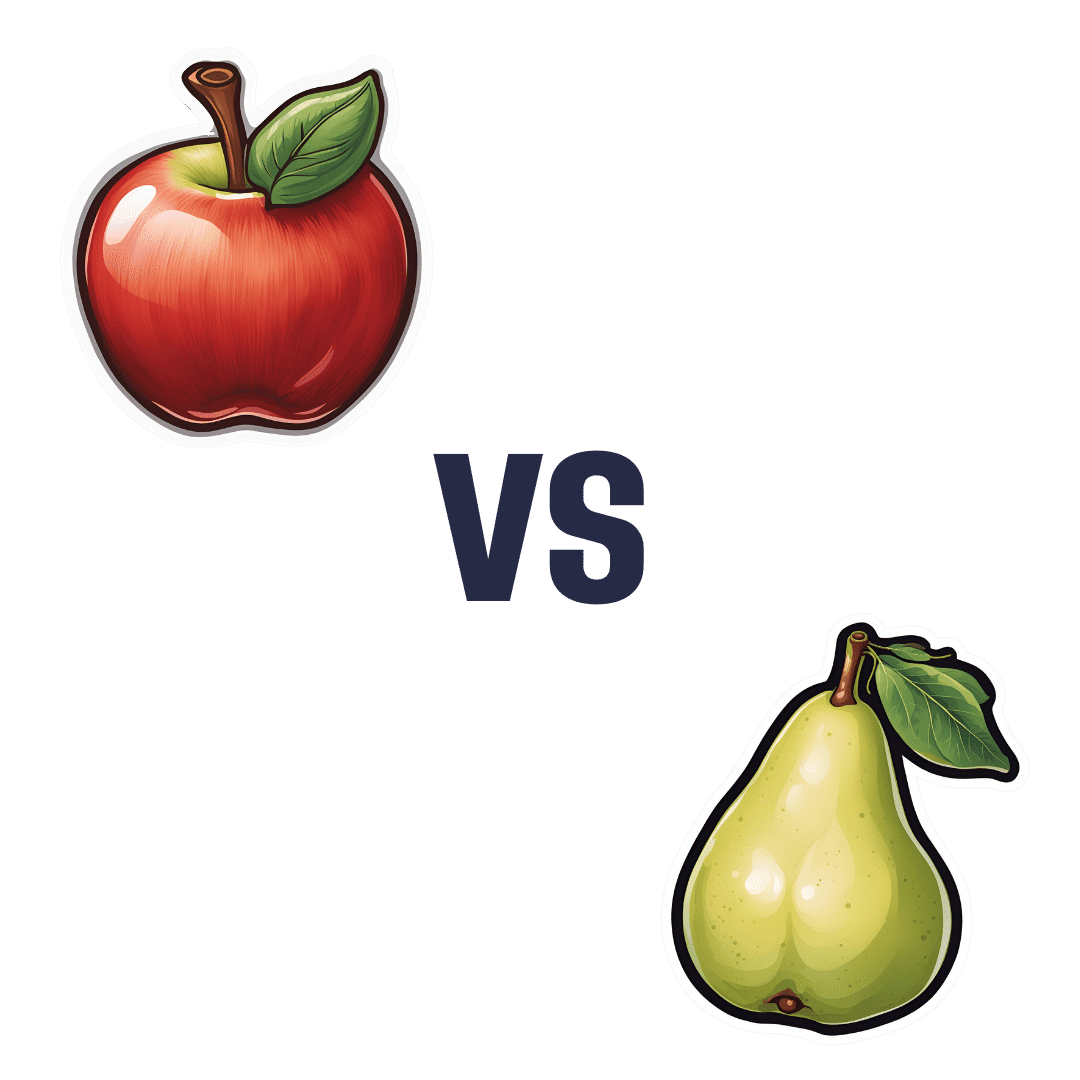
Apple vs Pear – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing apple to pear, we picked the pear.
Why?
Both are great! But there’s a category that puts pears ahead of apples…
Looking at their macros first, pears contain more carbs but also more fiber. Both are low glycemic index foods, though.
In the category of vitamins, things are moderately even: apples contain more of vitamins A, B1, B6, and E, while pears contain more of vitamins B3, B9, K, and choline. That’s a 4:4 split, and the two fruits are about equal in the other vitamins they both contain.
When it comes to minerals, pears contain more calcium, copper, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc. A resounding victory for pears, as apples are not higher in any mineral.
In short, if an apple a day keeps the doctor away, a pear should keep the doctor away for about a day and a half, based on the extra nutrients ← this is slightly facetious as medicine doesn’t work like that, but you get the idea: pears simply have more to offer. Apples are still great though! Enjoy both! Diversity is good.
Want to learn more?
You might like to read:
From Apples To Bees, And High-Fructose Cs: Which Sugars Are Healthier, And Which Are Just The Same?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How the stress of playing chess can be fatal
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The death of a chess player in the middle of a match at the world’s most prestigious competition may have shocked those who view the game as a relaxing pastime. Kurt Meier, 67, collapsed during his final match in the tournament and died in hospital later that day. But chess, like any other game or sport, can lead to an immense amount of stress, which can be bad for a competitor’s physical health too.
We tend to associate playing sport or games with good health and well-being. And there are a countless number of studies showing playing games has an association with feeling happier. While this argument is true for recreational players, the story can be different for the elite, where success and failure are won and lost by the finest margins and where winning can mean funding and a future, and losing can mean poverty and unemployment. If this is the case, can being successful at a sport or game actually be bad for you?
Competitive anxiety
Elite competition can be stressful because the outcome is so important to the competitors. We can measure stress using a whole range of physiological indicators such as heart rate and temperature, and responses such as changes in the intensity of our emotions.
Emotions provide a warning of threat. So if you feel that achieving your goal is going to be difficult, then expect to feel intense emotions. The leading candidate that signals we are experiencing stress is anxiety, characterised by thoughts of worry, fears of dread about performance, along with accompanying physiological responses such as increased heart rate and sweaty palms. If these symptoms are experienced regularly or chronically, then this is clearly detrimental to health.
This stress response is probably not restricted to elite athletes. Intense emotions are linked to trying to achieve important goals and while it isn’t the only situation where it occurs, it is just very noticeable in sport.
The causes of stress
It makes more sense to focus on what the causes of stress are rather than where we experience it. The principle is that the more important the goal is to achieve, then the greater the propensity for the situation to intensify emotions.
Emotions intensify also by the degree of uncertainty and competing, at whatever level of a sport, is uncertain when the opposition is trying its hardest to win the contest and also has a motivation to succeed. The key point is that almost all athletes at any level can suffer bouts of stress, partly due to high levels of motivation.
A stress response is also linked to how performance is judged and reported. Potentially stressful tasks tend to be ones where performance is public and feedback is immediate. In chess – as with most sporting contests – we see who the winner is and can start celebrating success or commiserating failure as soon as the game is over.
There are many tasks which have similar features. Giving a speech in public, taking an academic examination, or taking your driving test are all examples of tasks that can illicit stress. Stress is not restricted to formal tasks but can also include social tasks. Asking a potential partner for a date, hand in marriage, and meeting the in-laws for the first time can be equally stressful.
Winning a contest or going on a date relate to higher-order goals about how we see ourselves. If we define ourselves as “being a good player” or “being attractive or likeable” then contrasting information is likely to associate with unpleasant emotions. You will feel devastated if you are turned down when asking someone out on a date, for instance, and if this was repeated, it could lead to reduced self-esteem and depression.
The key message here is to recognise what your goals are and think about how important they are. If you want to achieve them with a passion and if the act of achieving them leads to intense and sometimes unwanted emotions, then it’s worth thinking about doing some work to manage these emotions.
Andrew Lane, Professor in Sport and Learning, University of Wolverhampton
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
80-Year-Olds Share Their Biggest Regrets
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Notwithstanding the title, some of these people are a little younger than 80, but this adds to the interest a little as we see the different regrets / learned wisdoms at different stages of later life!
If we could turn back the time…
There are dozens of life regrets / wishes / retroactive advices shared in this video; here are some highlights:
- “My regret was I had a dysfunctional family and I wish I would have learned not to take responsibility.”
- “In my 30s, when I started drinking very heavily, I wish I hadn’t done that because it escalated to drug abuse.”
- “When my parents were old ages, I was working very hard… I didn’t have time to take care of them, not even spend the time with them. That’s my biggest regret.”
- “Live life to the fullest because none of us have any assurance on how old we’re going to be when we’re going to die.”
- “If I could do it over, I would have called home more and realized what my brother was going through.”
- “Spent a lot of years being concerned about what other people thought of me.”
- “You got to be careful what you say to your children because it means a lot.”
For the rest, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
- Managing Your Mortality Without Regrets
- How To Avoid Carer Burnout (Without Dropping Care)
- Managing Sibling Relationships In Adult Life
- Family Estrangment & How To Fix It
Take care!
Share This Post
-
The Minerals That Neutralize Viruses (While Being Harmless To Humans)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Researchers in Estonia and Sweden (it was a joint project, with five researchers from each country) have found a way to use titanium dioxide nanoparticles to neutralize viruses, including COVID & flu.
Titanium dioxide, yes, the common additive to foods, cosmetics, and more (in most cases, added as a non-bleaching whitening agent—simply, titanium dioxide is body-safe, white in color, and very reflective, making it a brilliant, shiny white). Also used in sunscreens, for its excellent safety profile and again, its full-spectrum reflectiveness.
See also: Who Screens The Sunscreens?
How it works
Some viruses, including coronaviruses and influenza viruses, have an outer layer that’s a lipid membrane. The researchers found (by testing against multiple viruses, and by using a control of silicotungstate polyoxymethalate nanoparticles), that the ability of titanium dioxide to bind to phospholipids (and ability that the silicotungstate polyoxymethalate doesn’t have) means that the nanoparticles bind to the virus’s outer case, thus preventing it from effectively entering human cells (which it needs to do in order to infect the host, as this is how viruses replicate themselves).
What this means, in practical terms
While more research will be needed to know whether this can be used in the medicinal sense, it already means that a nanoparticle spray can be used to create virus-neutralizing layers on surfaces and in air filters. This alone could greatly reduce transmission in enclosed spaces such as public transport (ranging from taxis to airplanes), as well as other places where people get packed into a small space.
If you have an air purifier at home, keep an eye out for when improved filters arrive on the market!
See also: What’s Lurking In Your Household Air?
Wait, you said “minerals”; are there more?
It seems so, but we can’t truly say for sure until they’ve been tested. However, the researchers see no reason why other small metal oxides that bind strongly to phospholipids shouldn’t work exactly the same way—which would include iron oxide (yes, as in rust) and aluminum oxide (the coating that automatically forms immediately when aluminum is exposed to oxygen (aluminum is so reactive to oxygen, that it’s almost impossible to get aluminum without an oxidized surface, unless you use something else to coat it, or cut it in an oxygen-free atmosphere and keep it there).
You can read the paper itself here:
Molecular mechanisms behind the anti corona virus activity of small metal oxide nanoparticles
And on a related note (different scientists, different science, similar principle, though, using mineral nanotechnology to kill microbes):
❝Researchers report that laboratory tests of their nanoflower-coated dressings demonstrate antibiotic, anti-inflammatory and biocompatible properties. They say these results show these tannic acid and copper(II) phosphate sprouted nanoflower bandages are promising candidates for treating infections and inflammatory conditions.❞
Read in full: This delicate nanoflower is downright deadly to bacteria
Want to learn more?
Check out:
Move over, COVID and Flu! We Have “Hybrid Viruses” To Contend With Now
Take care!
Share This Post
Related Posts
-
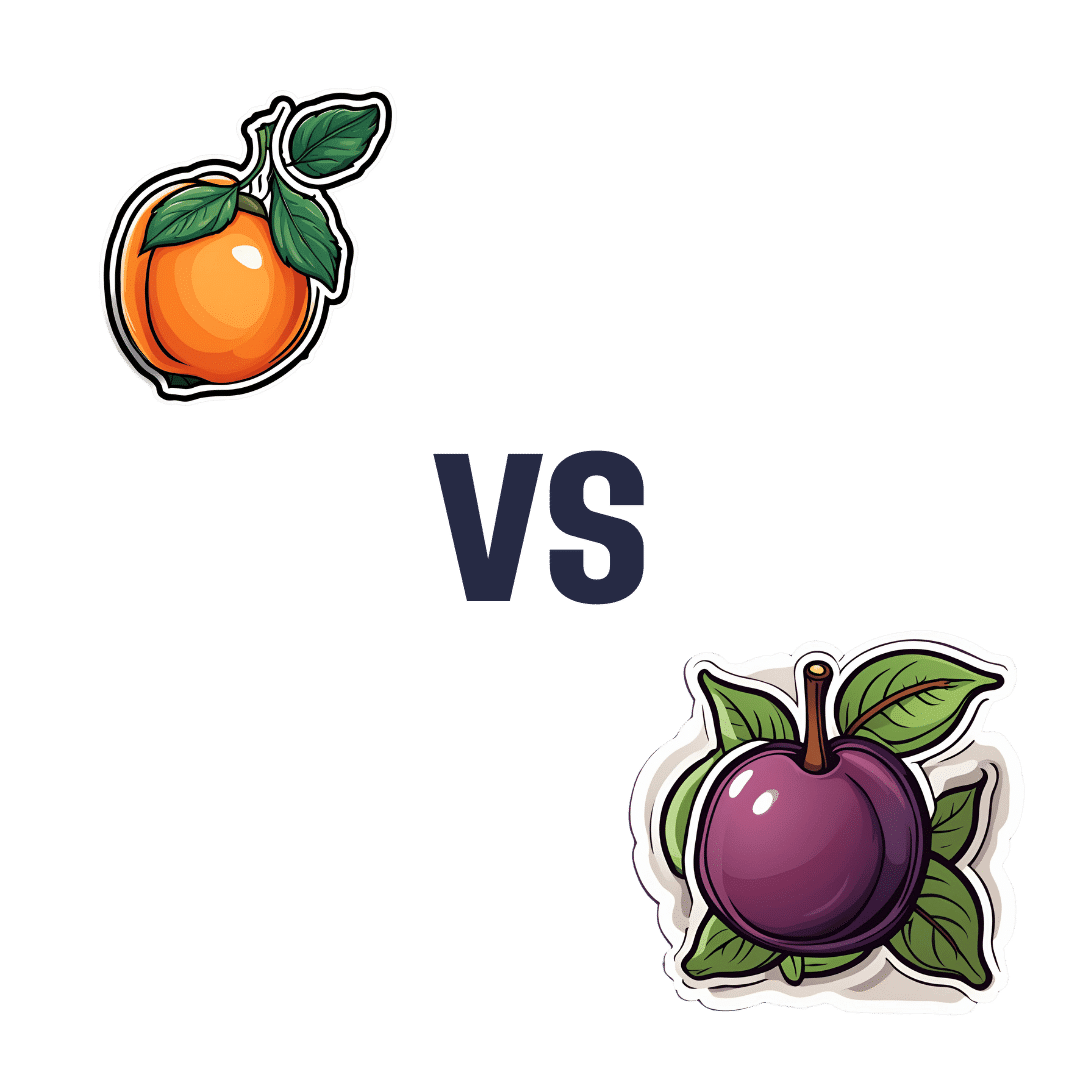
Apricots vs Plums – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing apricots to plums, we picked the apricots.
Why?
Both are great, but it wasn’t close!
In terms of macros, apricots have more fiber, protein, and carbs, with their fiber:carb ratio also giving them the lower glycemic index (although, as usual for any whole fruit, neither are going to give anyone metabolic disease). In any case, by the numbers, and especially for having more fiber, apricots win this category.
In the category of vitamins, apricots have more of vitamins A, B1, B2, B3, B5, B6, B7, B9, C, E, and choline, while plums have more vitamin K. A clear win for apricots.
When it comes to minerals, apricots have more calcium, copper, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc, while plums are not higher in any mineral. Another hands-down win for apricots.
Looking at polyphenols, both have an abundance of many, especially assorted flavanols, including quercetin. However, plums additionally have some anthocyanins (whence the color), so they get a marginal victory in this round.
Still, adding up the sections, it’s a 3:1 win for apricots. Of course, do enjoy either or both, though; diversity is good!
Want to learn more?
You might like:
Top 8 Fruits That Prevent & Kill Cancer
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Practical Optimism – by Dr. Sue Varma
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve written before about how to get your brain onto a more positive track (without toxic positivity), but there’s a lot more to be said than we can fit into an article, so here’s a whole book packed full with usable advice.
The subtitle claims “the art, science, and practice of…”, but mostly it’s the science of. If there’s art to be found here, then this reviewer missed it, and as for the practice of, well, that’s down to the reader, of course.
However, it is easy to use the contents of this book to translate science into practice without difficulty.
If you’re a fan of acronyms, initialisms, and other mnemonics (such as the rhyming “Name, Claim, Tame, and Reframe”), then you’ll love this book as they come thick and fast throughout, and they contribute to the overall ease of application of the ideas within.
The writing style is conversational but with enough clinical content that one never forgets who is speaking—not in the egotistical way that some authors do, but rather, just, she has a lot of professional experience to share and it shows.
Bottom line: if you’d like to be more optimistic without delving into the delusional, this book can really help a lot with that (in measurable ways, no less!).
Click here to check out Practical Optimism, and brighten up your life!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Codependency Isn’t What Most People Think It Is
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Codependency isn’t what most people think it is
In popular parlance, people are often described as “codependent” when they rely on each other to function normally. That’s interdependent mutualism, and while it too can become a problem if a person is deprived of their “other half” and has no idea how to do laundry and does not remember to take their meds, it’s not codependency.
Codependency finds its origins in the treatment and management of alcoholism, and has been expanded to encompass other forms of relationships with dependence on substances and/or self-destructive behaviors—which can be many things, including the non-physical, for example a pattern of irresponsible impulse-spending, or sabotaging one’s own relationship(s).
We’ll use the simplest example, though:
- Person A is (for example) an alcoholic. They have a dependency.
- Person B, married to A, is not an alcoholic. However, their spouse’s dependency affects them greatly, and they do what they can to manage that, and experience tension between wanting to “save” their spouse, and wanting their spouse to be ok, which latter, superficially, often means them having their alcohol.
Person B is thus said to be “codependent”.
The problem with codependency
The problems of codependency are mainly twofold:
- The dependent partner’s dependency is enabled and thus perpetuated by the codependent partner—they might actually have to address their dependency, if it weren’t for their partner keeping them from too great a harm (be it financially, socially, psychologically, medically, whatever)
- The codependent partner is not having a good time of it either. They have the stress of two lives with the resources (e.g. time) of one. They are stressing about something they cannot control, understandably worrying about their loved one, and, worse: every action they might take to “save” their loved one by reducing the substance use, is an action that makes their partner unhappy, and causes conflict too.
Note: codependency is often a thing in romantic relationships, but it can appear in other relationships too, e.g. parent-child, or even between friends.
See also: Development and validation of a revised measure of codependency
How to deal with this
If you find yourself in a codependent position, or are advising someone who is, there are some key things that can help:
- Be a nurturer, not a rescuer. It is natural to want to “rescue” someone we care about, but there are some things we cannot do for them. Instead, we must look for ways to build their strength so that they can take the steps that only they can take to fix the problem.
- Establish boundaries. Practise saying “no”, and also be clear over what things you can and cannot control—and let go of the latter. Communicate this, though. An “I’m not the boss of you” angle can prompt a lot of people to take more personal responsibility.
- Schedule time for yourself. You might take some ideas from our previous tangentially-related article:
How To Avoid Carer Burnout (Without Dropping Care)
Want to read more?
That’s all we have space for today, but here’s a very useful page with a lot of great resources (including questionnaires and checklist and things, in case you’re thinking “is it, or…?”)
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: