration and lack of progress. A personalised approach can take into account the child’s unique social, sensory and cognitive sensitivities.
In the preschool and early primary years, children have limited ability to manage their impulses or learn techniques for managing their emotions, relationships or environments. Careful watching for potential triggers and then working on timetables and routines, sleep, environments, tasks, and relationships can help.
As children move into later primary school and adolescence, they are more likely to want to influence others and be able to have more self control. As their autonomy and ability to collaborate increases, the problematic behaviours tend to reduce.
Strategies that build self-determination are crucial. They include opportunities for developing confidence, communication and more options to choose from when facing challenges. This therapeutic work with children and families takes time and needs to be revisited at different developmental stages. Support to engage in school and community activities is also needed. Each small step brings more capacity and more effective ways for a child to understand and manage themselves and their worlds.
What about Charlie?
The current scope to explain and manage PDA is limited. Future research must include the voices and views of children and adults with PDA symptoms.
Such emotional and behavioural difficulties are distressing and difficult for children and families. They need compassion and practical help.
For a child like Charlie, this could look like a series of sessions where she and her parents meet with clinicians to explore Charlie’s perspective, experiences and triggers. The family might come to understand that, in addition to autism, Charlie has complex developmental strengths and challenges, anxiety, and some difficulties with adjustment related to stress at home and school. This means Charlie experiences a fight, flight, freeze response that looks like aggression, avoidance or shutting down.
With carefully planned supports at home and school, Charlie’s options can broaden and her distress and avoidance can soften. Outside the clinic room, Charlie and her family can be supported to join an inclusive local community sporting or creative activity. Gradually she can spend more time engaged at home, school and in the community.
Nicole Rinehart, Professor, Child and Adolescent Psychology, Director, Krongold Clinic (Research), Monash University; David Moseley, Senior Research Fellow, Deputy Director (Clinical), Monash Krongold Clinic, Monash University, and Michael Gordon, Associate Professor, Psychiatry, Monash University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts

Why do I keep getting urinary tract infections? And why are chronic UTIs so hard to treat?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dealing with chronic urinary tract infections (UTIs) means facing more than the occasional discomfort. It’s like being on a never ending battlefield against an unseen adversary, making simple daily activities a trial.
UTIs happen when bacteria sneak into the urinary system, causing pain and frequent trips to the bathroom.
Chronic UTIs take this to the next level, coming back repeatedly or never fully going away despite treatment. Chronic UTIs are typically diagnosed when a person experiences two or more infections within six months or three or more within a year.
They can happen to anyone, but some are more prone due to their body’s makeup or habits. Women are more likely to get UTIs than men, due to their shorter urethra and hormonal changes during menopause that can decrease the protective lining of the urinary tract. Sexually active people are also at greater risk, as bacteria can be transferred around the area.
Up to 60% of women will have at least one UTI in their lifetime. While effective treatments exist, about 25% of women face recurrent infections within six months. Around 20–30% of UTIs don’t respond to standard antibiotic. The challenge of chronic UTIs lies in bacteria’s ability to shield themselves against treatments.
Why are chronic UTIs so hard to treat?
Once thought of as straightforward infections cured by antibiotics, we now know chronic UTIs are complex. The cunning nature of the bacteria responsible for the condition allows them to hide in bladder walls, out of antibiotics’ reach.
The bacteria form biofilms, a kind of protective barrier that makes them nearly impervious to standard antibiotic treatments.
This ability to evade treatment has led to a troubling increase in antibiotic resistance, a global health concern that renders some of the conventional treatments ineffective.

Some antibiotics no longer work against UTIs.
Michael Ebardt/ShutterstockAntibiotics need to be advanced to keep up with evolving bacteria, in a similar way to the flu vaccine, which is updated annually to combat the latest strains of the flu virus. If we used the same flu vaccine year after year, its effectiveness would wane, just as overused antibiotics lose their power against bacteria that have adapted.
But fighting bacteria that resist antibiotics is much tougher than updating the flu vaccine. Bacteria change in ways that are harder to predict, making it more challenging to create new, effective antibiotics. It’s like a never-ending game where the bacteria are always one step ahead.
Treating chronic UTIs still relies heavily on antibiotics, but doctors are getting crafty, changing up medications or prescribing low doses over a longer time to outwit the bacteria.
Doctors are also placing a greater emphasis on thorough diagnostics to accurately identify chronic UTIs from the outset. By asking detailed questions about the duration and frequency of symptoms, health-care providers can better distinguish between isolated UTI episodes and chronic conditions.
The approach to initial treatment can significantly influence the likelihood of a UTI becoming chronic. Early, targeted therapy, based on the specific bacteria causing the infection and its antibiotic sensitivity, may reduce the risk of recurrence.
For post-menopausal women, estrogen therapy has shown promise in reducing the risk of recurrent UTIs. After menopause, the decrease in estrogen levels can lead to changes in the urinary tract that makes it more susceptible to infections. This treatment restores the balance of the vaginal and urinary tract environments, making it less likely for UTIs to occur.
Lifestyle changes, such as drinking more water and practising good hygiene like washing hands with soap after going to the toilet and the recommended front-to-back wiping for women, also play a big role.
Some swear by cranberry juice or supplements, though researchers are still figuring out how effective these remedies truly are.
What treatments might we see in the future?
Scientists are currently working on new treatments for chronic UTIs. One promising avenue is the development of vaccines aimed at preventing UTIs altogether, much like flu shots prepare our immune system to fend off the flu.

Emerging treatments could help clear chronic UTIs.
guys_who_shoot/ShutterstockAnother new method being looked at is called phage therapy. It uses special viruses called bacteriophages that go after and kill only the bad bacteria causing UTIs, while leaving the good bacteria in our body alone. This way, it doesn’t make the bacteria resistant to treatment, which is a big plus.
Researchers are also exploring the potential of probiotics. Probiotics introduce beneficial bacteria into the urinary tract to out-compete harmful pathogens. These good bacteria work by occupying space and resources in the urinary tract, making it harder for harmful pathogens to establish themselves.
Probiotics can also produce substances that inhibit the growth of harmful bacteria and enhance the body’s immune response.
Chronic UTIs represent a stubborn challenge, but with a mix of current treatments and promising research, we’re getting closer to a day when chronic UTIs are a thing of the past.

Iris Lim, Assistant Professor, Bond University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:

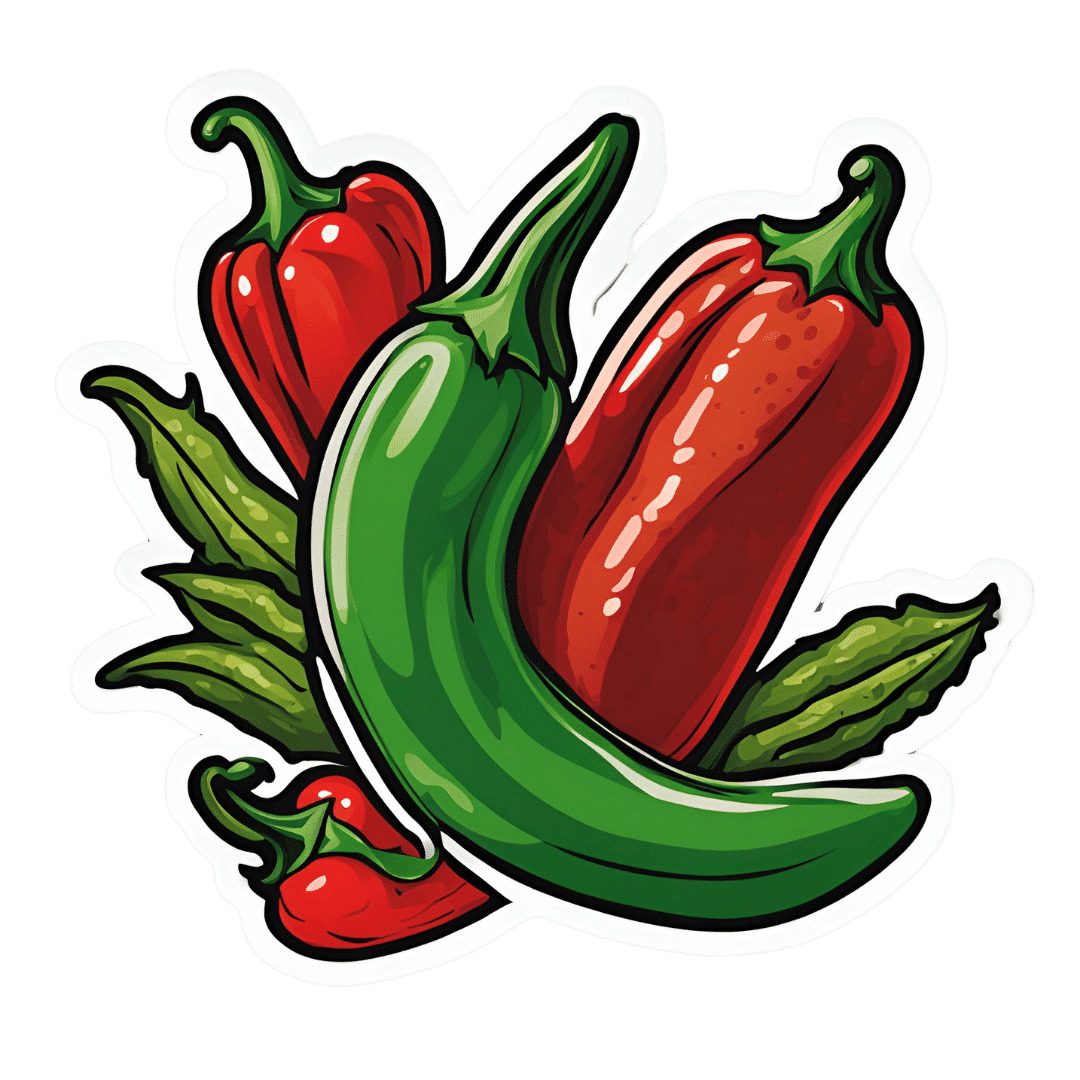
How Internal Organs Can Be Affected By Spicy Foods (Doctor Explains)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Capsaicin has an array of health-giving properties in moderation, but consumed in immoderation and/or without building up tolerance first, can cause problems—serious health issues such as heart attacks, brain spasms, torn esophagus, and even death can occur.
Heating up
Capsaicin, the compound that gives peppers their “heat”, is a chemical irritant and neurotoxin that activates pain receptors (TRPV1) tricking the brain into sensing heat, leading to a burning sensation, sweating, and flushing. The pain signal can also trigger the fight-or-flight response, causing a surge of adrenaline. Endorphins are eventually released, creating a pain-relief effect similar to a runner’s high, and ultimately it reduces systemic inflammation, boosts the metabolism, and increases healthy longevity.
However, in cases of extreme consumption and/or lack of preparation, woe can befall, for example:
- A man ruptured his esophagus after vomiting from eating a ghost pepper.
- A participant experienced severe brain blood vessel constriction (reversible cerebral vasoconstriction syndrome) after eating a Carolina reaper.
- A 25-year-old suffered permanent heart damage from cayenne pepper pills due to restricted blood flow.
- A teenager died after the “one chip challenge,” although the cause of death was undetermined.
So, what does moderation and preparation look like?
Moderation can be different to different people, since genetics do play a part—some people have more TRPV1 receptors than other people. However, for all people (unless in case of having an allergy or similar), acclimatization is important, and a much bigger factor than genetics.
Writer’s anecdote: on the other hand, when my son was a toddler I once left the room and came back to find him cheerfully drinking hot sauce straight from the bottle, so it can be suspected that genetics are definitely relevant too, as while I did season his food and he did already enjoy curries and such, he didn’t exactly have a background of entering chili-eating competitions.
Still, regardless of genes (unless you actually have a medical condition that disallows this), a person who regularly eats spicy food will develop an increasing tolerance for spicy food, and will get to enjoy the benefits without the risks, provided they don’t suddenly jump way past their point of tolerance.
On which note, in this video you can also see what happens when Dr. Deshauer goes from biting a jalapeño (relatively low on the Scoville heat scale) to biting a Scotch bonnet pepper (about 10x higher on the Scoville heat scale):
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Capsaicin For Weight Loss And Against Inflammation
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:

I’ve recovered from a cold but I still have a hoarse voice. What should I do?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Cold, flu, COVID and RSV have been circulating across Australia this winter. Many of us have caught and recovered from one of these common upper respiratory tract infections.
But for some people their impact is ongoing. Even if your throat isn’t sore anymore, your voice may still be hoarse or croaky.
So what happens to the voice when we get a virus? And what happens after?
Here’s what you should know if your voice is still hoarse for days – or even weeks – after your other symptoms have resolved.
Why does my voice get croaky during a cold?
A healthy voice is normally clear and strong. It’s powered by the lungs, which push air past the vocal cords to make them vibrate. These vibrations are amplified in the throat and mouth, creating the voice we hear.
The vocal cords are two elastic muscles situated in your throat, around the level of your laryngeal prominence, or Adam’s apple. (Although everyone has one, it tends to be more pronounced in males.) The vocal cords are small and delicate – around the size of your fingernail. Any small change in their structure will affect how the voice sounds.
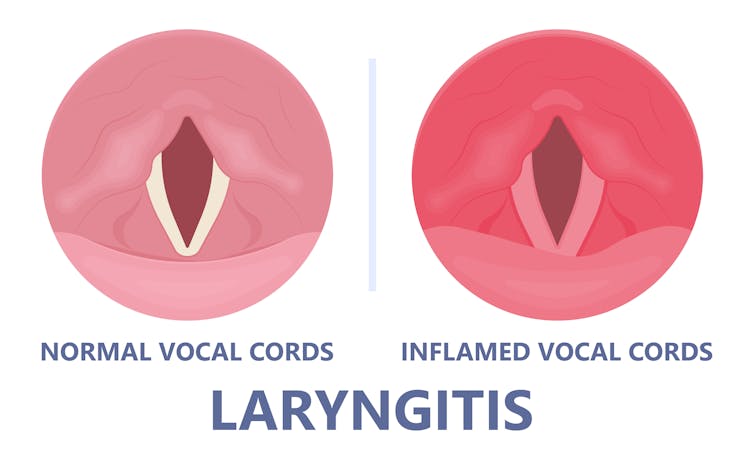
When the vocal cords become inflamed – known as laryngitis – your voice will sound different. Laryngitis is a common part of upper respiratory tract infections, but can also be caused through misuse.

Viruses such as the common cold can inflame the vocal cords. Pepermpron/Shutterstock Catching a virus triggers the body’s defence mechanisms. White blood cells are recruited to kill the virus and heal the tissues in the vocal cords. They become inflamed, but also stiffer. It’s harder for them to vibrate, so the voice comes out hoarse and croaky.
In some instances, you may find it hard to speak in a loud voice or have a reduced pitch range, meaning you can’t go as high or loud as normal. You may even “lose” your voice altogether.
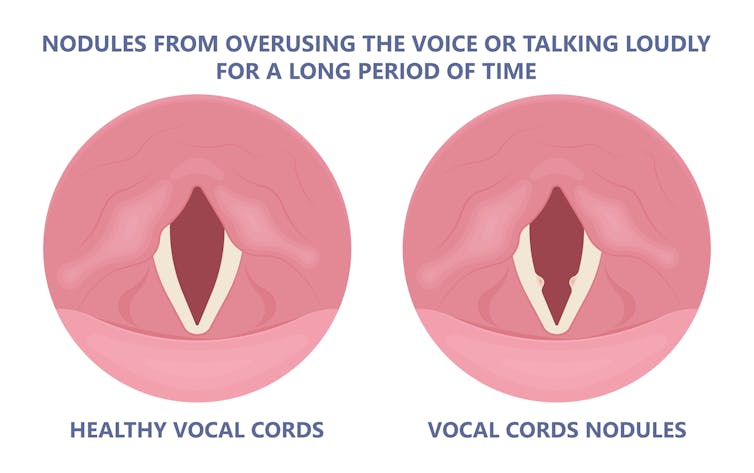
Coughing can also make things worse. It is the body’s way of trying to clear the airways of irritation, including your own mucus dripping onto your throat (post-nasal drip). But coughing slams the vocal cords together with force.
Chronic coughing can lead to persistent inflammation and even thicken the vocal cords. This thickening is the body trying to protect itself, similar to developing a callus when a pair of new shoes rubs.
Thickening on your vocal cords can lead to physical changes in the vocal cords – such as developing a growth or “nodule” – and further deterioration of your voice quality.

Coughing and exertion can cause inflamed vocal cords to thicken and develop nodules. Pepermpron/Shutterstock How can you care for your voice during infection?
People who use their voices a lot professionally – such as teachers, call centre workers and singers – are often desperate to resume their vocal activities. They are more at risk of forcing their voice before it’s ready.
The good news is most viral infections resolve themselves. Your voice is usually restored within five to ten days of recovering from a cold.
Occasionally, your pharmacist or doctor may prescribe cough suppressants to limit additional damage to the vocal cords (among other reasons) or mucolytics, which break down mucus. But the most effective treatments for viral upper respiratory tract infections are hydration and rest.
Drink plenty of water, avoid alcohol and exposure to cigarette smoke. Inhaling steam by making yourself a cup of hot water will also help clear blocked noses and hydrate your vocal cords.
Rest your voice by talking as little as possible. If you do need to talk, don’t whisper – this strains the muscles.
Instead, consider using “confidential voice”. This is a soft voice – not a whisper – that gently vibrates your vocal cords but puts less strain on your voice than normal speech. Think of the voice you use when communicating with someone close by.
During the first five to ten days of your infection, it is important not to push through. Exerting the voice by talking a lot or loudly will only exacerbate the situation. Once you’ve recovered from your cold, you can speak as you would normally.
What should you do if your voice is still hoarse after recovery?
If your voice hasn’t returned to normal after two to three weeks, you should seek medical attention from your doctor, who may refer you to an ear nose and throat specialist.
If you’ve developed a nodule, the specialist would likely refer you to a speech pathologist who will show you how to take care of your voice. Many nodules can be treated with voice therapy and don’t require surgery.
You may have also developed a habit of straining your vocal cords, if you forced yourself to speak or sing while they were inflamed. This can be a reason why some people continue to have a hoarse voice even when they’ve recovered from the cold.
In those cases, a speech pathologist may play a valuable role. They may teach you to exercises that make voicing more efficient. For example, lip trills (blowing raspberries) are a fun and easy way you can learn to relax the voice. This can help break the habit of straining your voice you may have developed during infection.
Yeptain Leung, Postdoctoral Research and Lecturer of Speech Pathology, School of Health Sciences, The University of Melbourne
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: