What is type 1.5 diabetes? It’s a bit like type 1 and a bit like type 2 – but it’s often misdiagnosed
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
While you’re likely familiar with type 1 and type 2 diabetes, you’ve probably heard less about type 1.5 diabetes.
Also known as latent autoimmune diabetes in adults (LADA), type 1.5 diabetes has features of both type 1 and type 2 diabetes.
More people became aware of this condition after Lance Bass, best known for his role in the iconic American pop band NSYNC, recently revealed he has it.
So, what is type 1.5 diabetes? And how is it diagnosed and treated?

There are several types of diabetes
Diabetes mellitus is a group of conditions that arise when the levels of glucose (sugar) in our blood are higher than normal. There are actually more than ten types of diabetes, but the most common are type 1 and type 2.
Type 1 diabetes is an autoimmune condition where the body’s immune system attacks and destroys the cells in the pancreas that make the hormone insulin. This leads to very little or no insulin production.
Insulin is important for moving glucose from the blood into our cells to be used for energy, which is why people with type 1 diabetes need insulin medication daily. Type 1 diabetes usually appears in children or young adults.
Type 2 diabetes is not an autoimmune condition. Rather, it happens when the body’s cells become resistant to insulin over time, and the pancreas is no longer able to make enough insulin to overcome this resistance. Unlike type 1 diabetes, people with type 2 diabetes still produce some insulin.
Type 2 is more common in adults but is increasingly seen in children and young people. Management can include behavioural changes such as nutrition and physical activity, as well as oral medications and insulin therapy.

How does type 1.5 diabetes differ from types 1 and 2?
Like type 1 diabetes, type 1.5 occurs when the immune system attacks the pancreas cells that make insulin. But people with type 1.5 often don’t need insulin immediately because their condition develops more slowly. Most people with type 1.5 diabetes will need to use insulin within five years of diagnosis, while those with type 1 typically require it from diagnosis.
Type 1.5 diabetes is usually diagnosed in people over 30, likely due to the slow progressing nature of the condition. This is older than the typical age for type 1 diabetes but younger than the usual diagnosis age for type 2.
Type 1.5 diabetes shares genetic and autoimmune risk factors with type 1 diabetes such as specific gene variants. However, evidence has also shown it may be influenced by lifestyle factors such as obesity and physical inactivity which are more commonly associated with type 2 diabetes.
What are the symptoms, and how is it treated?
The symptoms of type 1.5 diabetes are highly variable between people. Some have no symptoms at all. But generally, people may experience the following symptoms:
- increased thirst
- frequent urination
- fatigue
- blurred vision
- unintentional weight loss.
Typically, type 1.5 diabetes is initially treated with oral medications to keep blood glucose levels in normal range. Depending on their glucose control and the medication they are using, people with type 1.5 diabetes may need to monitor their blood glucose levels regularly throughout the day.
When average blood glucose levels increase beyond normal range even with oral medications, treatment may progress to insulin. However, there are no universally accepted management or treatment strategies for type 1.5 diabetes.

Type 1.5 diabetes is often misdiagnosed
Lance Bass said he was initially diagnosed with type 2 diabetes, but later learned he actually has type 1.5 diabetes. This is not entirely uncommon. Estimates suggest type 1.5 diabetes is misdiagnosed as type 2 diabetes 5–10% of the time.
There are a few possible reasons for this.
First, accurately diagnosing type 1.5 diabetes, and distinguishing it from other types of diabetes, requires special antibody tests (a type of blood test) to detect autoimmune markers. Not all health-care professionals necessarily order these tests routinely, either due to cost concerns or because they may not consider them.
Second, type 1.5 diabetes is commonly found in adults, so doctors might wrongly assume a person has developed type 2 diabetes, which is more common in this age group (whereas type 1 diabetes usually affects children and young adults).
Third, people with type 1.5 diabetes often initially make enough insulin in the body to manage their blood glucose levels without needing to start insulin medication. This can make their condition appear like type 2 diabetes, where people also produce some insulin.
Finally, because type 1.5 diabetes has symptoms that are similar to type 2 diabetes, it may initially be treated as type 2.
We’re still learning about type 1.5
Compared with type 1 and type 2 diabetes, there has been much less research on how common type 1.5 diabetes is, especially in non-European populations. In 2023, it was estimated type 1.5 diabetes represented 8.9% of all diabetes cases, which is similar to type 1. However, we need more research to get accurate numbers.
Overall, there has been a limited awareness of type 1.5 diabetes and unclear diagnostic criteria which have slowed down our understanding of this condition.
A misdiagnosis can be stressful and confusing. For people with type 1.5 diabetes, being misdiagnosed with type 2 diabetes might mean they don’t get the insulin they need in a timely manner. This can lead to worsening health and a greater likelihood of complications down the road.
Getting the right diagnosis helps people receive the most appropriate treatment, save money, and reduce diabetes distress. If you’re experiencing symptoms you think may indicate diabetes, or feel unsure about a diagnosis you’ve already received, monitor your symptoms and chat with your doctor.
Emily Burch, Accredited Practising Dietitian and Lecturer, Southern Cross University and Lauren Ball, Professor of Community Health and Wellbeing, The University of Queensland
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Black Bean Burgers With Guacamole
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Once again proving that burgers do not have to be unhealthy, this one’s a nutritional powerhouse full of protein, fiber, vitamins, and minerals, as well as healthy fats and extra health-giving spices.
You will need
- 1 can black beans, drained and rinsed (or 1 cup same, cooked, drained, and rinsed)
- 3 oz walnuts (if allergic, substitute with pumpkin seeds)
- 1 tbsp chia seeds
- 1 tbsp flax seeds
- ½ red onion, finely chopped
- 1 small eggplant, diced small (e.g. ½” cubes or smaller)
- 1 small carrot, grated
- 3 tbsp finely chopped cilantro (or if you have the “this tastes like soap” gene, then substitute with parsley)
- 1 tbsp lemon juice
- 1 jalapeño pepper, finely chopped (adjust per heat preferences)
- ¼ bulb garlic, crushed
- 2 tsp black pepper
- 1 tsp smoked paprika
- 1 tsp cayenne pepper (adjust per heat preferences)
- ½ tsp MSG or 1 tsp low-sodium salt
- Burger buns (you can use our Delicious Quinoa Avocado Bread recipe if you like)
For the guacamole:
- 1 large ripe avocado, pitted, skinned, and chopped
- 1 tbsp lime juice
- 1 tomato, finely chopped
- ¼ red onion, finely chopped
- ¼ bulb garlic, crushed
- 1 tsp red chili pepper flakes (adjust per heat preferences)
Method
(we suggest you read everything at least once before doing anything)
1) Process the walnuts, chia seeds, and flax seeds in a food processor/blender, until they become a coarse mixture. Set aside.
2) Heat a little oil in a skillet, and fry the red onion, aubergine, and carrot for 5 minutes stirring frequently, then add the garlic and jalapeño and stir for a further 1 minute. Set aside.
3) Combine both mixtures you set aside with the rest of the ingredients from the burger section of the recipe, except the buns, and process them in the food processor on a low setting if possible, until you have a coarse mixture—you still want some texture, not a paste.
4) Shape into patties; this recipe gives for 4 large patties or 8 small ones. When you’ve done this, put them in the fridge for at least 30 minutes, to firm up.
5) While you wait, make the guacamole by mashing the avocado with the lime juice, and then stirring into the onion, tomato, garlic, and pepper.
6) Cook the patties; you can do this on the grill, in a skillet, or in the oven, per your preference. Grilling or frying should take about 5 minutes on each side, give or take the size and shape of the patties. Baking in the oven should take 20–30 minutes at 400℉ / 200℃ turning over halfway through, but keep an eye on them, because again, the size and shape of the patties will affect this. You may be wondering: aren’t they all going to be patty-shaped? And yes, but for example a wide flat patty will cook more quickly than the same volume of burger mixture in a taller less wide patty.
7) Assemble! We recommend the order: bottom bun, guacamole, burger patty, any additional toppings you want to add (e.g. more salad, pickles, etc), top bun:
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Level-Up Your Fiber Intake! (Without Difficulty Or Discomfort)
- Chickpeas vs Black Beans – Which is Healthier?
- Kidney Beans or Black Beans – Which is Healthier?
- Coconut vs Avocado – Which is Healthier?
- Our Top 5 Spices: How Much Is Enough For Benefits?
Take care!
Share This Post
-
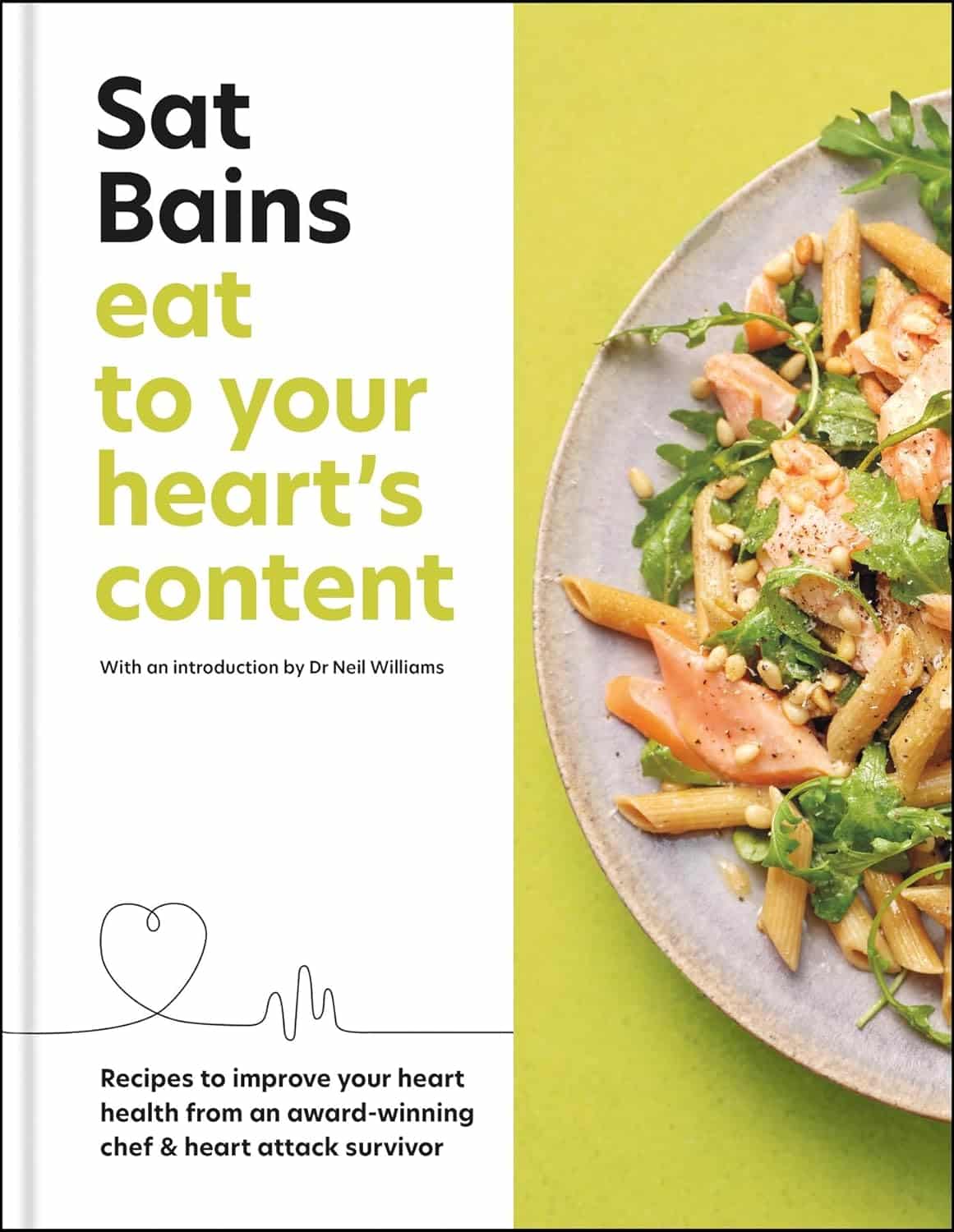
Eat to Your Heart’s Content – by Dr. Sat Bains
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Making food heart-healthy and tasty is a challenge that vexes many, but it doesn’t have to be so difficult.
Dr. Sat Bains, a professional chef with multiple Michelin stars to his name, is an expert on “tasty”, and after surviving a heart attack himself, he’s become an expert on “heart-healthy” since then.
The book contains not only the recipes (of which there are 68, by the way), but also large sections of explanation of what makes various ingredients or methods heart-healthy or heart-unhealthy.
There’s science in there too, and these sections were written under the guidance of Dr. Neil Williams, a lecturer in physiology and nutrition.
You may be wondering as to why the author himself has a doctorate too; in fact he has three, none of which are relevant:
- Doctor of Arts
- Doctor of Laws
- Doctor of Hospitality (Honorary)
…but we prefix “Dr.” when people are that and he is that. The expertise we’re getting here though is really his culinary skill and extracurricular heart-healthy learning, plus Dr. Williams’ actual professional health guidance.
Bottom line: if you’d like heart-healthy recipes with restaurant-level glamour, this book is a fine choice.
Click here to check out Eat To Your Heart’s Content, and look after yours!
Share This Post
-
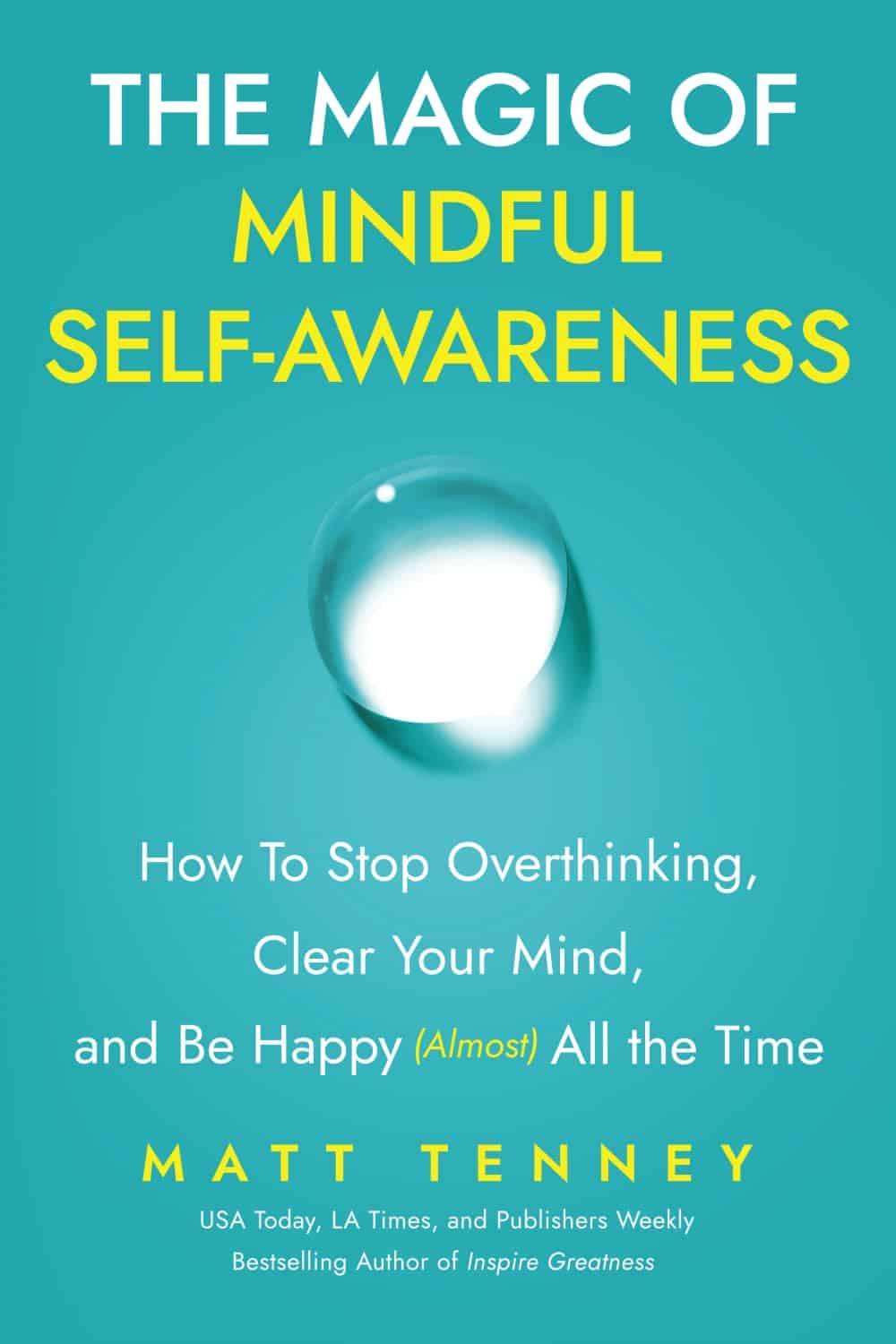
The Magic Of Mindful Self-Awareness − by Matt Tenny
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
As the author is not a Dr. Matt Tenny, you may wonder his qualifications. In this case, the answer is summed up in the title of the first part of the book, “How I discovered unconditional happiness on my journey from prisoner to monk to social entrepreneur”. In other words, this one’s about personal experience of changing his life considerably.
Part two, however, is where the actual practical content starts, with such topics as:
- How to be free from your thoughts so you can stop overthinking and enjoy the present moment
- How to clear your mind and make the practice of self-awareness (almost) effortless
- How to transform mundane activities into magical moments and be happy 95% of the time
You may be wondering about the other 5%; i.e. will this not work for some things? The answer is rather that sometimes we will experience emotions that are considered negative, and that’s ok. It need not be much of the time, but if we didn’t experience them at all, we’d just normalize a new set point and consider the least enjoyable 5% of that to be negative.
And indeed, part three is “how to be at peace during the 5% of life that is truly painful, and live a deeply meaningful life”.
Which, honestly, is a very important life skill, and this alone is worth the price of the book if you don’t already have this skill (and if you do, then condolences for however you got it, but congratulations on having it).
The style is quite personal and direct, and—unlike that of a lot of CEO-monk types—surprisingly down-to-earth and (actually!) mindfully self-aware.
Bottom line: if you’d like to be at peace in life with more practical advice than just “practice some mindfulness meditation”, then this book could be just the turning point you need.
Share This Post
Related Posts
-
Does This New Machine Cure Depression?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Let us first talk briefly about the slightly older tech that this may replace, transcranial magnetic stimulation (TMS).
TMS involves electromagnetic fields to stimulate the left half of the brain and inhibit the right half of the brain. It sounds like something from the late 19th century—“cure your melancholy with the mystical power of magnetism”—but the thing is, it works:
The main barriers to its use are that the machine itself is expensive, and it has to be done in a clinic by a trained clinician. Which, if it were treating one’s heart, say, would not be so much of an issue, but when treating depression, there is a problem that depressed people are not the most likely to commit to (and follow through with) going somewhere probably out-of-town regularly to get a treatment, when merely getting out of the door was already a challenge and motivation is thin on the ground to start with.
Thus, antidepressant medications are more often the go-to for cost-effectiveness and adherence. Of course, some will work better than others for different people, and some may not work at all in the case of what is generally called “treatment-resistant depression”:
Antidepressants: Personalization Is Key!
Transcranial stimulation… At home?
Move over transcranial magnetic stimulation; it’s time for transcranial direct-current stimulation (tDCS).
First, what it’s not: electroconvulsive therapy (ECT). Rather, it uses a very low current.
What it is: a small and portable headset (as opposed to the big machine to go sit in for TMS) that one can use at home. Here’s an example product on Amazon, though there are more stylish versions around, this is the same basic technology.
In a recent study, 45% of those who received treatment with this device experienced remission in 10 weeks, significantly beating placebo (bearing in mind that placebo effect is strongest when it comes to invisible ailments such as depression).
See also: How To Leverage Placebo Effect For Yourself ← this explains more about how the placebo effect works, to the extent that it can even be an adjuvant tool to augment “real” therapies
And as for the study, here it is:
…which rather cuts through the “depressed people don’t make it to the clinic consistently, if at all” problem. Of course, it still requires adherence to its use at home, for example three 30-minute sessions per week, but honestly, “lie/sit still” is likely within the abilities of the majority of depressed people. However…
Important note: you remember we said “in 10 weeks”? That may be critical, because shorter studies (e.g. 6 weeks) have previously returned without such glowing results:
Home-Use Transcranial Direct Current Stimulation for the Treatment of a Major Depressive Episode
This means that if you get this tech for yourself or a loved one, it’ll be necessary to persist for likely 10 weeks, certainly more than 6 weeks, and not abandon it after a few sessions when it hasn’t been life-changing yet. And that may be more of a challenge for a depressed person, so likely an “accountability buddy” of some kind is in order (partner, close friend, etc) to help ensure adherence and generally bug you/them into doing it consistently.
And then, of course, you/they might still be in the 55% of people for whom it didn’t work. And that does suck, but random antidepressant medications (i.e., not personalized) don’t fare much better, statistically.
Want something else against depression meanwhile?
Here are some strategies that not only can significantly help, but also are tailored to be actually doable while depressed:
The Mental Health First-Aid You’ll Hopefully Never Need ← written by your writer who has previously suffered extensively from depression and knows what it is like
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Cabbage vs Kale – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing cabbage to kale, we picked the kale.
Why?
Here we go again, pitting Brassica oleracea vs Brassica oleracea. One species, many cultivars! Notwithstanding being the same species, there are important nutritional differences:
In terms of macros, kale has more protein, carbs, and fiber, and even has the lower glycemic index, not that cabbage is bad at all, of course. But nominally, kale gets the win on all counts in this category.
In the category of vitamins, cabbage has more of vitamins B5 and choline, while kale has more of vitamins A, B1, B2, B3, B6, B7, B9, C, E, and K. An easy win for kale!
When it comes to minerals, it’s even more decisive: cabbage is not higher in any minerals, while kale has more calcium, copper, iron, magnesium, manganese, phosphorus, potassium, and zinc. Another clear win for kale.
Adding up the sections makes it very clear that kale wins the day, but we’d like to mention that cabbage was good in all of these metrics too; kale was just better!
Want to learn more?
You might like to read:
21 Most Beneficial Polyphenols & What Foods Have Them
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Best Foods For Collagen Production
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Andrea Suarez gives us the low-down on collagen synthesis and maintenance. Collagen is the most abundant protein in our body, and it can be fairly described as “the stuff that holds us together”. It’s particularly important for joints and bones too, though many people’s focus on it is for the skin. Whatever your priorities, collagen levels are something it pays to be mindful of, as they usually drop quite sharply after a certain age. What certain age? Well, that depends a lot on you, and your diet and lifestyle. But it can start to decline from the age of 30 with often noticeable drop-offs in one’s mid-40s and again in one’s mid-60s.
Showing us what we’re made of
There’s a lot more to having good collagen levels than just how much collagen we consume (which for vegetarians/vegans, will be “none”, unless using the “except if for medical reasons” exemption, which is probably a little tenuous in the case of collagen but nevertheless it’s a possibility; this exemption is usually one that people use for, say, a nasal spray vaccine that contains gelatine, or a medicinal tablet that contains lactose, etc).
Rather, having good collagen levels is also a matter of what we eat that allows us to synthesize our own collagen (which includes: its ingredients, and various “helper” nutrients), as well as what dietary adjustments we make to avoid our extant collagen getting broken down, degraded, and generally lost.
Here’s what Dr. Suarez recommends:
Protein-rich foods (but watch out)
- Protein is essential for collagen production.
- Sources: fish, soy, lean meats (but not red meats, which—counterintuitively—degrade collagen), eggs, lentils.
- Egg whites are high in lysine, vital for collagen synthesis.
- Bone broth is a natural source of collagen.
Omega-3 fatty acids
- Omega-3s are anti-inflammatory and protect skin collagen.
- Sources: walnuts, chia seeds, flax seeds, fatty fish (e.g. mackerel, sardines).
Leafy greens
- Leafy dark green vegetables (e.g. kale, spinach) are rich in vitamins C and B9.
- Vitamin C is crucial for collagen synthesis and acts as an antioxidant.
- Vitamin B9 supports skin cell division and DNA repair.
Red fruits & vegetables
- Red fruits/vegetables (e.g. tomatoes, red bell peppers) contain lycopene, an antioxidant that protects collagen from UV damage (so, that aspect is mostly relevant for skin, but antioxidants are good things to have in all of the body in any case).
Orange-colored vegetables
- Carrots and sweet potatoes are rich in vitamin A, which helps in collagen repair and synthesis.
- Vitamin A is best from food, not supplements, to avoid potential toxicity.
Fruits rich in vitamin C
- Citrus fruits, kiwi, and berries are loaded with vitamin C and antioxidants, essential for collagen synthesis and skin health.
Soy
- Soy products (e.g. tofu, soybeans) contain isoflavones, which reduce inflammation and inhibit enzymes that degrade collagen.
- Soy is associated with lower risks of chronic diseases.
Garlic
- Garlic contains sulfur, taurine, and lipoic acid, important for collagen production and repair.
What to avoid:
- Reduce foods high in advanced glycation end products (AGEs), which damage collagen and promote inflammation.
- AGEs are found in fried, roasted, or grilled fatty proteinous foods (e.g. meat, including synthetic meat, and yes, including grass-fed nicely marketed meat—although processed meat such as bacon and sausages are even worse than steaks etc).
- Switch to cooking methods like boiling or steaming to reduce AGE levels.
- Processed foods, sugary pastries, and red meats contribute to collagen degradation.
General diet tips:
- Incorporate more plant-based, antioxidant-rich foods.
- Opt for slow cooking to reduce AGEs.
- Since sustainability is key, choose foods you enjoy for a collagen-boosting diet that you won’t seem like a chore a month later.
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
We Are Such Stuff As Fish Are Made Of ← our main feature research review about collagen
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: