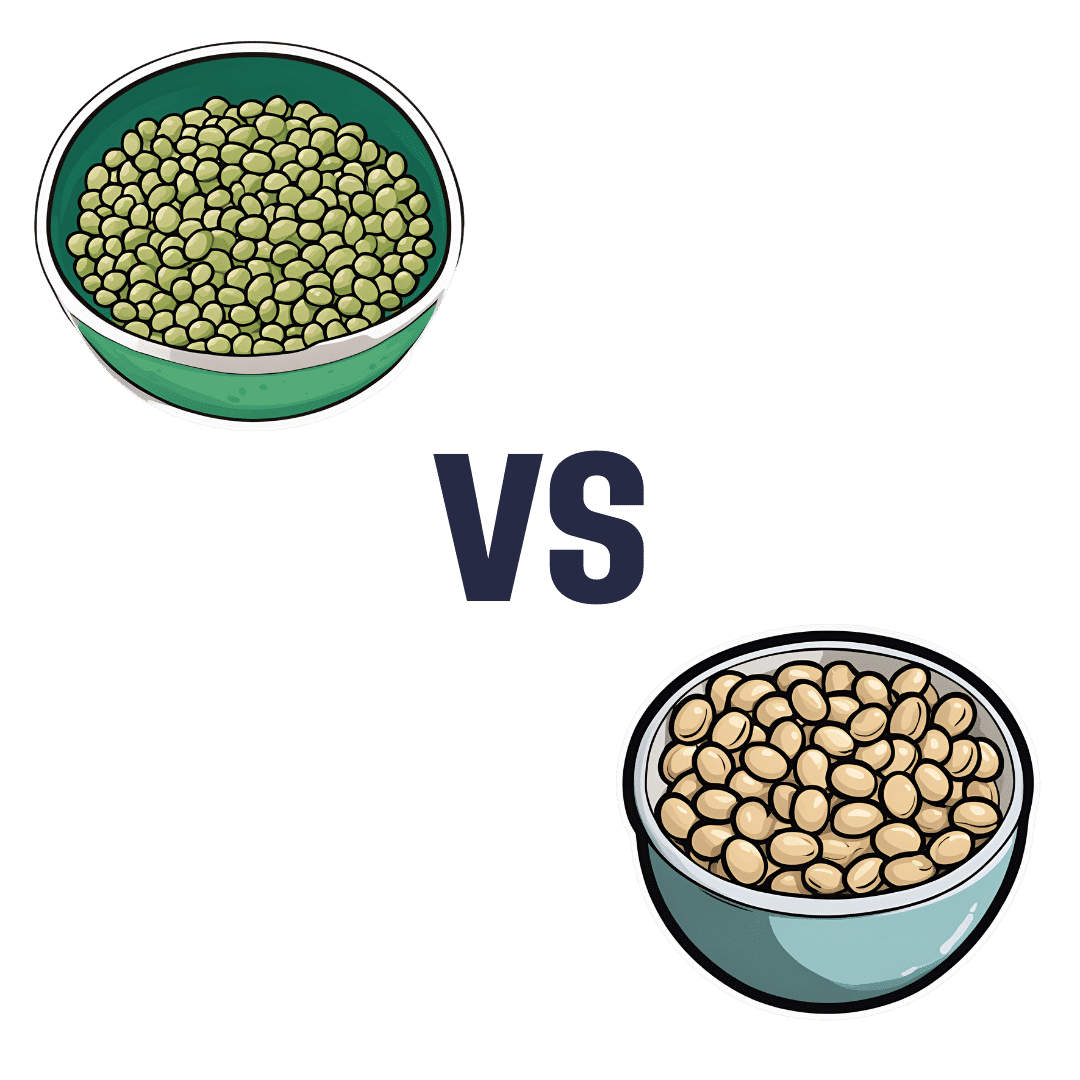
Mung Beans vs Soy Beans – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing mung beans to soy beans, we picked the soy.
Why?
Mung beans are great, but honestly, it’s not close:
In terms of macronutrients, soy has more than 2x the protein (of which, it’s also a complete protein, containing significant amounts of all essential amino acids) while mung beans have more than 2x the carbs. In their defense, mung beans also have very slightly more fiber, but the carb:fiber ratio is such that soy beans have the lower GI by far.
When it comes to vitamins, mung beans have more of vitamins A, B3, B5, and, B9, while soy beans have more of vitamins B2, B6, C, E, K, and choline, making for a moderate win for soy beans, especially as that vitamin K is more than 7x as much as mung beans have.
In the category of minerals, soy wins even more convincingly; soy beans have more calcium, copper, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc. On the other hand, mung beans have more sodium.
In short, while mung beans are a very respectable option, they don’t come close to meaningfully competing with soy.
Want to learn more?
You might like to read:
How To Sprout Your Seeds, Grains, Beans, Etc
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How To Clean Your Brain (Glymphatic Health Primer)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
That’s not a typo! The name “glymphatic system” was coined by the Danish neuroscientist Dr. Maiken Nedergaard, and is a nod to its use of glial cells to do a similar job to that of the peripheral lymphatic system—but this time, in the CNS. Today, we have Dr. Jin Sung to tell us more:
Brainwashing (but not like that)
The glymphatic system may sound like a boring job, but so does “sanitation worker” in a city—yet the city would grind to a messy halt very very quickly without them. Same goes for your brain.
Diseases that are prevalent when this doesn’t happen the way it should include Alzheimer’s (beta-amyloid clearance) and Parkinson’s (alpha-synuclein clearance) amongst others.
Things Dr. Sung recommends for optimal glymphatic function include: sleep (7–9 hours), exercise (30–45 minutes daily), hydration (half your bodyweight in pounds, in ounces, so if your body weighs 150 lbs, that means 75 oz of water), good posture (including the use of good ergonomics, e.g. computer monitor at right height, car seat correct, etc), stress reduction (reduces inflammatory cytokines), getting enough omega-3 (the brain needs certain fats to work properly, and this is the one most likely to see a deficit), vagal stimulation (methods include humming, gargling, and gagging—please note we said vagal stimulation; easy to misread at a glance!), LED light therapy, and fasting (intermittent or prolonged).
For more on each of these, including specific tips, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
- Ask Not What Your Lymphatic System Can Do For You…
- The Vagus Nerve (And How You Can Make Use Of It)
- Casting Yourself In A Healthier Light
- Intermittent Fasting: How Does It Work?
Take care!
Share This Post
-
What causes food cravings? And what can we do about them?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Many of us try to eat more fruits and vegetables and less ultra-processed food. But why is sticking to your goals so hard?
High-fat, sugar-rich and salty foods are simply so enjoyable to eat. And it’s not just you – we’ve evolved that way. These foods activate the brain’s reward system because in the past they were rare.
Now, they’re all around us. In wealthy modern societies we are bombarded by advertising which intentionally reminds us about the sight, smell and taste of calorie-dense foods. And in response to these powerful cues, our brains respond just as they’re designed to, triggering an intense urge to eat them.
Here’s how food cravings work and what you can do if you find yourself hunting for sweet or salty foods.
Fascinadora/Shutterstock What causes cravings?
A food craving is an intense desire or urge to eat something, often focused on a particular food.
We are programmed to learn how good a food tastes and smells and where we can find it again, especially if it’s high in fat, sugar or salt.
Something that reminds us of enjoying a certain food, such as an eye-catching ad or delicious smell, can cause us to crave it.
Our brains learn to crave foods based on what we’ve enjoyed before. fon thachakul/Shutterstock The cue triggers a physical response, increasing saliva production and gastric activity. These responses are relatively automatic and difficult to control.
What else influences our choices?
While the effect of cues on our physical response is relatively automatic, what we do next is influenced by complex factors.
Whether or not you eat the food might depend on things like cost, whether it’s easily available, and if eating it would align with your health goals.But it’s usually hard to keep healthy eating in mind. This is because we tend to prioritise a more immediate reward, like the pleasure of eating, over one that’s delayed or abstract – including health goals that will make us feel good in the long term.
Stress can also make us eat more. When hungry, we choose larger portions, underestimate calories and find eating more rewarding.
Looking for something salty or sweet
So what if a cue prompts us to look for a certain food, but it’s not available?
Previous research suggested you would then look for anything that makes you feel good. So if you saw someone eating a doughnut but there were none around, you might eat chips or even drink alcohol.
But our new research has confirmed something you probably knew: it’s more specific than that.
If an ad for chips makes you look for food, it’s likely a slice of cake won’t cut it – you’ll be looking for something salty. Cues in our environment don’t just make us crave food generally, they prompt us to look for certain food “categories”, such as salty, sweet or creamy.
Food cues and mindless eating
Your eating history and genetics can also make it harder to suppress food cravings. But don’t beat yourself up – relying on willpower alone is hard for almost everyone.
Food cues are so powerful they can prompt us to seek out a certain food, even if we’re not overcome by a particularly strong urge to eat it. The effect is more intense if the food is easily available.
This helps explain why we can eat an entire large bag of chips that’s in front of us, even though our pleasure decreases as we eat. Sometimes we use finishing the packet as the signal to stop eating rather than hunger or desire.
Is there anything I can do to resist cravings?
We largely don’t have control over cues in our environment and the cravings they trigger. But there are some ways you can try and control the situations you make food choices in.
- Acknowledge your craving and think about a healthier way to satisfy it. For example, if you’re craving chips, could you have lightly-salted nuts instead? If you want something sweet, you could try fruit.
- Avoid shopping when you’re hungry, and make a list beforehand. Making the most of supermarket “click and collect” or delivery options can also help avoid ads and impulse buys in the aisle.
- At home, have fruit and vegetables easily available – and easy to see. Also have other nutrient dense, fibre-rich and unprocessed foods on hand such as nuts or plain yoghurt. If you can, remove high-fat, sugar-rich and salty foods from your environment.
- Make sure your goals for eating are SMART. This means they are specific, measurable, achievable, relevant and time-bound.
- Be kind to yourself. Don’t beat yourself up if you eat something that doesn’t meet your health goals. Just keep on trying.
Gabrielle Weidemann, Associate Professor in Psychological Science, Western Sydney University and Justin Mahlberg, Research Fellow, Pyschology, Monash University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Statins: Study Insights
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Q: Can you let us know about more studies that have been done on statins? Are they really worth taking?
That is a great question! We imagine it might have been our recent book recommendation that prompted it? It’s quite a broad question though, so we’ll do that as a main feature in the near future!
Share This Post
Related Posts
-
Longevity… Simplified – by Dr. Howard Luks
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In the spirit of the book itself, we’ll keep this one simple:
The information in this book will not be new to regular readers of 10almonds, or at least, not if you’ve been with us for a while (because we can only cover so much per day, so long-time readers will have accumulated more knowledge).
On the other hand, the information is clear, correct, and very much stripped down to the most important basics. Not the very simplest basics, which would be an oversimplification to the point of inutility, but the most important basics.
To take an example, when it comes to exercise, he doesn’t say “exercise more” but rather that “a complete exercise program has four pillars: aerobic training, resistance training, balance training, and high-intensity interval training (HIIT)”, and then he goes about explaining, in clear and simple terms, how to do those.
The style is similar when it comes to diet, sleep, and body-part-specific chapters such as about heart health, brain health, and so forth.
Bottom line: if you’re a long-time 10almonds reader, you probably don’t need this one, but it’d be a great book for someone else who has expressed an interest in getting healthier, as it really is a top-tier “primer” in increasing health and healthspan.
Click here to check out Longevity… Simplified, and enjoy simplified longevity!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Sweet Dreams Are Made Of Cheese (Or Are They?)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝In order to lose a little weight I have cut out cheese from my diet – and am finding that I am sleeping better. Would be interested in your views on cheese and sleep, and whether some types of cheese are worse for sleep than others. I don’t want to give up cheese entirely!❞
In principle, there’s nothing in cheese that, biochemically, should impair sleep. If anything, its tryptophan content could aid good sleep.
Tryptophan is found in many foods, including cheese, which (of common foods, anyway), for example cheddar cheese ranks second only to pumpkin seeds in tryptophan content.
Tryptophan can be converted by the body into 5-HTP, which you’ve maybe seen sold as a supplement. Its full name is 5-hydroxytryptophan.
5-HTP can, in turn, be used to make melatonin and/or serotonin. Which of those you will get more of, depends on what your body is being cued to do by ambient light/darkness, and other environmental cues.
If you are having cheese and then checking your phone, for instance, or otherwise hanging out where there are white/blue lights, then your body may dutifully convert the tryptophan into serotonin (calm wakefulness) instead of melatonin (drowsiness and sleep).
In short: the cheese will (in terms of this biochemical pathway, anyway) augment some sleep-inducing or wakefulness-inducing cues, depending on which are available.
You may be wondering: what about casein?
Casein is oft-touted as producing deep sleep, or disturbed sleep, or vivid dreams, or bad dreams. There’s no science to back any of this up, though the following research review is fascinating:
Dreams of the Rarebit Fiend: food and diet as instigators of bizarre and disturbing dreams
(it largely supports the null hypothesis of “not a causal factor” but does look at the many more likely alternative explanations, ranging from associated actually casual factors (such as alcohol and caffeine) and placebo/nocebo effect)
Finally, simple digestive issues may be the real thing at hand:
Worth noting that around two thirds of all people, including those who regularly enjoy dairy products, have some degree of lactose intolerance:
Lactose Intolerance in Adults: Biological Mechanism and Dietary Management
So, in terms of what cheese may be better/worse for you in this context, you might try experimenting with lactose-free cheese, which will help you identify whether that was the issue!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Meds That Impair Decision-Making
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Impairment to cognitive function is often comorbid with Parkinson’s disease. That is to say: it’s not a symptom of Parkinson’s, but it often occurs in the same people. This may seem natural: after all, both are strongly associated with aging.
However, recent (last month, at time of writing) research has brought to light a very specific way in which medication for Parkinson’s may impair the ability to make sound decisions.
Obviously, this is a big deal, because it can affect healthcare decisions, financial decisions, and more—greatly impacting quality of life.
See also: Age-related differences in financial decision-making and social influence
(in which older people were found more likely to be influenced by the impulsive financial preferences of others than their younger counterparts, when other factors are controlled for)
As for how this pans out when it comes to Parkinson’s meds…
Pramipexole (PPX)
This drug can, due to an overlap in molecular shape, mimic dopamine in the brains of people who don’t have enough—such as those with Parkinson’s disease. This (as you might expect) helps alleviate Parkinson’s symptoms.
However, researchers found that mice treated with PPX and given a touch-screen based gambling game picked the high-risk, high reward option much more often. In the hopes of winning strawberry milkshake (the reward), they got themselves subjected to a lot of blindingly-bright flashing lights (the risk, to which untreated mice were much more averse, as this is very stressful for a mouse).
You may be wondering: did the mice have Parkinson’s?
The answer: kind of; they had been subjected to injections with 6-hydroxydopamine, which damages dopamine-producing neurons similarly to Parkinson’s.
This result was somewhat surprising, because one would expect that a mouse whose depleted dopamine was being mimicked by a stand-in (thus, doing much of the job of dopamine) would be less swayed by the allure of gambling (a high-dopamine activity), since gambling is typically most attractive to those who are desperate to find a crumb of dopamine somewhere.
They did find out why this happened, by the way, the PPX hyperactivated the external globus pallidus (also called GPe, and notwithstanding the name, this is located deep inside the brain). Chemically inhibiting this area of the brain reduced the risk-taking activity of the mice.
This has important implications for Parkinson’s patients, because:
- on an individual level, it means this is a side effect of PPX to be aware of
- on a research-and-development level, it means drugs need to be developed that specifically target the GPe, to avoid/mitigate this side effect.
You can read the study in full here:
Don’t want to get Parkinson’s in the first place?
While nothing is a magic bullet, there are things that can greatly increase or decrease Parkinson’s risk. Here’s a big one, as found recently (last week, at the time of writing):
Air Pollution and Parkinson’s Disease in a Population-Based Study
Also: knowing about its onset sooner rather than later is scary, but beneficial. So, with that in mind…
Recognize The Early Symptoms Of Parkinson’s Disease
Finally, because Parkinson’s disease is theorized to be caused by a dysfunction of alpha-synuclein clearance (much like the dysfunction of beta-amyloid clearance, in the case of Alzheimer’s disease), this means that having a healthy glymphatic system (glial cells doing the same clean-up job as the lymphatic system, but in the brain) is critical:
How To Clean Your Brain (Glymphatic Health Primer)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: