Invigorating Sabzi Khordan
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Have you ever looked at the nutritional values and phytochemical properties of herbs, and thought “well that’s all well and good, but we only use a tiny amount”? Sabzi khordan is a herb-centric traditional Levantine sharing platter served most commonly as an appetizer, and it is indeed appetizing! Never again will “start your meal with a green salad to ensure a gentle blood sugar curve” seem like a chore:
You will need
- Large bunch of parsley
- Small bunch of tarragon leaves
- Small bunch of basil leaves
- Small bunch of mint
- Small bunch of sorrel leaves
- 7 oz block of feta cheese (if vegan, a plant-based substitution is fine in culinary terms, but won’t have the same gut-healthy benefits, as plant-based cheeses are not fermented)
- 9 oz labneh-stuffed vine leaves in olive oil (if vegan, same deal as the above, except it’s harder to find plant-based substitutes for labneh (strained yogurt cheese), so you might want to use our Plant-Based Healthy Cream Cheese recipe instead and make your own)
- 2 tbsp za’atar (you can make your own by blending dried hyssop, dried sumac berries, sesame seeds, dried thyme, and salt—but if you haven’t had za’atar before, we recommend first buying some like the one that we linked, so that next time you know what you’re aiming for)
- 3 tbsp extra virgin olive oil
- 10 radishes
- 6 scallions
- 9 oz walnuts, soaked in water overnight and drained
- 1 cucumber, cut into batons
- Warm flatbreads (you can use our Healthy Homemade Flatbreads recipe)
Method
(we suggest you read everything at least once before doing anything)
1) Arrange the feta, labneh, za’atar, and olive oil in separate little serving dishes.
2) Arrange everything else around them on a platter.
3) Serve! You may be thinking: did we really need a recipe to tell us “put the things on a plate”? The answer here is that this one today was shared mostly as a matter of inspiration, because when was the last time you thought to serve herbs as the star of the dish? Plus, it’s an excuse to try za’atar, not something so commonly seen outside of the Levant.

An alternative presentation
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Herbs for Evidence-Based Health & Healing
- Making Friends With Your Gut (You Can Thank Us Later)
- 10 Ways To Balance Blood Sugars
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How to be kind to yourself (without going to a day spa)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
“I have to be hard on myself,” Sarah told me in a recent telehealth psychology session. “I would never reach my potential if I was kind and let myself off the hook.”
I could empathise with this fear of self-compassion from clients such as Sarah (not her real name). From a young age, we are taught to be kind to others, but self-kindness is never mentioned.
Instead, we are taught success hinges on self-sacrifice. And we need a healthy inner critic to bully us forward into becoming increasingly better versions of ourselves.
But research shows there doesn’t have to be a trade-off between self-compassion and success.
Self-compassion can help you reach your potential, while supporting you to face the inevitable stumbles and setbacks along the way.
What is self-compassion?
Self-compassion has three key ingredients.
1. Self-kindness
This involves treating yourself with the same kindness you would extend towards a good friend – via your thoughts, feelings and actions – especially during life’s difficult moments.
For instance, if you find yourself fixating on a minor mistake you made at work, self-kindness might involve taking a ten-minute walk to shift focus, and reminding yourself it is OK to make mistakes sometimes, before moving on with your day.
2. Mindfulness
In this context, mindfulness involves being aware of your own experience of stress or suffering, rather than repressing or avoiding your feelings, or over-identifying with them.
Basically, you must see your stress with a clear (mindful) perspective before you can respond with kindness. If we avoid or are consumed by our suffering, we lose perspective.
3. Common humanity
Common humanity involves recognising our own experience of suffering as something that unites us as being human.
For instance, a sleep-deprived parent waking up (for the fourth time) to feed their newborn might choose to think about all the other parents around the world doing exactly the same thing – as opposed to feeling isolated and alone.
It’s not about day spas, or booking a manicure
When Sarah voiced her fear that self-compassion would prevent her success, I explained self-compassion is distinct from self-indulgence.
“So is self-compassion just about booking in more mani/pedis?” Sarah asked.
Not really, I explained. A one-off trip to a day spa is unlikely to transform your mental health.
Instead, self-compassion is a flexible psychological resilience factor that shapes our thoughts, feelings and actions.
It’s associated with a suite of benefits to our wellbeing, relationships and health.
A one-off trip to a day spa is unlikely to transform your mental health.
baranq/ShutterstockWhat does the science say?
Over the past 20 years, we’ve learned self-compassionate people enjoy a wide range of benefits. They tend to be happier and have fewer psychological symptoms of distress.
Those high on self-compassion persevere following a failure. They say they are more motivated to overcome a personal weakness than those low on self-compassion, who are more likely to give up.
So rather than feeling trapped by your inadequacies, self-compassion encourages a growth mindset, helping you reach your potential.
However, self-compassion is not a panacea. It will not change your life circumstances or somehow make life “easy”. It is based on the premise that life is hard, and provides practical tools to cope.
It’s a factor in healthy ageing
I research menopause and healthy ageing and am especially interested in the value of self-compassion through menopause and in the second half of life.
Because self-compassion becomes important during life’s challenges, it can help people navigate physical symptoms (for instance, menopausal hot flushes), life transitions such as divorce, and promote healthy ageing.
I’ve also teamed up with researchers at Autism Spectrum Australia to explore self-compassion in autistic adults.
We found autistic adults report significantly lower levels of self-compassion than neurotypical adults. So we developed an online self-compassion training program for this at-risk population.
Three tips for self-compassion
You can learn self-compassion with these three exercises.
1. What would you say to a friend?
Think back to the last time you made a mistake. What did you say to yourself?
If you notice you’re treating yourself more like an enemy than a friend, don’t beat yourself up about it. Instead, try to think about what you might tell a friend, and direct that same friendly language towards yourself.
2. Harness the power of touch
Soothing human touch activates the parasympathetic “relaxation” branch of our nervous system and counteracts the fight or flight response.
Specifically, self-soothing touch (for instance, by placing both hands on your heart, stroking your forearm or giving yourself a hug) reduces cortisol responses to psychosocial stress.
Yes, hugging yourself can help.
http://krakenimages.com/Shutterstock3. What do I need right now?
Sometimes, it can be hard to figure out exactly what self-compassion looks like in a given moment. The question “what do I need right now” helps clarify your true needs.
For example, when I was 37 weeks pregnant, I woke up bolt awake one morning at 3am.
Rather than beating myself up about it, or fretting about not getting enough sleep, I gently placed my hands on my heart and took a few deep breaths. By asking myself “what do I need right now?” it became clear that listening to a gentle podcast/meditation fitted the bill (even though I wanted to addictively scroll my phone).
Lydia Brown, Senior Lecturer in Psychology, The University of Melbourne
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
How To Avoid Age-Related Macular Degeneration
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Avoiding Age-Related Macular Degeneration
Eye problems can strike at any age, but as we get older, it becomes a lot more likely. In particular, age-related macular degeneration is, as the name suggests, an age-bound disease.
Is there no escaping it, then?
The risk factors for age-related macular degeneration are as follows:
- Being over the age of 55 (can’t do much about this one)
- Being over the age of 65 (risk climbs sharply now)
- Having a genetic predisposition (can’t do much about this one)
- Having high cholesterol (this one we can tackle)
- Having cardiovascular disease (this one we can tackle)
- Smoking (so, just don’t)
Genes predispose; they don’t predetermine. Or to put it another way: genes load the gun, but lifestyle pulls the trigger.
Preventative interventions against age-related macular degeneration
Prevention is better than a cure in general, and this especially goes for things like age-related macular degeneration, because the most common form of it has no known cure.
So first, look after your heart (because your heart feeds your eyes).
See also: The Mediterranean Diet
Next, eat to feed your eyes specifically. There’s a lot of research to show that lutein helps avoid age-related diseases in the eyes and the rest of the brain, too:
See also: Brain Food? The Eyes Have It
Do supplements help?
They can! There was a multiple-part landmark study by the National Eye Institute, a formula was developed that reduced the 5-year risk of intermediate disease progressing to late disease by 25–30%. It also reduced the risk of vision loss by 19%.
You can read about both parts of the study here:
Age-Related Eye Disease Studies (AREDS/AREDS2): major findings
As you can see, an improvement was made between the initial study and the second one, by replacing beta-carotene with lutein and zeaxanthin.
The AREDS2 formula contains:
- 500 mg vitamin C
- 180 mg vitamin E
- 80 mg zinc
- 10 mg lutein
- 2 mg copper
You can learn more about these supplements, and where to get them, here on the NEI’s corner of the official NIH website:
AREDS 2 Supplements for Age-Related Macular Degeneration
Take care of yourself!
Share This Post
-
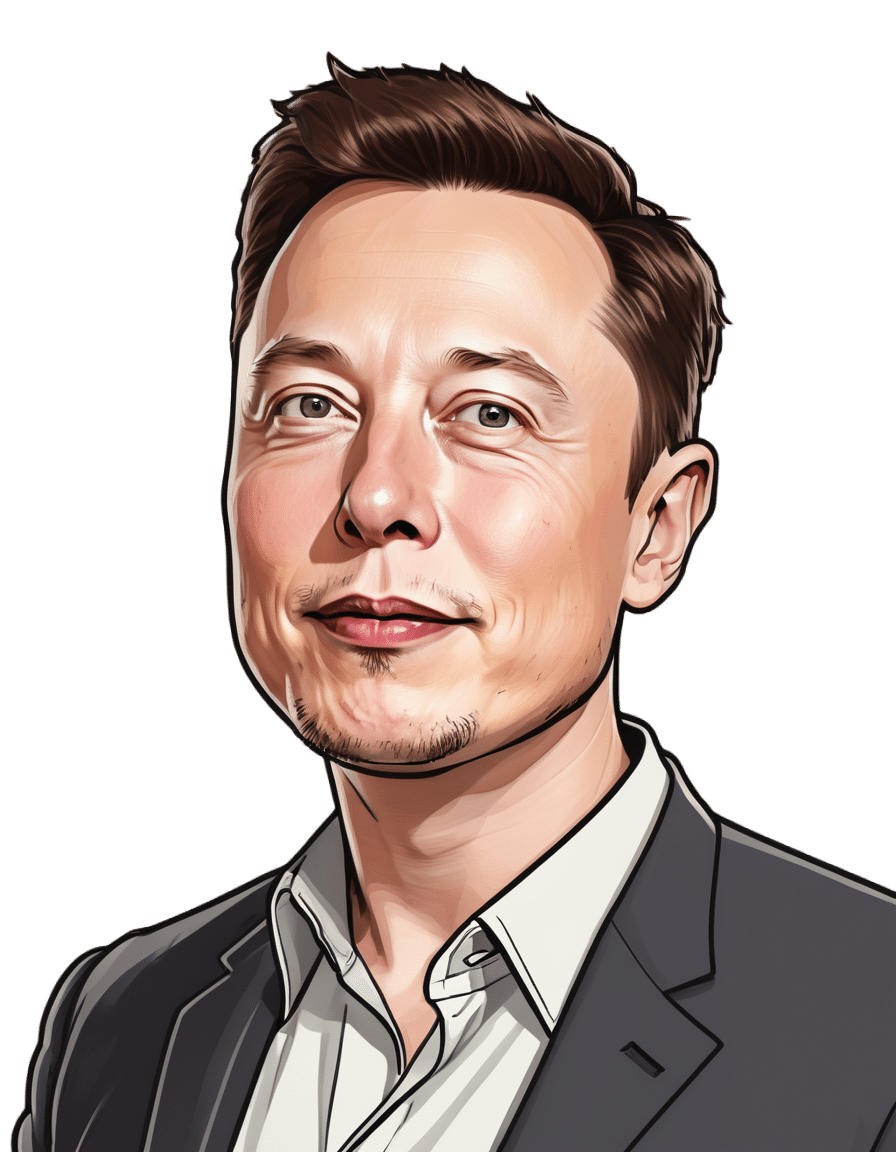
Elon Musk says ‘disc replacement’ worked for him. But evidence this surgery helps chronic pain is lacking
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Last week in a post on X, owner of the platform Elon Musk recommended people look into disc replacement if they’re experiencing severe neck or back pain.
According to a biography of the billionaire, he’s had chronic back and neck pain since he tried to “judo throw” a 350-pound sumo wrestler in 2013 at a Japanese-themed party for his 42nd birthday, and blew out a disc at the base of his neck.
In comments following the post, Musk said the surgery was a “gamechanger” and reduced his pain significantly.
Musk’s original post has so far had more than 50 million views and generated controversy. So what is disc replacement surgery and what does the evidence tells us about its benefits and harms?
What’s involved in a disc replacement?
Disc replacement is a type of surgery in which one or more spinal discs (a cushion between the spine bones, also known as vertebrae) are removed and replaced with an artificial disc to retain movement between the vertebrae. Artificial discs are made of metal or a combination of metal and plastic.
Disc replacement may be performed for a number of reasons, including slipped discs in the neck, as appears to be the case for Musk.
Disc replacement is major surgery. It requires general anaesthesia and the operation usually takes 2–4 hours. Most people stay in hospital for 2–7 days. After surgery patients can walk but need to avoid things like strenuous exercise and driving for 3–6 weeks. People may be required to wear a neck collar (following neck surgery) or a back brace (following back surgery) for about 6 weeks.
Costs vary depending on whether you have surgery in the public or private health system, if you have private health insurance, and your level of coverage if you do. In Australia, even if you have health insurance, a disc replacement surgery may leave you more than A$12,000 out of pocket.
Disc replacement surgery is not performed as much as other spinal surgeries (for example, spinal fusion) but its use is increasing.
In New South Wales for example, rates of privately-funded disc replacement increased six-fold from 6.2 per million people in 2010–11 to 38.4 per million in 2019–20.
What are the benefits and harms?
People considering surgery will typically weigh that option against not having surgery. But there has been very little research comparing disc replacement surgery with non-surgical treatments.
Clinical trials are the best way to determine if a treatment is effective. You first want to show that a new treatment is better than doing nothing before you start comparisons with other treatments. For surgical procedures, the next step might be to compare the procedure to non-surgical alternatives.
Unfortunately, these crucial first research steps have largely been skipped for disc replacement surgery for both neck and back pain. As a result, there’s a great deal of uncertainty about the treatment.
There are no clinical trials we know of investigating whether disc replacement is effective for neck pain compared to nothing or compared to non-surgical treatments.
For low back pain, the only clinical trial that has been conducted to our knowledge comparing disc replacement to a non-surgical alternative found disc replacement surgery was slightly more effective than an intensive rehabilitation program after two years and eight years.
Many people experience chronic pain. Yan Krukau/Pexels Complications are not uncommon, and can include disclocation of the artificial disc, fracture (break) of the artificial disc, and infection.
In the clinical trial mentioned above, 26 of the 77 surgical patients had a complication within two years of follow up, including one person who underwent revision surgery that damaged an artery leading to a leg needing to be amputated. Revision surgery means a re-do to the primary surgery if something needs fixing.
Are there effective alternatives?
The first thing to consider is whether you need surgery. Seeking a second opinion may help you feel more informed about your options.
Many surgeons see disc replacement as an alternative to spinal fusion, and this choice is often presented to patients. Indeed, the research evidence used to support disc replacement mainly comes from studies that compare disc replacement to spinal fusion. These studies show people with neck pain may recover and return to work faster after disc replacement compared to spinal fusion and that people with back pain may get slightly better pain relief with disc replacement than with spinal fusion.
However, spinal fusion is similarly not well supported by evidence comparing it to non-surgical alternatives and, like disc replacement, it’s also expensive and associated with considerable risks of harm.
Fortunately for patients, there are new, non-surgical treatments for neck and back pain that evidence is showing are effective – and are far cheaper than surgery. These include treatments that address both physical and psychological factors that contribute to a person’s pain, such as cognitive functional therapy.
While Musk reported a good immediate outcome with disc replacement surgery, given the evidence – or lack thereof – we advise caution when considering this surgery. And if you’re presented with the choice between disc replacement and spinal fusion, you might want to consider a third alternative: not having surgery at all.
Giovanni E Ferreira, NHMRC Emerging Leader Research Fellow, Institute of Musculoskeletal Health, University of Sydney; Christine Lin, Professor, Institute for Musculoskeletal Health, University of Sydney; Christopher Maher, Professor, Sydney School of Public Health, University of Sydney; Ian Harris, Professor of Orthopaedic Surgery, UNSW Sydney, and Joshua Zadro, NHMRC Emerging Leader Research Fellow, University of Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
Greek Yogurt vs Cottage Cheese – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing Greek yogurt to cottage cheese, we picked the yogurt.
Why?
These are both dairy products popularly considered healthy, mostly for their high-protein, low-carb, low-fat profile. We’re going to assume that both were made without added sugars. Thus, their macro profiles are close to identical, and nothing between them there.
In the category of vitamins, both are a good source of some B vitamins, and neither are good source of much else. The B-vitamins they have most of, B2 and B12, Greek yogurt has more.
We’ll call this a small win for Greek yogurt.
As they are dairy products, you might have expected them to contain vitamin D—however (unless they have been artificially fortified, as is usually done with plant-based equivalents) they contain none or trace amounts only.
When it comes to minerals, both are reasonable sources of calcium, selenium, and phosphorus. Of these, they’re equal on the selenium, while cottage cheese has more phosphorus and Greek yogurt has more calcium.
Since it’s also a mineral (even if it’s usually one we’re more likely to be trying to get less of), it’s also worth noting here that cottage cheese is quite high in sodium, while Greek yogurt is not.
Another win for Greek yogurt.
Beyond those things, we’d be remiss not to mention that Greek yogurt contains plenty of probiotic bacteria, while cottage cheese does not.
Want to learn more?
You might like to read:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Statins and Brain Fog?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝I was wondering if you had done any info about statins. I’ve tried 3, and keep quitting them because they give me brain fog. Am I imagining this as the research suggests?❞
If you are female, the chances of adverse side-effects are a lot higher:
As an extra kicker, not only are the adverse side-effects more likely for women, but also, the benefits are often less beneficial, too (see the above main feature for some details).
That’s not to say that statins can’t have their place for women; sometimes it will still be the right choice. Just, not as readily so as for men.
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Is Air-Fried Food Really Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Air-frying has a reputation for being healthy—and it generally is, provided it’s used carefully:
Just one thing to watch out for
An air-fryer is basically a small convection oven that uses circulating air rather than immersion in oil to cook food. The smallness of an air-fryer is a feature not a bug—if you get an air-fryer over a certain size, then congratulations, you just have a convection oven. The small size it what helps it to cook so efficiently. This is one reason that they’re not really used in industrial settings.
The documentary-makers from this video had their food (chicken, fish, and fries) lab-tested (for fat, cholesterol, and acrylamide), and found:
- Air-frying significantly reduced saturated fat (38–53%) and trans fats (up to 55%) in some foods.
- Cholesterol reduction varied depending on the food type.
- Acrylamide levels in air-fried potatoes were much higher due to cooking time and temperature.
About that acrylamide: acrylamide forms in starchy foods at high temperatures and may pose cancer risks (the research is as yet unclear, with conflicting evidence). Air-frying can cause higher acrylamide levels if cooking is prolonged or temperatures are too high.
Recommendations to reduce acrylamide:
- Soak potatoes before cooking.
- Use lower temperatures (e.g. 180℃/350℉) and shorter cooking times.
- Avoid over-browning food.
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Unlock Your Air-Fryer’s Potential!
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: