Protein Immune Support Salad
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How to get enough protein from a salad, without adding meat? Cashews and chickpeas have you more than covered! Along with the leafy greens and an impressive array of minor ingredients full of healthy phytochemicals, this one’s good for your muscles, bones, skin, immune health, and more.
You will need
- 1½ cups raw cashews (if allergic, omit; the chickpeas and coconut will still carry the dish for protein and healthy fats)
- 2 cans (2x 14oz) chickpeas, drained
- 1½ lbs baby spinach leaves
- 2 large onions, finely chopped
- 3 oz goji berries
- ½ bulb garlic, finely chopped
- 2 tbsp dessicated coconut
- 1 tbsp dried cumin
- 1 tbsp nutritional yeast
- 2 tsp chili flakes
- 1 tsp black pepper, coarse ground
- ½ tsp MSG, or 1 tsp low-sodium salt
- Extra virgin olive oil, for cooking
Method
(we suggest you read everything at least once before doing anything)
1) Heat a little oil in a pan; add the onions and cook for about 3 minutes.
2) Add the garlic and cook for a further 2 minutes.
3) Add the spinach, and cook until it wilts.
4) Add the remaining ingredients except the coconut, and cook for another three minutes.
5) Heat another pan (dry); add the coconut and toast for 1–2 minutes, until lightly golden. Add it to the main pan.
6) Serve hot as a main, or an attention-grabbing side:

Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Cashew Nuts vs Coconut – Which is Healthier?
- What Matters Most For Your Heart?
- Beyond Supplements: The Real Immune-Boosters!
- Goji Berries: Which Benefits Do They Really Have?
- Our Top 5 Spices: How Much Is Enough For Benefits?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Do we need animal products to be healthy?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Do we need animal products to be healthy?
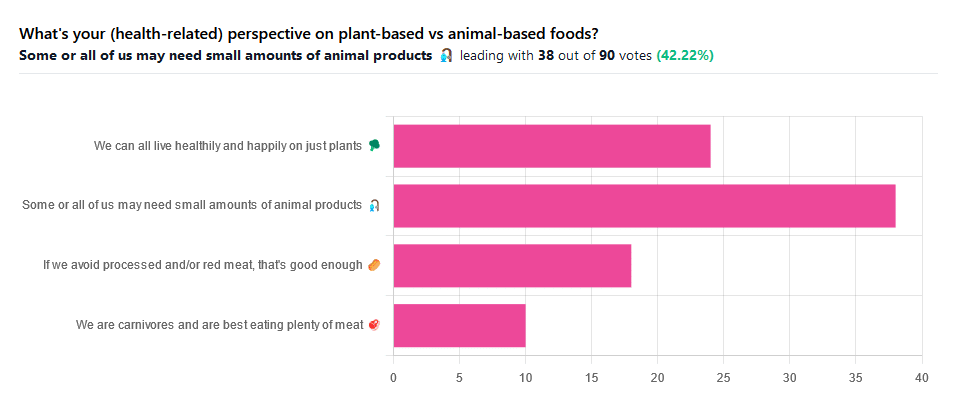
We asked you for your (health-related) perspective on plant-based vs anima-based foods, and got the above-pictured spread of answers.
“Some or all of us may need small amounts of animal products” came out on top with more votes than the two more meat-eatery options combined, and the second most popular option was the hard-line “We can all live healthily and happily on just plants”.
Based on these answers, it seems our readership has quite a lot of vegans, vegetarians, and perhaps “flexitarians” who just have a little of animal products here and there.
Perhaps we should have seen this coming; the newsletter is “10almonds”, not “10 rashers of bacon”, after all.
But what does the science say?
We are carnivores and are best eating plenty of meat: True or False?
False. Let’s just rip the band-aid off for this one.
In terms of our anatomy and physiology, we are neither carnivores nor herbivores:
- We have a mid-length digestive tract (unlike carnivores and herbivores who have short and long ones, respectively)
- We have a mouthful of an assortment of teeth; molars and premolars for getting through plants from hard nuts to tough fibrous tubers, and we have incisors for cutting into flesh and (vestigial, but they’re there) canines that really serve us no purpose now but would have been a vicious bite when they were bigger, like some other modern-day primates.
- If we look at our closest living relatives, the other great apes, they are mostly frugivores (fruit-eaters) who supplement their fruity diet with a small quantity of insects and sometimes other small animals—of which they’ll often eat only the fatty organ meat and discard the rest.
And then, there’s the health risks associated with meat. We’ll not linger on this as we’ve talked about it before, but for example:
- Processed Meat Consumption and the Risk of Cancer: A Critical Evaluation of the Constraints of Current Evidence from Epidemiological Studies
- Red Meat Consumption (Heme Iron Intake) and Risk for Diabetes and Comorbidities?
- Health Risks Associated with Meat Consumption: A Review of Epidemiological Studies
- Associations of Processed Meat, Unprocessed Red Meat, Poultry, or Fish Intake With Incident Cardiovascular Disease and All-Cause Mortality
- Meat consumption: Which are the current global risks? A review of recent (2010-2020) evidences
If we avoid processed and/or red meat, that’s good enough: True or False?
True… Ish.
Really this one depends on one’s criteria for “good enough”. The above-linked studies, and plenty more like them, give the following broad picture:
- Red and/or processed meats are unequivocally terrible for the health in general
- Other mammalian meats, such as from pigs, are really not much better
- Poultry, on the other hand, the science is less clear on; the results are mixed, and thus so are the conclusions. The results are often barely statistically significant. In other words, when it comes to poultry, in the matter of health, the general consensus is that you can take it or leave it and will be fine. Some studies have found firmly for or against it, but the consensus is a collective scientific shrug.
- Fish, meanwhile, has almost universally been found to be healthful in moderation. You may have other reasons for wanting to avoid it (ethics, environmentalism, personal taste) but those things are beyond the scope of this article.
Some or all of us may need small amounts of animal products: True or False?
True! With nuances.
Let’s divide this into “some” and “all”. Firstly, some people may have health conditions and/or other mitigating circumstances that make an entirely plant-based diet untenable.
We’re going light on quotations from subscriber comments today because otherwise this article will get a bit long, but here’s a great example that’s worth quoting, from a subscriber who voted for this option:
❝I have a rare genetic disease called hereditary fructose intolerance. It means I lack the enzyme, Aldolase B, to process fructose. Eating fruits and veggies thus gives me severe hypoglycemia. I also have anemia caused by two autoimmune diseases, so I have to eat meat for the iron it supplies. I also supplement with iron pills but the pills alone can’t fix the problem entirely.❞
And, there’s the thing. Popular vegan talking-points are very good at saying “if you have this problem, this will address it; if you have that problem, that will address it”, etc. For every health-related objection to a fully plant-based diet there’s a refutation… Individually.
But actual real-world health doesn’t work like that; co-morbidities are very common, and in some cases, like our subscriber above, one problem undermines the solution to another. Add a third problem and by now you really just have to do what you need to do to survive.
For this reason, even the Vegan Society’s definition of veganism includes the clause “so far as is possible and practicable”.
Now, as for the rest of us “all”.
What if we’re really healthy and are living in optimal circumstances (easy access to a wide variety of choice of food), can we live healthily and happily just on plants?
No—on a technicality.
Vegans famously need to supplement vitamin B12, which is not found in plants. Ironically, much of the B12 in animal products comes from the animals themselves being given supplements, but that’s another matter. However, B12 can also be enjoyed from yeast. Popular options include the use of yeast extract (e.g. Marmite) and/or nutritional yeast in cooking.
Yeast is a single-celled microorganism that’s taxonomically classified as a fungus, even though in many ways it behaves like an animal (which series of words may conjure an amusing image, but we mean, biologically speaking).
However, it’s also not technically a plant, hence the “No—on a technicality”
Bottom line:
By nature, humans are quite versatile generalists when it comes to diet:
- Most of us can live healthily and happily on just plants if we so choose.
- Some people cannot, and will require varying kinds (and quantities) of animal products.
- As for red and/or processed meats, we’re not the boss of you, but from a health perspective, the science is clear: unless you have a circumstance that really necessitates it, just don’t.
- Same goes for pork, which isn’t red and may not be processed, but metabolically it’s associated with the same problems.
- The jury is out on poultry, but it strongly appears to be optional, healthwise, without making much of a difference either way
- Fish is roundly considered healthful in moderation. Enjoy it if you want, don’t if you don’t.
Share This Post
-
Chili Chestnut, Sweet Apricot, & Whipped Feta Toasts
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is a delightful breakfast or light lunch option, full of gut-healthy ingredients and a fair list of healthy polyphenols too.
You will need
- ½ baguette, sliced into ½” slices; if making your own, feel free to use our Delicious Quinoa Avocado Bread recipe. If buying shop-bought, a sourdough baguette will likely be the healthiest option, and tasty too.
- 4 oz feta cheese; if you are vegan, a plant-based version will work in culinary terms, but will have a different (less gut-healthy) nutritional profile, as plant-based cheeses generally use a lot of coconut oil and potato starch, and are not actually fermented.
- 1 tbsp yogurt; your preference what kind; live-cultured with minimal additives is of course best—and this time, plant-based is also just as good, healthwise, since they are fermented and contain more or less the same beneficial bacteria, and have a good macro profile too.
- 4 oz precooked chestnuts, finely chopped
- 6 dried apricots, finely chopped
- ¼ bulb garlic, grated
- 2 tsp harissa paste
- 1 tsp black pepper, coarse ground
- ¼ tsp MSG or ½ tsp low-sodium salt
- Extra virgin olive oil, for frying
- Optional garnish: finely chopped chives
Method
(we suggest you read everything at least once before doing anything)
1) Combine the feta and yogurt in a small, high-speed blender and process into a smooth purée. If it isn’t working, add 1 tbsp kettle-hot water and try again.
2) Heat the oil in a skillet over a medium heat; add the garlic and when it starts to turn golden, add the chestnuts and harissa, as well as the black pepper and MSG/salt. Stir for about 2 minutes, and then stir in the apricots and take it off the heat.
3) Toast the baguette slices under the grill. If you’re feeling bold about the multitasking, you can start this while still doing the previous step, for optimal timing. If not, simply doing it in the order presented is fine.
4) Assemble: spread the whipped feta over the toast; add the apricot-chestnut mixture, followed by the finely chopped chives if using, and serve immediately:
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Making Friends With Your Gut (You Can Thank Us Later)
- Apricots vs Peaches – Which is Healthier?
- Why You Should Diversify Your Nuts!
- Capsaicin For Weight Loss And Against Inflammation
- The Many Health Benefits Of Garlic
- Black Pepper’s Impressive Anti-Cancer Arsenal (And More)
- Sea Salt vs MSG – Which is Healthier?
Take care!
Share This Post
-
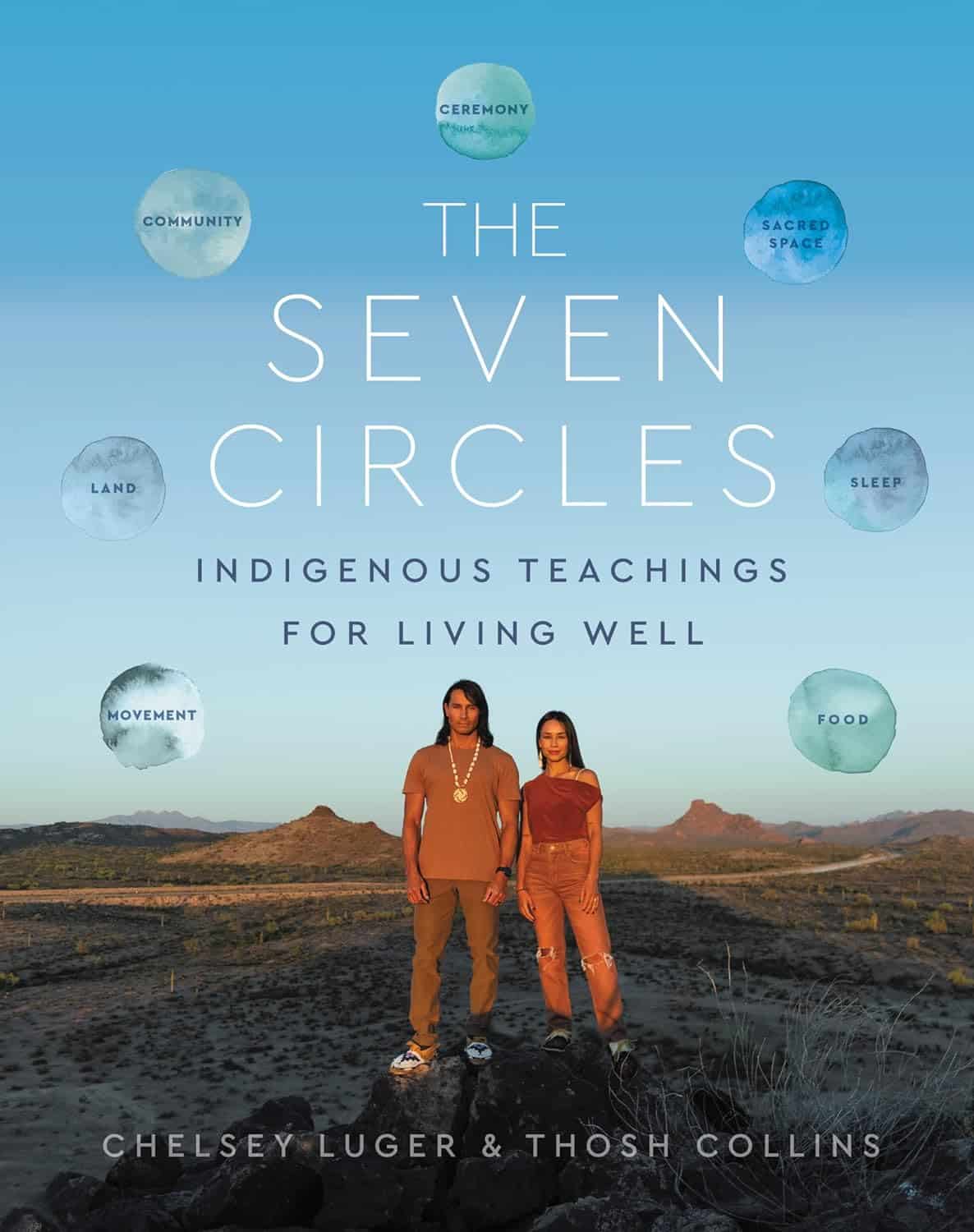
The Seven Circles – by Chelsey Luger & Thosh Collins
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
At first glance, this can seem like an unscientific book—you won’t find links to studies in this one, for sure! However, if we take a look at the seven circles in question, they are:
- Food
- Movement
- Sleep
- Ceremony
- Sacred Space
- Land
- Community
Regular 10almonds readers may notice that these seven items contain five of the things strongly associated with the “supercentenarian Blue Zones”. (If you are wondering why Native American reservations are not Blue Zones, the answer there lies less in health science and more in history and sociology, and what things have been done to a given people).
The authors—who are Native American, yes—present in one place a wealth of knowledge and know-how. Not even just from their own knowledge and their own respective tribes, but gathered from other tribes too.
Perhaps the strongest value of this book to the reader is in the explanation of noting the size of each of those circles, how they connect with each other, and providing a whole well-explained system for how we can grow each of them in harmony with each other.
Or to say the same thing in sciencey terms: how to mindfully improve integrated lifestyle factors synergistically for greater efficacy and improved health-adjusted quality-of-life years.
Bottom line: if you’re not averse to something that mostly doesn’t use sciencey terms of have citations to peer-reviewed studies peppered through the text, then this book has wisdom that’s a) older than the pyramids of Giza, yet also b) highly consistent with our current best science of Blue Zone healthy longevity.
Share This Post
Related Posts
-
Why are people on TikTok talking about going for a ‘fart walk’? A gastroenterologist weighs in
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
“Fart walks” have become a cultural phenomenon, after a woman named Mairlyn Smith posted online a now-viral video about how she and her husband go on walks about 60 minutes after dinner and release their gas.
Smith, known on TikTok as @mairlynthequeenoffibre and @mairlynsmith on Instagram, has since appeared on myriad TV and press interviews extolling the benefits of a fart walk. Countless TikTok and Instagram users and have now shared their own experiences of feeling better after taking up the #fartwalk habit.
So what’s the evidence behind the fart walk? And what’s the best way to do it?
CandyBox Images/Shutterstock Exercise can help get the gas out
We know exercise can help relieve bloating by getting gas moving and out of our bodies.
Researchers from Barcelona, Spain in 2006 asked eight patients complaining of bloating, seven of whom had irritable bowel syndrome, to avoid “gassy” foods such as beans for two days and to fast for eight hours before their study.
Each patient was asked to sit in an armchair, in order to avoid any effects of body position on the movement of gas. Gas was pumped directly into their small bowel via a thin plastic tube that went down their mouth, and the gas expelled from the body was collected into a bag via a tube placed in the rectum. This way, the researchers could determine how much gas was retained in the gut.
The patients were then asked to pedal on a modified exercise bike while remaining seated in their armchairs.
The researchers found that much less gas was retained in the patients’ gut when they exercised. They determined exercise probably helped the movement and release of intestinal gas.
Walking may have another bonus; it may trigger a nerve reflex that helps propel foods and gas contents through the gut.
Walking can also increase internal abdominal pressure as you use your abdominal muscles to stay upright and balance as you walk. This pressure on the colon helps to push intestinal gas out.
Proper fart walk technique
One study from Iran studied the effects of walking in 94 individuals with bloating.
They asked participants to carry out ten to 15 minutes of slow walking (about 1,000 steps) after eating lunch and dinner. They filled out gut symptom questionnaires before starting the program and again at the end of the four week program.
The researchers found walking after meals resulted in improvements to gut symptoms such as belching, farting, bloating and abdominal discomfort.
Now for the crucial part: in the Iranian study, there was a particular way in which participants were advised to walk. They were asked to clasp hands together behind their back and to flex their neck forward.
The clasped hands posture leads to more internal abdominal pressure and therefore more gentle squeezing out of gas from the colon. The flexed neck posture decreases the swallowing of air during walking.
This therefore is the proper fart walk technique, based on science.
Could walking with your hands behind your back yield better or more farts? candy candy/Shutterstock What about constipation?
A fart walk can help with constipation.
One study involved middle aged inactive patients with chronic constipation, who did a 12 week program of brisk walking at least 30 minutes a day – combined with 11 minutes of strength and flexibility exercises.
This program, the researchers found, improved constipation symptoms through reduced straining, less hard stools and more complete evacuation.
It also appears that the more you walk the better the benefits for gut symptoms.
In patients with irritable bowel syndrome, one study increasing the daily step count to 9,500 steps from 4,000 steps led to a 50% reduction in the severity of their symptoms.
And just 30 minutes of a fart walk has been shown to improve blood sugar levels after eating.
Walking after eating can help keep your blood sugar levels under control. IndianFaces/Shutterstock What if I can’t get outside the house?
If getting outside the house after dinner is impossible, could you try walking slowly on a treadmill or around the house for 1,000 steps?
If not, perhaps you could borrow an idea from the Barcelona research: sit back in an armchair and pedal using a modified exercise bike. Any type of exercise is better than none.
Whatever you do, don’t be a couch potato! Research has found more leisure screen time is linked to a greater risk of developing gut diseases.
We also know physical inactivity during leisure time and eating irregular meals are linked to a higher risk of abdominal pain, bloating and altered bowel motions.
Try the fart walk today
It may not be for everyone but this simple physical activity does have good evidence behind it. A fart walk can improve common symptoms such as bloating, abdominal discomfort and constipation.
It can even help lower blood sugar levels after eating.
Will you be trying a fart walk today?
Vincent Ho, Associate Professor and clinical academic gastroenterologist, Western Sydney University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
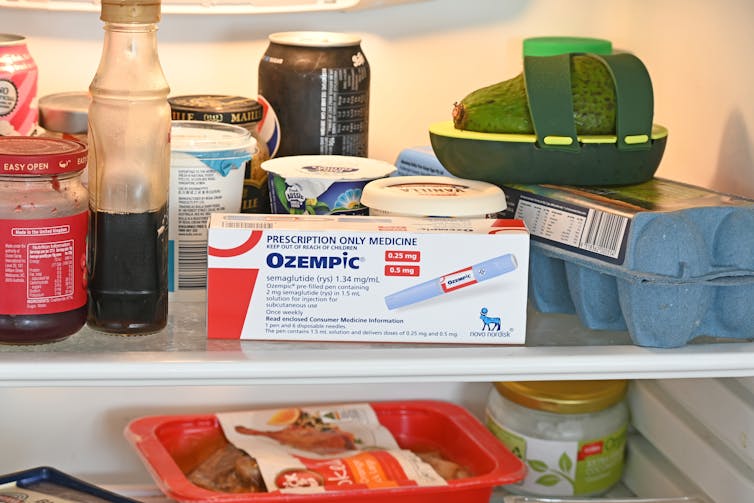
People on Ozempic may have fewer heart attacks, strokes and addictions – but more nausea, vomiting and stomach pain
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Ozempic and Wegovy are increasingly available in Australia and worldwide to treat type 2 diabetes and obesity.
The dramatic effects of these drugs, known as GLP-1s, on weight loss have sparked huge public interest in this new treatment option.
However, the risks and benefits are still being actively studied.
In a new study in Nature Medicine, researchers from the United States reviewed health data from about 2.4 million people who have type 2 diabetes, including around 216,000 people who used a GLP-1 drug, between 2017 and 2023.
The researchers compared a range of health outcomes when GLP-1s were added to a person’s treatment plan, versus managing their diabetes in other ways, often using glucose-lowering medications.
Overall, they found people who used GLP-1s were less likely to experience 42 health conditions or adverse health events – but more likely to face 19 others.
myskin/Shutterstock What conditions were less common?
Cardiometabolic conditions
GLP-1 use was associated with fewer serious cardiovascular and coagulation disorders. This includes deep vein thrombosis, pulmonary embolism, stroke, cardiac arrest, heart failure and myocardial infarction.
Neurological and psychiatric conditions
GLP-1 use was associated with fewer reported substance use disorders or addictions, psychotic disorders and seizures.
Infectious conditions
GLP-1 use was associated with fewer bacterial infections and pneumonia.
What conditions were more common?
Gastrointestinal conditions
Consistent with prior studies, GLP-1 use was associated with gastrointestinal conditions such as nausea, vomiting, gastritis, diverticulitis and abdominal pain.
Other adverse effects
Increased risks were seen for conditions such as low blood pressure, syncope (fainting) and arthritis.
People who took Ozempic were more likely to experience stomach upsets than those who used other type 2 diabetes treatments. Douglas Cliff/Shutterstock How robust is this study?
The study used a large and reputable dataset from the US Department of Veterans Affairs. It’s an observational study, meaning the researchers tracked health outcomes over time without changing anyone’s treatment plan.
A strength of the study is it captures data from more than 2.4 million people across more than six years. This is much longer than what is typically feasible in an intervention study.
Observational studies like this are also thought to be more reflective of the “real world”, because participants aren’t asked to follow instructions to change their behaviour in unnatural or forced ways, as they are in intervention studies.
However, this study cannot say for sure that GLP-1 use was the cause of the change in risk of different health outcomes. Such conclusions can only be confidently made from tightly controlled intervention studies, where researchers actively change or control the treatment or behaviour.
The authors note the data used in this study comes from predominantly older, white men so the findings may not apply to other groups.
Also, the large number of participants means that even very small effects can be detected, but they might not actually make a real difference in overall population health.
Observational studies track outcomes over time, but can’t say what caused the changes. Jacob Lund/Shutterstock Other possible reasons for these links
Beyond the effect of GLP-1 in the body, other factors may explain some of the findings in this study. For example, it’s possible that:
- people who used GLP-1 could be more informed about treatment options and more motivated to manage their own health
- people who used GLP-1 may have received it because their health-care team were motivated to offer the latest treatment options, which could lead to better care in other areas that impact the risk of various health outcomes
- people who used GLP-1 may have been able to do so because they lived in metropolitan centres and could afford the medication, as well as other health-promoting services and products, such as gyms, mental health care, or healthy food delivery services.
Did the authors have any conflicts of interest?
Two of the study’s authors declared they were “uncompensated consultants” for Pfizer, a global pharmaceutical company known for developing a wide range of medicines and vaccines. While Pfizer does not currently make readily available GLP-1s such as Ozempic or Wegovy, they are attempting to develop their own GLP-1s, so may benefit from greater demand for these drugs.
This research was funded by the US Department of Veterans Affairs, a government agency that provides a wide range of services to military veterans.
No other competing interests were reported.
Diabetes vs weight-loss treatments
Overall, this study shows people with type 2 diabetes using GLP-1 medication generally have more positive health outcomes than negative health outcomes.
However, the study didn’t include people without type 2 diabetes. More research is needed to understand the effects of these medications in people without diabetes who are using them for other reasons, including weight loss.
While the findings highlight the therapeutic benefits of GLP-1 medications, they also raise important questions about how to manage the potential risks for those who choose to use this medication.
The findings of this study can help many people, including:
- policymakers looking at ways to make GLP-1 medications more widely available for people with various health conditions
- health professionals who have regular discussions with patients considering GLP-1 use
- individuals considering whether a GLP-1 medication is right for them.
Lauren Ball, Professor of Community Health and Wellbeing, The University of Queensland and Emily Burch, Accredited Practising Dietitian and Lecturer, Southern Cross University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Could the shingles vaccine lower your risk of dementia?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A recent study has suggested Shingrix, a relatively new vaccine given to protect older adults against shingles, may delay the onset of dementia.
This might seem like a bizarre link, but actually, research has previously shown an older version of the shingles vaccine, Zostavax, reduced the risk of dementia.
In this new study, published last week in the journal Nature Medicine, researchers from the United Kingdom found Shingrix delayed dementia onset by 17% compared with Zostavax.
So how did the researchers work this out, and how could a shingles vaccine affect dementia risk?
Melinda Nagy/Shutterstock From Zostavax to Shingrix
Shingles is a viral infection caused by the varicella-zoster virus. It causes painful rashes, and affects older people in particular.
Previously, Zostavax was used to vaccinate against shingles. It was administered as a single shot and provided good protection for about five years.
Shingrix has been developed based on a newer vaccine technology, and is thought to offer stronger and longer-lasting protection. Given in two doses, it’s now the preferred option for shingles vaccination in Australia and elsewhere.
In November 2023, Shingrix replaced Zostavax on the National Immunisation Program, making it available for free to those at highest risk of complications from shingles. This includes all adults aged 65 and over, First Nations people aged 50 and older, and younger adults with certain medical conditions that affect their immune systems.
What the study found
Shingrix was approved by the US Food and Drugs Administration in October 2017. The researchers in the new study used the transition from Zostavax to Shingrix in the United States as an opportunity for research.
They selected 103,837 people who received Zostavax (between October 2014 and September 2017) and compared them with 103,837 people who received Shingrix (between November 2017 and October 2020).
By analysing data from electronic health records, they found people who received Shingrix had a 17% increase in “diagnosis-free time” during the follow-up period (up to six years after vaccination) compared with those who received Zostavax. This was equivalent to an average of 164 extra days without a dementia diagnosis.
The researchers also compared the shingles vaccines to other vaccines: influenza, and a combined vaccine for tetanus, diphtheria and pertussis. Shingrix and Zostavax performed around 14–27% better in lowering the risk of a dementia diagnosis, with Shingrix associated with a greater improvement.
The benefits of Shingrix in terms of dementia risk were significant for both sexes, but more pronounced for women. This is not entirely surprising, because we know women have a higher risk of developing dementia due to interplay of biological factors. These include being more sensitive to certain genetic mutations associated with dementia and hormonal differences.
Why the link?
The idea that vaccination against viral infection can lower the risk of dementia has been around for more than two decades. Associations have been observed between vaccines, such as those for diphtheria, tetanus, polio and influenza, and subsequent dementia risk.
Research has shown Zostavax vaccination can reduce the risk of developing dementia by 20% compared with people who are unvaccinated.
But it may not be that the vaccines themselves protect against dementia. Rather, it may be the resulting lack of viral infection creating this effect. Research indicates bacterial infections in the gut, as well as viral infections, are associated with a higher risk of dementia.
Notably, untreated infections with herpes simplex (herpes) virus – closely related to the varicella-zoster virus that causes shingles – can significantly increase the risk of developing dementia. Research has also shown shingles increases the risk of a later dementia diagnosis.
This isn’t the first time research has suggested a vaccine could reduce dementia risk. ben bryant/Shutterstock The mechanism is not entirely clear. But there are two potential pathways which may help us understand why infections could increase the risk of dementia.
First, certain molecules are produced when a baby is developing in the womb to help with the body’s development. These molecules have the potential to cause inflammation and accelerate ageing, so the production of these molecules is silenced around birth. However, viral infections such as shingles can reactivate the production of these molecules in adult life which could hypothetically lead to dementia.
Second, in Alzheimer’s disease, a specific protein called Amyloid-β go rogue and kill brain cells. Certain proteins produced by viruses such as COVID and bad gut bacteria have the potential to support Amyloid-β in its toxic form. In laboratory conditions, these proteins have been shown to accelerate the onset of dementia.
What does this all mean?
With an ageing population, the burden of dementia is only likely to become greater in the years to come. There’s a lot more we have to learn about the causes of the disease and what we can potentially do to prevent and treat it.
This new study has some limitations. For example, time without a diagnosis doesn’t necessarily mean time without disease. Some people may have underlying disease with delayed diagnosis.
This research indicates Shingrix could have a silent benefit, but it’s too early to suggest we can use antiviral vaccines to prevent dementia.
Overall, we need more research exploring in greater detail how infections are linked with dementia. This will help us understand the root causes of dementia and design potential therapies.
Ibrahim Javed, Enterprise and NHMRC Emerging Leadership Fellow, UniSA Clinical & Health Sciences, University of South Australia
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: