This Is Your Brain on Food – by Dr. Uma Naidoo
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
“Diet will fix your brain” is a bold claim that often comes from wishful thinking and an optimistic place where anecdote is louder than evidence. But, diet does incontrovertibly also affect brain health. So, what does Dr. Naidoo bring to the table?
The author is a Harvard-trained psychiatrist, a professional chef who graduated with her culinary school’s most coveted award, and a trained-and-certified nutritionist. Between those three qualifications, it’s safe to she knows her stuff when it comes to the niche that is nutritional psychiatry. And it shows.
She takes us through the neurochemistry involved, what chemicals are consumed, made, affected, inhibited, upregulated, etc, what passes through the blood-brain barrier and what doesn’t, what part the gut really plays in its “second brain” role, and how we can leverage that—as well as mythbusting a lot of popular misconceptions about certain foods and moods.
There’s hard science in here, but presented in quite a pop-science way, making for a very light yet informative read.
Bottom line: if you’d like to better understand what your food is doing to your brain (and what it could be doing instead), then this is a top-tier book for you!
Click here to check out This Is Your Brain On Food, and get to know yours!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
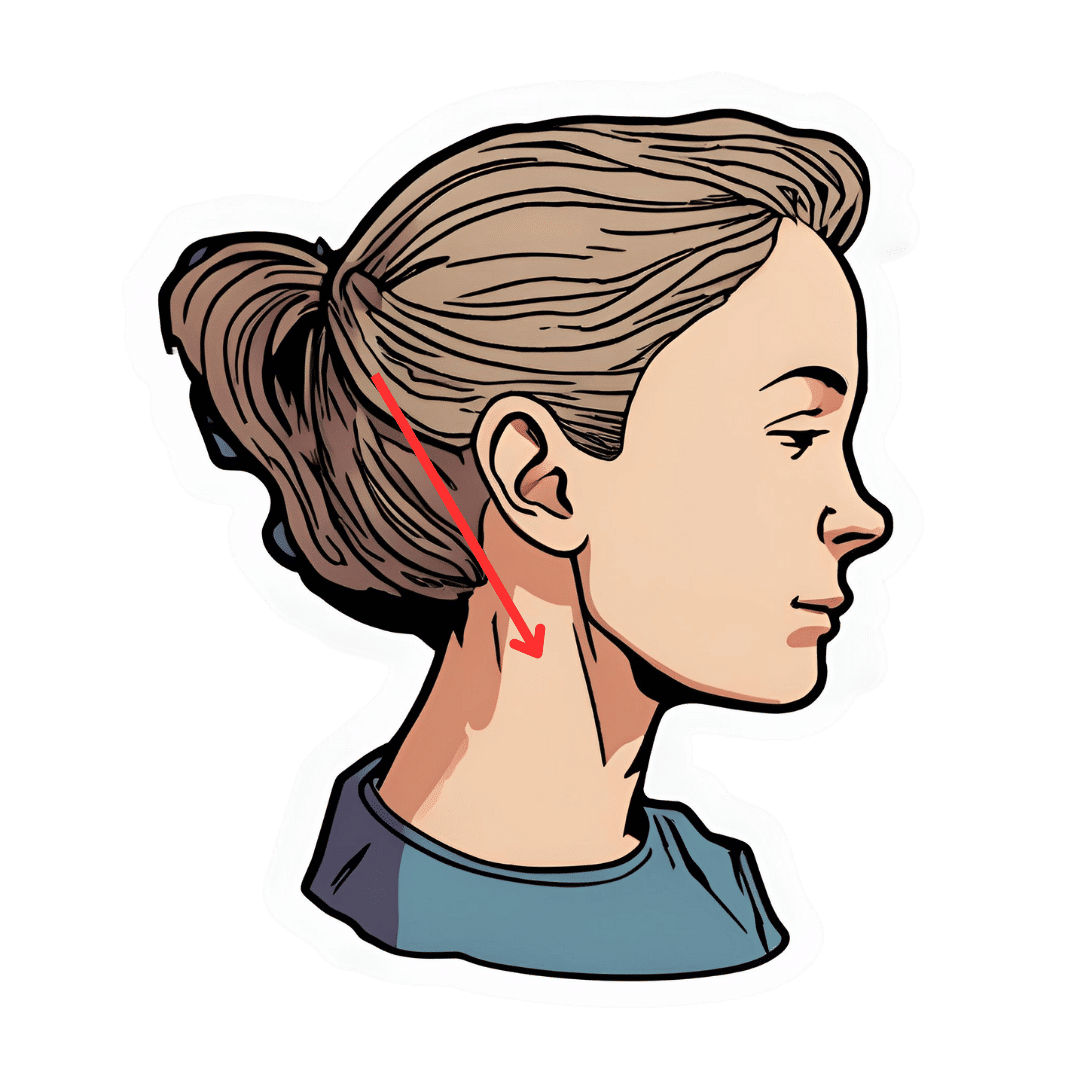
The Vagus Nerve’s Power for Weight Loss
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Arun Dhir is a university lecturer, a gastrointestinal surgeon, an author, and a yoga and meditation instructor, and he has this to say:
Gut feelings
The vagus nerve is the 10th cranial nerve, also known as “vagus” (“the wanderer”), because it travels from the brain to many other body parts, including the ears, throat, heart, respiratory system, gut, pancreas, liver, and reproductive system. It’s no surprise then, that it plays a key role in brain-gut communication and metabolism regulation.
The vagus nerve is part of the parasympathetic nervous system, responsible for rest, digestion, and counteracting the stress response. Most signals through the vagus nerve travel from the gut to the brain, though there is communication in both directions.
You may be beginning to see how this works and its implications for weight management: the vagus nerve senses metabolites from the liver, pancreas, and small intestine, and regulates insulin production by stimulating beta cells in the pancreas, which is important for avoiding/managing insulin resistance and metabolic syndrome in general.
Dr. Dhir cites a study in which vagus nerve stimulation (originally used for treating epilepsy and depression) was shown to cause unintentional weight loss (6-11%) in patients, revealing a link to weight management. Of course, that is quite a specific sample, so more research is needed to say for sure, but because the principle is very sound and the mechanism of action is clear, it’s not being viewed as a controversial conclusion.
As for how get these benefits, here are seven ways:
- Cold water on the face: submerge your face in cold water in the morning while holding water in your mouth, or cover your face with a cold wet washcloth (while holding your breath please; no need to waterboard yourself!), which activates the “mammalian dive response” in which your body activates the parasympathetic nervous system in order to remain calm and thus survive for longer underwater
- Alternate hot and cold showers: switch between hot and cold water during showers for 10-second intervals; this creates eustress and activates the process of hormesis, improving your overall stress management and reducing any chronic stress response you may otherwise have going on
- Humming and gargling: the vibrations in the throat stimulate the nearby vagus nerve
- Deep breathing (pranayama): yoga breathing exercises, especially combined with somatic exercises such as the sun salutation, can stimulate the vagus nerve
- Intermittent fasting: helps recalibrate the metabolism and indirectly improves vagus nerve function
- Massage and acupressure: stimulates lymphatic channels and the vagus nerve
- Long walks in nature (“forest bathing”): helps trigger relaxation in general
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
The Vagus Nerve (And How You Can Make Use Of It)
Take care!
Share This Post
-
Cost of living: if you can’t afford as much fresh produce, are canned veggies or frozen fruit just as good?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The cost of living crisis is affecting how we spend our money. For many people, this means tightening the budget on the weekly supermarket shop.
One victim may be fresh fruit and vegetables. Data from the Australian Bureau of Statistics (ABS) suggests Australians were consuming fewer fruit and vegetables in 2022–23 than the year before.
The cost of living is likely compounding a problem that exists already – on the whole, Australians don’t eat enough fruit and vegetables. Australian dietary guidelines recommend people aged nine and older should consume two serves of fruit and five serves of vegetables each day for optimal health. But in 2022 the ABS reported only 4% of Australians met the recommendations for both fruit and vegetable consumption.
Fruit and vegetables are crucial for a healthy, balanced diet, providing a range of vitamins and minerals as well as fibre.
If you can’t afford as much fresh produce at the moment, there are other ways to ensure you still get the benefits of these food groups. You might even be able to increase your intake of fruit and vegetables.
New Africa/Shutterstock Frozen
Fresh produce is often touted as being the most nutritious (think of the old adage “fresh is best”). But this is not necessarily true.
Nutrients can decline in transit from the paddock to your kitchen, and while the produce is stored in your fridge. Frozen vegetables may actually be higher in some nutrients such as vitamin C and E as they are snap frozen very close to the time of harvest. Variations in transport and storage can affect this slightly.
Minerals such as calcium, iron and magnesium stay at similar levels in frozen produce compared to fresh.
Another advantage to frozen vegetables and fruit is the potential to reduce food waste, as you can use only what you need at the time.
Freezing preserves the nutritional quality of vegetables and increases their shelf life. Tohid Hashemkhani/Pexels As well as buying frozen fruit and vegetables from the supermarket, you can freeze produce yourself at home if you have an oversupply from the garden, or when produce may be cheaper.
A quick blanching prior to freezing can improve the safety and quality of the produce. This is when food is briefly submerged in boiling water or steamed for a short time.
Frozen vegetables won’t be suitable for salads but can be eaten roasted or steamed and used for soups, stews, casseroles, curries, pies and quiches. Frozen fruits can be added to breakfast dishes (with cereal or youghurt) or used in cooking for fruit pies and cakes, for example.
Canned
Canned vegetables and fruit similarly often offer a cheaper alternative to fresh produce. They’re also very convenient to have on hand. The canning process is the preservation technique, so there’s no need to add any additional preservatives, including salt.
Due to the cooking process, levels of heat-sensitive nutrients such as vitamin C will decline a little compared to fresh produce. When you’re using canned vegetables in a hot dish, you can add them later in the cooking process to reduce the amount of nutrient loss.
To minimise waste, you can freeze the portion you don’t need.
Fermented
Fermented vegetables are another good option. Angela Khebou/Unsplash Fermentation has recently come into fashion, but it’s actually one of the oldest food processing and preservation techniques.
Fermentation largely retains the vitamins and minerals in fresh vegetables. But fermentation may also enhance the food’s nutritional profile by creating new nutrients and allowing existing ones to be absorbed more easily.
Further, fermented foods contain probiotics, which are beneficial for our gut microbiome.
5 other tips to get your fresh fix
Although alternatives to fresh such as canned or frozen fruit and vegetables are good substitutes, if you’re looking to get more fresh produce into your diet on a tight budget, here are some things you can do.
1. Buy in season
Based on supply and demand principles, buying local seasonal vegetables and fruit will always be cheaper than those that are imported out of season from other countries.
2. Don’t shun the ugly fruit and vegetables
Most supermarkets now sell “ugly” fruit and vegetables, that are not physically perfect in some way. This does not affect the levels of nutrients in them at all, or their taste.
Buying fruit and vegetables during the right season will be cheaper. August de Richelieu/Pexels 3. Reduce waste
On average, an Australian household throws out A$2,000–$2,500 worth of food every year. Fruit, vegetables and bagged salad are the three of the top five foods thrown out in our homes. So properly managing fresh produce could help you save money (and benefit the environment).
To minimise waste, plan your meals and shopping ahead of time. And if you don’t think you’re going to get to eat the fruit and vegetables you have before they go off, freeze them.
4. Swap and share
There are many websites and apps which offer the opportunity to swap or even pick up free fresh produce if people have more than they need. Some local councils are also encouraging swaps on their websites, so dig around and see what you can find in your local area.
5. Gardening
Regardless of how small your garden is you can always plant produce in pots. Herbs, rocket, cherry tomatoes, chillies and strawberries all grow well. In the long run, these will offset some of your cost on fresh produce.
Plus, when you have put the effort in to grow your own produce, you are less likely to waste it.
Evangeline Mantzioris, Program Director of Nutrition and Food Sciences, Accredited Practising Dietitian, University of South Australia
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
How To Engage Your Whole Brain
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Stroke Of Insight That Nobody Wants
This is Dr. Jill Bolte Taylor. She’s a neuroanatomist, who, at the age of 37 (when she was a post-doctoral fellow at Harvard Medical School), had what she refers to as her “stroke of insight”.
That is to say, she had a massive stroke, and after a major brain surgery to remove a clot the size of a golf ball, she spent the next 8 years re-learning to do everything.
Whereas previously she’d been busy mapping the brain to determine how cells communicate with each other, now she was busy mapping whether socks or shoes should go on first. Needless to say, she got an insight into neuroplasticity that few people would hope for.
What does she want us to know?
Dr. Taylor (now once again a successful scientist, lecturer, and author) advocates for “whole brain living”, which involves not taking parts of our brain for granted.
About those parts…
Dr. Taylor wants us to pay attention to all the parts regardless of size, ranging from the two hemispheres, all the way down to the billions of brain cells, and yet even further, to the “trillions of molecular geniuses”—because each brain cell is itself reliant on countless molecules of the many neurochemicals that make up our brain.
For a quick refresher on some of the key players in that latter category, see our Neurotransmitter Cheatsheet 😎
When it comes to the hemispheres, there has historically been a popular belief that these re divided into:
- The right brain: emotional, imaginative, creative, fluid feeling
- The left brain: intellectual, analytical, calculating, crystal thinking
…which is not true, anatomically speaking, because there are cells on both sides doing their part of both of these broad categories of brain processes.
However, Dr. Taylor found, while one hemisphere of her brain was much more damaged than the other, that nevertheless she could recover some functions more quickly than others, which, once she was able to resume her career, inspired her model of four distinct ways of cogitating that can be switched-between and played with or against each other:
Meet The Four Characters Inside Your Brain
Why this matters
As she was re-learning everything, the way forward was not quick or easy, and she also didn’t know where she was going, because for obvious reasons, she couldn’t remember, much less plan.
Looking backwards after her eventual full recovery, she noted a lot of things that she needed during that recovery, some of which she got and some of which she didn’t.
Most notably for her, she needed the right kind of support that would allow all four of the above “characters” as she puts it, to thrive and grow. And, when we say “grow” here we mean that literally, because of growing new brain cells to replace the lost ones (as well as the simple ongoing process of slowly replacing brain cells).
For more on growing new brain cells, by the way, see:
How To Grow New Brain Cells (At Any Age)
In order to achieve this in all of the required brain areas (i.e., and all of the required brain functions), she also wants us to know… drumroll please…
When to STFU
Specifically, the ability to silence parts of our brain that while useful in general, aren’t necessarily being useful right now. Since it’s very difficult to actively achieve a negative when it comes to brain-stuff (don’t think of an elephant), this means scheduling time for other parts of our brain to be louder. And that includes:
- scheduling time to feel (emotionally)
- scheduling time to feel (gut feelings)
- scheduling time to feel (kinesthetically)
…amongst others.
Note: those three are presented in that order, from least basic to most basic. And why? Because, clever beings that we are, we typically start from a position that’s not remotely basic, such as “overthinking”, for example. So, there’s a wind-down through thinking just the right amount, thinking through simpler concepts, feeling, noticing one’s feelings, noticing noticing one’s feelings, all the way down to what, kinesthetically, are we actually physically feeling.
❝It is interesting to note that although our limbic system fucntions throughout our lifetime, it does not mature. As a result, when our emotional “buttons” are pushed, we retain the ability to react to incoming stimulation as though we were a two-year-old, even when we are adults.❞
~ Dr. Jill Taylor
Of course, sometimes the above is not useful, which is why the ability to switch between brain modes is a very important and useful skill to develop.
And how do we do that? By practising. Which is something that it’s necessary to take up consciously, and pursue consistently. When children are at school, there are (hopefully, ideally) curricula set out to ensure they engage and train all parts of their brain. As adults, this does not tend to get the same amount of focus.
“Children’s brains are still developing”—indeed, and so are adult brains:
The Brain As A Work-In-Progress
Dr. Taylor had the uncommon experience of having to, in many ways, neurologically speaking, redo childhood. And having had a second run at it, she developed an appreciation of the process that most of us didn’t necessarily get when doing childhood just the once.
In other words: take the time to feel stuff; take the time to quiet down your chatty mind, take the time engage your senses, and take it seriously! Really notice, as though for the first time, what the texture of your carpet is like. Really notice, as though for the first time, what it feels like to swallow some water. Really notice, as though for the first time, what it feels like to experience joy—or sadness, or comfort, or anger, or peace. Exercise your imagination. Make some art (it doesn’t have to win awards; it just has to light up your brain!). Make music (again, it’s about wiring your brain in your body, not about outdoing Mozart in composition and/or performance). Make changes! Make your brain work in the ways it’s not in the habit of doing.
If you need a little help switching off parts of your brain that are being too active, so that you can better exercise other parts of your brain that might otherwise have been neglected, you might want to try:
Enjoy!
Share This Post
Related Posts
-
Seven and a Half Lessons About the Brain – by Dr. Lisa Feldman Barrett
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve reviewed books about neurology before, and we always try to review books that bring something new/different. So, what makes this one stand out?
Dr. Lisa Feldman Barrett, one of the world’s foremost neuroscientists, starts with an overview of how our unusual brain (definitely our species’ defining characteristic) came to be, and then devotes the rest of the book to mostly practical information.
She explains, in clear terms and without undue jargon, how the brain goes about such things as making constant predictions and useful assumptions about our environment, and reports these things to us as facts—which process is usually useful, and sometimes counterproductive.
We learn about how the apparently mystical trait of empathy works, in real flesh-and-blood terms, and why some kinds of empathy are more metabolically costly than others, and what that means for us all.
Unlike many such books, this one also looks at what is going on in the case of “different minds” that operate very dissimilarly to our own, and how this neurodiversity is important for our species.
Critically, she also looks at what else makes our brains stand out, the symphony of “5 Cs” that aren’t often found to the same extent all in the same species: creativity, communication, copying, cooperation, and compression. This latter being less obvious, but perhaps the most important; Dr. Feldman Barrett explains how we use this ability to layer summaries of our memories, perceptions, and assumptions, to allow us to think in abstractions—something that powers much of what we do that separates us from other animals.
Bottom line: if you’d like to learn more about that big wet organ between your ears, what it does for you, and how it goes about doing it, then this book gives a very practical foundation from which to build.
Click here to check out Seven and a Half Lessons about the Brain, and learn more about yours!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
7 Principles of Becoming a Leader – by Riku Vuorenmaa
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We urge you to overlook the cliché cover art (we don’t know what they were thinking, going for the headless suited torso) because…
This one could be the best investment you make in your career this year! You may be wondering what the titular 7 principles are. We won’t keep you guessing; they are:
- Professional development: personal excellence, productivity, and time management
- Leadership development: mindset and essential leadership skills
- Personal development: your motivation, character, and confidence as a leader
- Career management: plan your career, get promoted and paid well
- Social skills & networking: work and connect with the right people
- Business- & company-understanding: the big picture
- Commitment: make the decision and commit to becoming a great leader
A lot of leadership books repeat the same old fluff that we’ve all read many times before… padded with a lot of lengthy personal anecdotes and generally editorializing fluff. Not so here!
While yes, this book does also cover some foundational things first, it’d be remiss not to. It also covers a whole (much deeper) range of related skills, with down-to-earth, brass tacks advice on putting them into practice.
This is the kind of book you will want to set as a recurring reminder in your phone, to re-read once a year, or whatever schedule seems sensible to you.
There aren’t many books we’d put in that category!
Pick Up Your Copy of the “7 Principles of Becoming a Leader” on Amazon Today!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Resveratrol & Healthy Aging
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Resveratrol & Healthy Aging
Resveratrol is the compound found in red grapes, and thus in red wine, that have resulted in red wine being sometimes touted as a heart-healthy drink.
However, at the levels contained in red wine, you’d need to drink 100–1000 glasses of wine per day (depending on the wine) to get the dose of resveratrol that was associated with heart health benefits in mouse studies.
Which also means: if you are not a mouse, you might need to drink even more than that!
Further reading: can we drink to good health?
Resveratrol supplementation
Happily, resveratrol supplements exist. But what does resveratrol do?
It lowers blood pressure:
Effect of resveratrol on blood pressure: a meta-analysis of randomized controlled trials
It improves blood lipid levels:
It improves insulin sensitivity:
It has neuroprotective effects too:
Resveratrol promotes clearance of Alzheimer’s disease amyloid-beta peptides
Is it safe?
For most people, it is generally recognized as safe. However, if you are on blood-thinners or otherwise have a bleeding disorder, you might want to skip it:
Antiplatelet activity of synthetic and natural resveratrol in red wine
You also might want to check with your pharmacist/doctor, if you’re on blood pressure meds, anxiety meds, or immunosuppressants, as it can increase the amount of these drugs that will then stay in your system:
Resveratrol modulates drug- and carcinogen-metabolizing enzymes in a healthy volunteer study
And as ever, of course, if unsure just check with your pharmacist/doctor, to be on the safe side.
Where to get it?
We don’t sell it, but here’s an example product on Amazon for your convenience
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: