From Lupus To Arthritis: New Developments
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This week’s health news round-up highlights some things that are getting better, and some things that are getting worse, and how to be on the right side of both:
New hope for lupus sufferers
Lupus is currently treated mostly with lifelong medications to suppress the immune system, which is not only inconvenient, but also can leave people more open to infectious diseases. The latest development uses CAR T-cell technology (as has been used in cancer treatment for a while) to genetically modify cells to enable the body’s own immune system to behave properly:
Read in full: Exciting new lupus treatment could end need for lifelong medication
Related: How to Prevent (Or Reduce The Severity Of) Inflammatory Diseases
It’s in the hips
There are a lot of different kinds of hip replacements, and those with either delta ceramic or oxidised zirconium head with a highly cross-linked polyethylene liner/cup have the lowest risk of need for revision in the 15 years after surgery. This is important, because obviously, once it’s in there, you want it to be able to stay in there and not have to be touched again any time soon:
Read in full: Study identifies hip implant materials with the lowest risk of needing revision
Related: Nobody Likes Surgery, But Here’s How To Make It Much Less Bad
Sooner is better than later
Often, people won’t know about an unwanted pregnancy in the first six weeks, but for those who are able to catch it early, Very Early Medical Abortion (VEMA) offers a safe an effective way of doing so, with success rate being linked to earliness of intervention:
Read in full: Very early medication abortion is effective and safe, study finds
Related: What Might A Second Trump Presidency Look Like for Health Care?
Increased infectious disease risks from cattle farms
Many serious-to-humans infectious diseases enter the human population via the animal food chain, and in this case, bird flu becoming more rampant amongst cows is starting to pose a clear threat to humans, so this is definitely something to be aware of:
Read in full: Bird flu infects 1 in 14 dairy workers exposed; CDC urges better protections
Related: With Only Gloves To Protect Them, Farmworkers Say They Tend Sick Cows Amid Bird Flu
Herald of woe
Gut health affects most of the rest of health, and there are a lot of links between gut and bone health. In this case, an association has been found between certain changes in the gut microbiome, and subsequent onset of rheumatoid arthritis:
Read in full: Changes in gut microbiome could signal onset of rheumatoid arthritis
Related: Stop Sabotaging Your Gut
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Hearty Healthy Ukrainian Borscht
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In the West, borscht is often thought of as Russian, but it is Ukrainian in origin and popular throughout much of Eastern Europe, with many local variations. Today’s borscht is a vegetarian (and vegan, depending on your choice of cooking fat) borscht from Kyiv, and it’s especially good for the gut, heart, and blood sugars.
You will need
- 1 quart vegetable stock; ideally you made this yourself from vegetable offcuts you kept in the freezer, but failing that, your supermarket should have low-sodium stock cubes
- 4 large beets, peeled and cut into matchsticks
- 1 can white beans (cannellini beans are ideal), drained and rinsed
- 1 cup sauerkraut
- 1 large onion, finely chopped
- 1 green bell pepper, roughly chopped
- 1 large russet potato, peeled and cut into large chunks
- 3 small carrots, tops removed and cut into large chunks
- 1 tbsp tomato paste
- ½ bulb garlic, finely chopped
- 2 tsp black pepper, coarse ground
- 1 bunch fresh dill, chopped. If you cannot get fresh, substitute with parsley (1 bunch fresh, chopped, or 1 tbsp dried). Do not use dried dill; it won’t work.
- A little fat for cooking; this one’s a tricky and personal decision. Butter is traditional, but would make this recipe impossible to cook without going over the recommended limit for saturated fat. Avocado oil is healthy, relatively neutral in taste, and has a high smoke point, though that latter shouldn’t be necessary here if you are attentive with the stirring. Extra virgin olive oil is also a healthy choice, but not as neutral in flavor and does have a lower smoke point. Coconut oil has arguably too strong a taste and a low smoke point. Seed oils are very heart-unhealthy. All in all, avocado oil is a respectable choice from all angles except tradition.
- On standby: a little vinegar (your preference what kind)
Salt is conspicuous by its absence, but there should be enough already from the other ingredients, especially the sauerkraut.
Method
(we suggest you read everything at least once before doing anything)
1) Heat some oil in a large sauté pan (cast iron is perfect if you have it), add the onion and pepper, and stir until the onion is becoming soft.
2) Add the carrots and beets and stir until they are becoming soft. If you need to add a little more oil, that’s fine.
3) Add the tomato paste, and stir in well.
4) Add a little (about ½ cup) of the vegetable stock and stir in well until you get a consistent texture with the tomato paste.
5) Add the sauerkraut and the rest of the broth, and cook for about 20 minutes.
6) Add the potatoes and cook for another 10 minutes.
7) Add the beans and cook for another 5 minutes.
8) Add the garlic, black pepper, and herbs. Check that everything is cooked (poke a chunk of potato with a fork) and that the seasoning is to your liking. The taste should be moderately sour from the sauerkraut; if it is sweet, you can stir in a little vinegar now to correct that.
9) Serve! Ukrainian borscht is most often served hot (unlike Lithuanian borscht, which is almost always served cold), but if the weather’s warm, it can certainly be enjoyed cold too:
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Making Friends With Your Gut (You Can Thank Us Later)
- Eat More (Of This) For Lower Blood Pressure
- No, Beetroot Isn’t Vegetable Viagra. But Here’s What It Can Do
- The Many Health Benefits Of Garlic
- Black Pepper’s Impressive Anti-Cancer Arsenal
Take care!
Share This Post
-
28-Day FAST Start Day-by-Day – by Gin Stephens
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We have previously reviewed Gin Stephens’ other book, “Fast. Feast. Repeat.”, so what’s so special about this one that it deserves reviewing too?
This one is all about troubleshooting the pitfalls that many people find when taking up intermittent fasting.
To be clear: the goal here is not a “28 days and yay you did it, put that behind you now”, but rather “28 days and you are now intermittently fasting easily each day and can keep it up without difficulty”. As for the difficulties that may arise early in the 28 days…
Not just issues of willpower, but also the accidental breaks. For example, some artificial sweeteners, while zero-calorie, trigger an insulin response, which breaks the fast on the metabolic level (avoiding that is the whole point of IF). Lots of little tips like that peppered through the book help the reader to stop accidentally self-sabotaging their progress.
The author does talk about psychological issues too, and also how it will feel different at first while the liver is adapting, than later when it has already depleted its glycogen reserves and the body must burn body fat instead. Information like that makes it easier to understand that some initial problems (hunger, getting “hangry”, feeling twitchy, or feeling light-headed) will last only a few weeks and then disappear.
So, understanding things like that makes a big difference too.
The style of the book is simple and clear pop-science, with lots of charts and bullet points and callout-boxes and the like; it makes for very easy reading, and very quick learning of all the salient points, of which there are many.
Bottom line: if you’ve tried intermittent fasting but struggled to make it stick, this book can help you get to where you want to be.
Share This Post
-
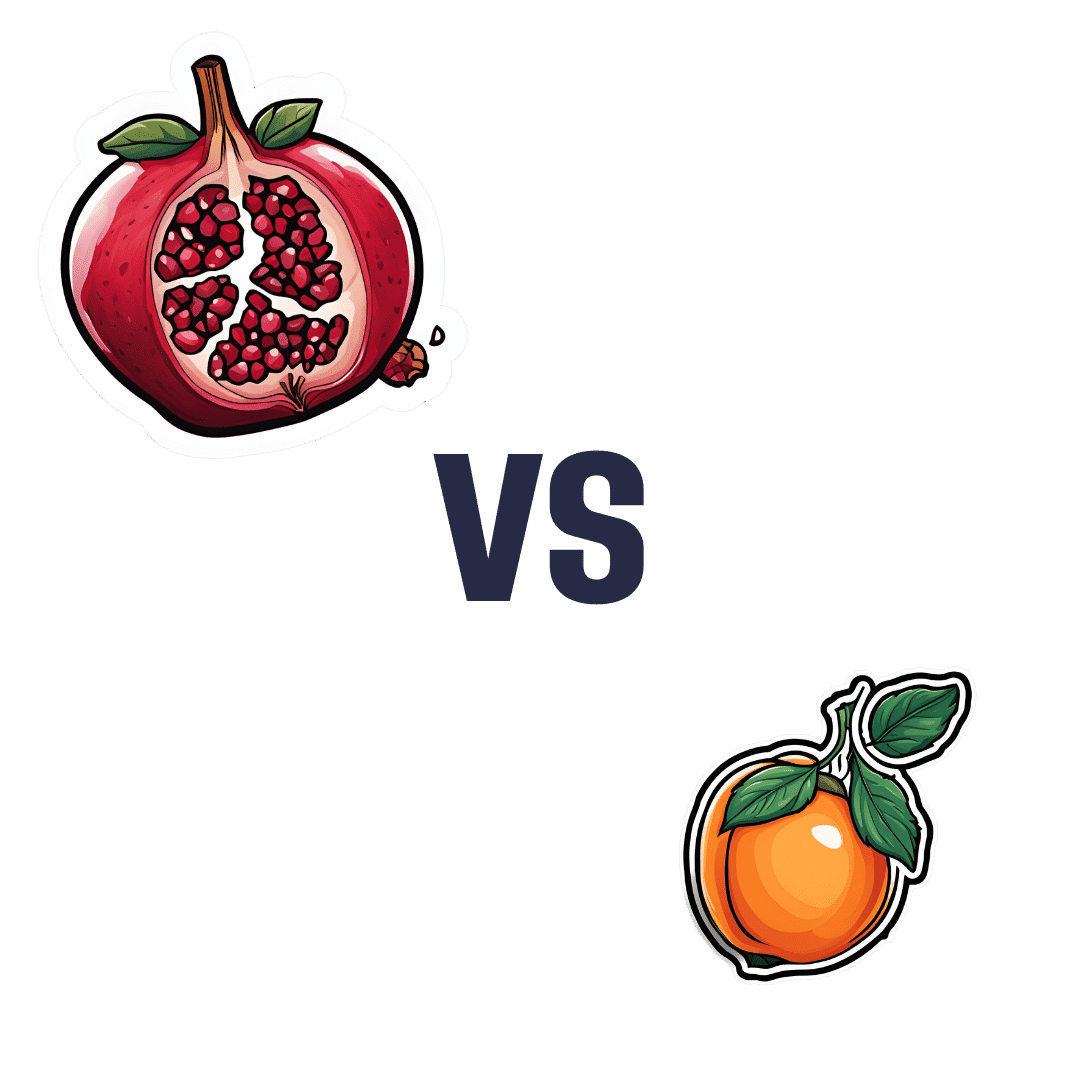
Pomegranate vs Apricot – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing pomegranate to apricot, we picked the pomegranate.
Why?
Both are great! Top tier fruits. But ultimately, pomegranate does have more to offer:
In terms of macros, pomegranate has more protein, carbs, and fiber (and even a little healthy fat—it’s the seeds); the main deciding factor on macros for fruits is almost always the fiber, and that’s the case here, which is why we hand the win to pomegranates in this category.
In the category of vitamins, pomegranates have more of vitamins B1, B2, b5, B6, B7, B9, K, and choline, while apricots have more of vitamins A, B3, and E. A clear win for pomegranates here.
When it comes to minerals, pomegranate has more copper, calcium, magnesium, manganese, phosphorus, selenium, and zinc, while apricots boast just a little more calcium and iron. Another easy win for pomegranates.
Looking at polyphenols, apricots finally win a category, with greater overall polyphenol coverage.
Which is good, but not enough to overcome the other three categories all being in pomegranates’ favor—hence the overall win for pomegranates here!
Of course, the solution is to enjoy both! Diversity is good, for exactly such reasons as this.
Want to learn more?
You might like to read:
Pomegranate’s Health Gifts Are Mostly In Its Peel ← in other words, the one part of the fruit you don’t normally eat. However! It can be dried and ground into a powder supplement, or else made in pomegranate tea.
Enjoy!
Share This Post
Related Posts
-
Optimism Seriously Increases Longevity!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Always look on the bright side for life
❝I’m not a pessimist; I’m a realist!❞
~ every pessimist ever
To believe self-reports, the world is divided between optimists and realists. But how does your outlook measure up, really?
Below, we’ve included a link to a test, and like most free online tests, this is offered “as-is” with the usual caveats about not being a clinical diagnostic tool, this one actually has a fair amount of scientific weight behind it:
❝Empirical testing has indicated the validity of the Optimism Pessimism Instrument as published in the scientific journal Current Psychology: Research and Reviews.
The IDRlabs Optimism/Pessimism Test (IDR-OPT) was developed by IDRlabs. The IDR-OPT is based on the Optimism/Pessimism Instrument (OPI) developed by Dr. William Dember, Dr. Stephanie Martin, Dr. Mary Hummer, Dr. Steven Howe, and Dr. Richard Melton, at the University of Cincinnati.❞
Take This Short (1–2 mins) Test
How did you score? And what could you do to improve on that score?
We said before that we’d do a main feature on this sometime, and today’s the day! Fits with the theme of Easter too, as for those who observe, this is a time for a celebration of hope, new beginnings, and life stepping out of the shadows.
On which note, before we go any further, let’s look at a very big “why” of optimism…
There have been many studies done regards optimism and health, and they generally come to the same conclusion: optimism is simply good for the health.
Here’s an example. It’s a longitudinal study, and it followed 121,700 women (what a sample size!) for eight years. It controlled for all kinds of other lifestyle factors (especially smoking, drinking, diet, and exercise habits, as well as pre-existing medical conditions), so this wasn’t a case of “people who are healthy are more optimistic as a result. And, in the researchers’ own words…
❝We found strong and statistically significant associations of increasing levels of optimism with decreasing risks of mortality, including mortality due each major cause of death, such as cancer, heart disease, stroke, respiratory disease, and infection.
Importantly, findings were maintained after close control for potential confounding factors, including sociodemographic characteristics and depression❞
Read: Optimism and Cause-Specific Mortality: A Prospective Cohort Study
So that’s the why. Now for the how…
Positive thinking is not what you think it is
A lot of people think of “think positive thoughts” as a very wishy-washy platitude, but positive thinking isn’t about ignoring what’s wrong, or burying every negative emotion.
Rather, it is taking advantage of the basic CBT, DBT, and, for that matter, NLP principles:
- Our feelings are driven by our thoughts
- Our thoughts can be changed by how we frame things
This is a lot like the idea that “there’s not such thing as bad weather; only the wrong clothes”. Clearly written by someone who’s never been in a hurricane, but by and large, the principle stands true.
For example…
- Most problems can be reframed as opportunities
- Replace “I have to…” with “I get to…”
- Will the task be arduous? It’ll be all the better looking back on it.
- Did you fail abjectly? Be proud that you lived true to your values anyway.
A lot of this is about focusing on what you can control. If you live your life by your values (first figure out what they are, if you haven’t already), then that will become a reassuring thing that you can always count on, no matter what.
Practice positive self-talk (eliminate the negative)
We often learn, usually as children, to be self deprecatory so as to not appear immodest. While modesty certainly has its place, we don’t have to trash ourselves to do that!
There are various approaches to this, for example:
- Replacing a self-criticism (whether it was true or not) with a neutral or positive statement that you know is true. “I suck at xyz” is just putting yourself down, “Xyz is a challenge for me” asks the question, how will you rise to it?
- Replacing a self-criticism with irony. It doesn’t matter how dripping with sarcasm your inner voice is, the words will still be better. “Glamorous as ever!” after accidentally putting mascara in your eye. “So elegant and graceful!” after walking into furniture. And so on.
Practice radical acceptance
This evokes the “optimistic nihilism” approach to life. It’s perhaps not best in all scenarios, but if you’re consciously and rationally pretty sure something is going to be terrible (and/or know it’s completely outside of your control), acknowledging that possibility (or even, likelihood) cheerfully. Borrowing from the last tip, this can be done with as much irony as you find necessary. For example:
Facing a surgery the recovery from which you know categorically will be very painful: with a big smile “Yep, I am going to be in a lot of pain, so that’s going to be fun!” (fun fact: psychological misery will not make the physical pain any less painful, so you might as well see the funny side) ← see link for additional benefits laughter can add to health-related quality of life)
Plan for the future with love
You know the whole “planting trees in whose shade you’ll never sit”, thing, but: actually for yourself too. Plan (and act!) now, out of love and compassion for your future self.
Simple example: preparing (or semi-preparing, if appropriate) breakfast for yourself the night before, when you know in the morning you’ll be tired, hungry, and/or pressed for time. You’ll wake up, remember that you did that, and…
Tip: at moments like that, take a moment to think “Thanks, past me”. (Or call yourself by your name, whatever works for you. For example I, your writer here, might say to myself “Thanks, past Nastja!”)
This helps to build a habit of gratitude for your past self and love for your future self.
This goes for little things like the above, but it also goes for things whereby there’s much longer-term delayed gratification, such as:
- Healthy lifestyle changes (usually these see slow, cumulative progress)
- Good financial strategies (usually these see slow, cumulative progress)
- Long educational courses (usually these see slow, cumulative progress)
Basically: pay it forward to your future self, and thank yourself later!
Some quick ideas of systems and apps that go hard on the “long slow cumulative progress” approach that you can look back on with pride:
- Noom—nutritional program with a psychology-based approach to help you attain and maintain your goals, long term
- You Need A Budget—we’ve recommended it before and we’ll recommend it again. This is so good. If you click through, you can see a short explanation of what makes it so different to other budgeting apps.
- Duolingo—the famously persistence-motivational language learning app
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Twice-Baked Stuffed Potatoes
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Packed with protein and fiber and dosed with healthy spices, these tasty treats can be enjoyed hot as they are, or cold as part of a salad dinner.
You will need
- 4 large baking potatoes
- 2 cans chickpeas, drained
- 1 can coconut milk
- ½ cup shredded mozzarella cheese, or plant-based alternative
- 1 bulb garlic (sounds like a lot, but this is about three cloves per potato; adjust if you want, though)
- 3 tbsp chopped pickled jalapeños
- 1 tbsp black pepper
- 2 tsp ground cumin
- 2 tsp dried thyme
- 1 tsp onion powder
- Toppings: smoked paprika, finely chopped parsley
Method
(we suggest you read everything at least once before doing anything)
1) Preheat the oven to 400℉ / 200℃.
2) Wash, prick, and bake the potatoes—the latter being for an hour, or until tender.
3) Remove them from the oven and lower the temperature to 350℉ / 175℃.
4) Cut the potatoes lengthways and scoop out the insides into a food processor, leaving enough in the potato that it can hold its shape.
5) Add the remaining ingredients (except the toppings, and half the chickpeas) to the food processor, and blend until smooth.
6) Stuff the filling back into the potato shells (by simple physics of volume, you’ll have a little more than you need, but make it heaped mounds rather than a flat fill-in, and you can probably use most of it, if not all), add the other half of the chickpeas on top and then finally the paprika dusting, and bake for a further 20 minutes.
7) Serve, adding the chopped parsley garnish.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Should You Go Light Or Heavy On Carbs?
- Eat More (Of This) For Lower Blood Pressure
- Level-Up Your Fiber Intake! (Without Difficulty Or Discomfort)
- Our Top 5 Spices: How Much Is Enough For Benefits?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Astaxanthin: Super-Antioxidant & Neuroprotectant
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Think Pink For Brain Health!
Astaxanthin is a carotenoid that’s found in:
- certain marine microalgae
- tiny crustaceans that eat the algae
- fish (and flamingos!) that eat the crustaceans
Yes, it’s the one that makes things pink.
But it does a lot more than that…
Super-antioxidant
Move over, green tea! Astaxanthin has higher antioxidant activity than most carotenoids. For example, it is 2–5 times more effective than alpha-carotene, lutein, beta-carotene, and lycopene:
Antioxidant activities of astaxanthin and related carotenoids
We can’t claim credit for naming it a super-antioxidant though, because:
Astaxanthin: A super antioxidant from microalgae and its therapeutic potential
Grow new brain cells
Axtaxanthin is a neuroprotectant, but that’s to be expected from something with such a powerful antioxidant ability.
What’s more special to astaxanthin is that it assists continued adult neurogenesis (creation of new brain cells):
❝The unique chemical structure of astaxanthin enables it to cross the blood-brain barrier and easily reach the brain, where it may positively influence adult neurogenesis.
Furthermore, astaxanthin appears to modulate neuroinflammation by suppressing the NF-κB pathway, reducing the production of pro-inflammatory cytokines, and limiting neuroinflammation associated with aging and chronic microglial activation.
By modulating these pathways, along with its potent antioxidant properties, astaxanthin may contribute to the restoration of a healthy neurogenic microenvironment, thereby preserving the activity of neurogenic niches during both normal and pathological aging. ❞
That first part is very important, by the way! There are so many things that our brain needs, and we can eat, but the molecules are unable to pass the blood-brain barrier, meaning they either get wasted, or used elsewhere, or dismantled for their constituent parts. In this case, it zips straight into the brain instead.
See also:
How To Grow New Brain Cells (At Any Age)
(Probably) good for the joints, too
First, astaxanthin got a glowing report in a study we knew not to trust blindly:
…and breathe. What a title that was! But, did you catch why it’s not to be trusted blindly? It was down at the bottom…
❝Conflict of interest statement
NOVAREX Co., Ltd. funded the study. Valensa International provided the FlexPro MD® ingredients, and NOVAREX Co., Ltd. encapsulated the test products (e.g., both FlexPro MD® and placebo)❞
Studies where a supplement company funded the study are not necessarily corrupt, but they can certainly sway publication bias, i.e. the company funds a bunch of studies and then pulls funding from the ones that aren’t going the way it wants.
So instead let’s look at:
Astaxanthin attenuates joint inflammation induced by monosodium urate crystals
and
Astaxanthin ameliorates cartilage damage in experimental osteoarthritis
…which had no such conflicts of interest.
They agree that astaxanthin indeed does the things (attenuates joint inflammation & ameliorates cartilage damage).
However, they are animal studies (rats), so we’d like to see studies with humans to be able to say for sure how much it helps these things.
Summary of benefits
Based on the available research, astaxanthin…
- is indeed a super-antioxidant
- is a neuroprotective agent
- also assists adult neurogenesis
- is probablygood for joints too
How much do I take, and is it safe?
A 2019 safety review concluded:
❝Recommended or approved doses varied in different countries and ranged between 2 and 24 mg.
We reviewed 87 human studies, none of which found safety concerns with natural astaxanthin supplementation, 35 with doses ≥12 mg/day.❞
Source: Astaxanthin: How much is too much? A safety review
In short: for most people, it’s very safe and well-tolerated. If you consume it to an extreme, you will likely turn pink, much as you would turn orange if you did the same thing with carrots. But aside from that, the risks appear to be minimal.
However! If you have a seafood allergy, please take care to get a supplement that’s made from microalgae, not one that’s made from krill or other crustaceans, or from other creatures that eat those.
Where can I get it?
We don’t sell it, but here’s an example product on Amazon, for your convenience
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: