Could the shingles vaccine lower your risk of dementia?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A recent study has suggested Shingrix, a relatively new vaccine given to protect older adults against shingles, may delay the onset of dementia.
This might seem like a bizarre link, but actually, research has previously shown an older version of the shingles vaccine, Zostavax, reduced the risk of dementia.
In this new study, published last week in the journal Nature Medicine, researchers from the United Kingdom found Shingrix delayed dementia onset by 17% compared with Zostavax.
So how did the researchers work this out, and how could a shingles vaccine affect dementia risk?

From Zostavax to Shingrix
Shingles is a viral infection caused by the varicella-zoster virus. It causes painful rashes, and affects older people in particular.
Previously, Zostavax was used to vaccinate against shingles. It was administered as a single shot and provided good protection for about five years.
Shingrix has been developed based on a newer vaccine technology, and is thought to offer stronger and longer-lasting protection. Given in two doses, it’s now the preferred option for shingles vaccination in Australia and elsewhere.
In November 2023, Shingrix replaced Zostavax on the National Immunisation Program, making it available for free to those at highest risk of complications from shingles. This includes all adults aged 65 and over, First Nations people aged 50 and older, and younger adults with certain medical conditions that affect their immune systems.
What the study found
Shingrix was approved by the US Food and Drugs Administration in October 2017. The researchers in the new study used the transition from Zostavax to Shingrix in the United States as an opportunity for research.
They selected 103,837 people who received Zostavax (between October 2014 and September 2017) and compared them with 103,837 people who received Shingrix (between November 2017 and October 2020).
By analysing data from electronic health records, they found people who received Shingrix had a 17% increase in “diagnosis-free time” during the follow-up period (up to six years after vaccination) compared with those who received Zostavax. This was equivalent to an average of 164 extra days without a dementia diagnosis.
The researchers also compared the shingles vaccines to other vaccines: influenza, and a combined vaccine for tetanus, diphtheria and pertussis. Shingrix and Zostavax performed around 14–27% better in lowering the risk of a dementia diagnosis, with Shingrix associated with a greater improvement.
The benefits of Shingrix in terms of dementia risk were significant for both sexes, but more pronounced for women. This is not entirely surprising, because we know women have a higher risk of developing dementia due to interplay of biological factors. These include being more sensitive to certain genetic mutations associated with dementia and hormonal differences.
Why the link?
The idea that vaccination against viral infection can lower the risk of dementia has been around for more than two decades. Associations have been observed between vaccines, such as those for diphtheria, tetanus, polio and influenza, and subsequent dementia risk.
Research has shown Zostavax vaccination can reduce the risk of developing dementia by 20% compared with people who are unvaccinated.
But it may not be that the vaccines themselves protect against dementia. Rather, it may be the resulting lack of viral infection creating this effect. Research indicates bacterial infections in the gut, as well as viral infections, are associated with a higher risk of dementia.
Notably, untreated infections with herpes simplex (herpes) virus – closely related to the varicella-zoster virus that causes shingles – can significantly increase the risk of developing dementia. Research has also shown shingles increases the risk of a later dementia diagnosis.

The mechanism is not entirely clear. But there are two potential pathways which may help us understand why infections could increase the risk of dementia.
First, certain molecules are produced when a baby is developing in the womb to help with the body’s development. These molecules have the potential to cause inflammation and accelerate ageing, so the production of these molecules is silenced around birth. However, viral infections such as shingles can reactivate the production of these molecules in adult life which could hypothetically lead to dementia.
Second, in Alzheimer’s disease, a specific protein called Amyloid-β go rogue and kill brain cells. Certain proteins produced by viruses such as COVID and bad gut bacteria have the potential to support Amyloid-β in its toxic form. In laboratory conditions, these proteins have been shown to accelerate the onset of dementia.
What does this all mean?
With an ageing population, the burden of dementia is only likely to become greater in the years to come. There’s a lot more we have to learn about the causes of the disease and what we can potentially do to prevent and treat it.
This new study has some limitations. For example, time without a diagnosis doesn’t necessarily mean time without disease. Some people may have underlying disease with delayed diagnosis.
This research indicates Shingrix could have a silent benefit, but it’s too early to suggest we can use antiviral vaccines to prevent dementia.
Overall, we need more research exploring in greater detail how infections are linked with dementia. This will help us understand the root causes of dementia and design potential therapies.
Ibrahim Javed, Enterprise and NHMRC Emerging Leadership Fellow, UniSA Clinical & Health Sciences, University of South Australia
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Stop Checking Your Likes – by Susie Moore
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
You might think this one’s advice is summed up sufficiently by the title, that there’s no need for a book! But…
There’s a lot more to this than “stop comparing the worst out-takes of your life to someone else’s highlight reel”, and there’s a lot more to this than “just unplug”.
Instead, Susie Moore discusses the serious underlying real emotional considerations of the need for approval (and even just acceptance) by our community, as well the fear of missing out.
It’s not just about how social media is designed to hijack various parts of our brain, or how The Alogorithm™ is out to personally drag your soul through Hell for a few more clicks; it’s also about the human element that would exist even without that. Who remembers MySpace? No algorithm in those days, but oh the drama potential for those “top 8 friends” places. And if you think that kind of problem is just for young people 20 years ago, you have mercifully missed the drama that older generations can get into on Facebook.
Along with the litany of evil, though, Moore also gives practical advice on how to overcome those things, how to “see the world through comedy-colored glasses”, how to ask “what’s missing, really?”, and how to make your social media experience work for you, rather than it merely using you as fuel. ← link is to our own related article!
Bottom line: if social media sucks a lot of your time, there may be more to it than just “social media sucks in general”, and there are ways to meet your emotional needs without playing by corporations’ rules to do so.
Click here to check out Stop Checking Your Likes, and breathe easy!
Share This Post
-
Genetic Risk Factors For Long COVID
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Some people, after getting COVID, go on to have Long COVID. There are various contributing factors to this, including:
- Lifestyle factors that impact general disease-proneness
- Immune-specific factors such as being immunocompromised already
- Genetic factors
We looked at some modifiable factors to improve one’s disease-resistance, yesterday:
And we’ve taken a more big-picture look previously:
Beyond Supplements: The Real Immune-Boosters!
Along with some more systemic issues:
Why Some People Get Sick More (And How To Not Be One Of Them)
But, for when the “don’t get COVID” ship has sailed, one of the big remaining deciding factors with regard to whether one gets Long COVID or not, is genetic
The Long COVID Genes
For those with their 23andMe genetic data to hand…
❝Study findings revealed that three specific genetic loci, HLA-DQA1–HLA-DQB1, ABO, and BPTF–KPAN2–C17orf58, and three phenotypes were at significantly heightened risk, highlighting high-priority populations for interventions against this poorly understood disease.❞
For those who don’t, then first: you might consider getting that! Here’s why:
Genetic Testing: Health Benefits & Methods
But also, all is not lost meanwhile:
The same study also found that individuals with genetic predispositions to chronic fatigue, depression, and fibromyalgia, as well as other phenotypes such as autoimmune conditions and cardiometabolic conditions, are at significantly higher risk of long-COVID than individuals without these conditions.
Good news, bad news
Another finding was that women and non-smokers were more likely to get Long COVID, than men and smokers, respectively.
Does that mean that those things are protective against Long COVID, which would be very counterintuitive in the case of smoking?
Well, yes and no; it depends on whether you count “less likely to get Long COVID because of being more likely to just die” as protective against Long COVID.
(Incidentally, estrogen is moderately immune-enhancing, while testosterone is moderately immune-suppressing, so the sex thing was not too surprising. It’s also at least contributory to why women get more autoimmune disorders, while men get more respiratory infections such as colds and the like)
Want to know more?
You can read the paper itself, here:
*GWAS = Genome-Wide Association Study
Take care!
Share This Post
-
The Many Health Benefits Of Garlic
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Many Health Benefits of Garlic
We’re quite confident you already know what garlic is, so we’re going to leap straight in there with some science today:
First, let’s talk about allicin
Allicin is a compound in garlic that gives most of its health benefits. A downside of allicin is that it’s not very stable, so what this means is:
- Garlic is best fresh—allicin breaks down soon after garlic is cut/crushed
- So while doing the paperwork isn’t fun, buying it as bulbs is better than buying it as granules or similar
- Allicin also breaks down somewhat in cooking, so raw garlic is best
- Our philosophy is: still use it in cooking as well; just use more!
- Supplements (capsule form etc) use typically use extracts and potency varies (from not great to actually very good)
Read more about that:
- Short-term heating reduces the anti-inflammatory effects of fresh raw garlic extracts
- Allicin Bioavailability and Bioequivalence from Garlic Supplements and Garlic Foods
Now, let’s talk benefits…
Benefits to heart health
Garlic has been found to be as effective as the drug Atenolol at reducing blood pressure:
It also lowers LDL (bad cholesterol):
Benefits to the gut
We weren’t even looking for this, but as it turns out, as an add-on to the heart benefits…
Benefits to the immune system
Whether against the common cold or bringing out the heavy guns, garlic is a booster:
- Preventing the common cold with a garlic supplement: a double-blind, placebo-controlled survey
- Supplementation with aged garlic extract improves both NK and γδ-T cell function and reduces the severity of cold and flu symptoms: a randomized, double-blind, placebo-controlled nutrition intervention
Benefits to the youthfulness of body and brain
Garlic is high in antioxidants that, by virtue of reducing oxidative stress, help slow aging. This effect, combined with the cholesterol and blood pressure benefits, means it may also reduce the risk of Alzheimer’s and other forms of dementia:
- Antioxidant health effects of aged garlic extract
- Effects of garlic consumption on plasma and erythrocyte antioxidant parameters in elderly subjects
- Garlic reduces heart disease and dementia risk
There are more benefits too…
That’s all we have time to dive into study-wise today, but for the visually-inclined, here are yet more benefits to garlic (at a rate of 3–4 cloves per day):
An incredible awesome recipe using lots of garlic:
- Take small potatoes (still in their skins), cut in half
- Add enough peeled cloves of garlic so that you have perhaps a 1:10 ratio of garlic to potato by mass
- Boil (pressure-cooking is ideal) until soft, and drain
- Keeping them in the pan, add a lashing of olive oil, and any additional seasonings per your preference (consider black pepper, rosemary, thyme, parsley)
- Put a lid on the pan, and holding it closed, shake the pan vigorously
- Note: if you didn’t leave the skins on, or you chopped much larger potatoes smaller instead of cutting in half, the potatoes will break up into a rough mash now. This is actually also fine and still tastes (and honestly, looks) great, but it is different, so just be aware, so that you get the outcome you want.
- The garlic, which—unlike the potatoes—didn’t have a skin to hold it together, will now have melted over the potatoes like butter
You can serve like this (it’s delicious already) or finish up in the oven or air-fryer or under the grill, if you prefer a roasted style dish (an amazing option too).
Share This Post
- Garlic is best fresh—allicin breaks down soon after garlic is cut/crushed
Related Posts
-
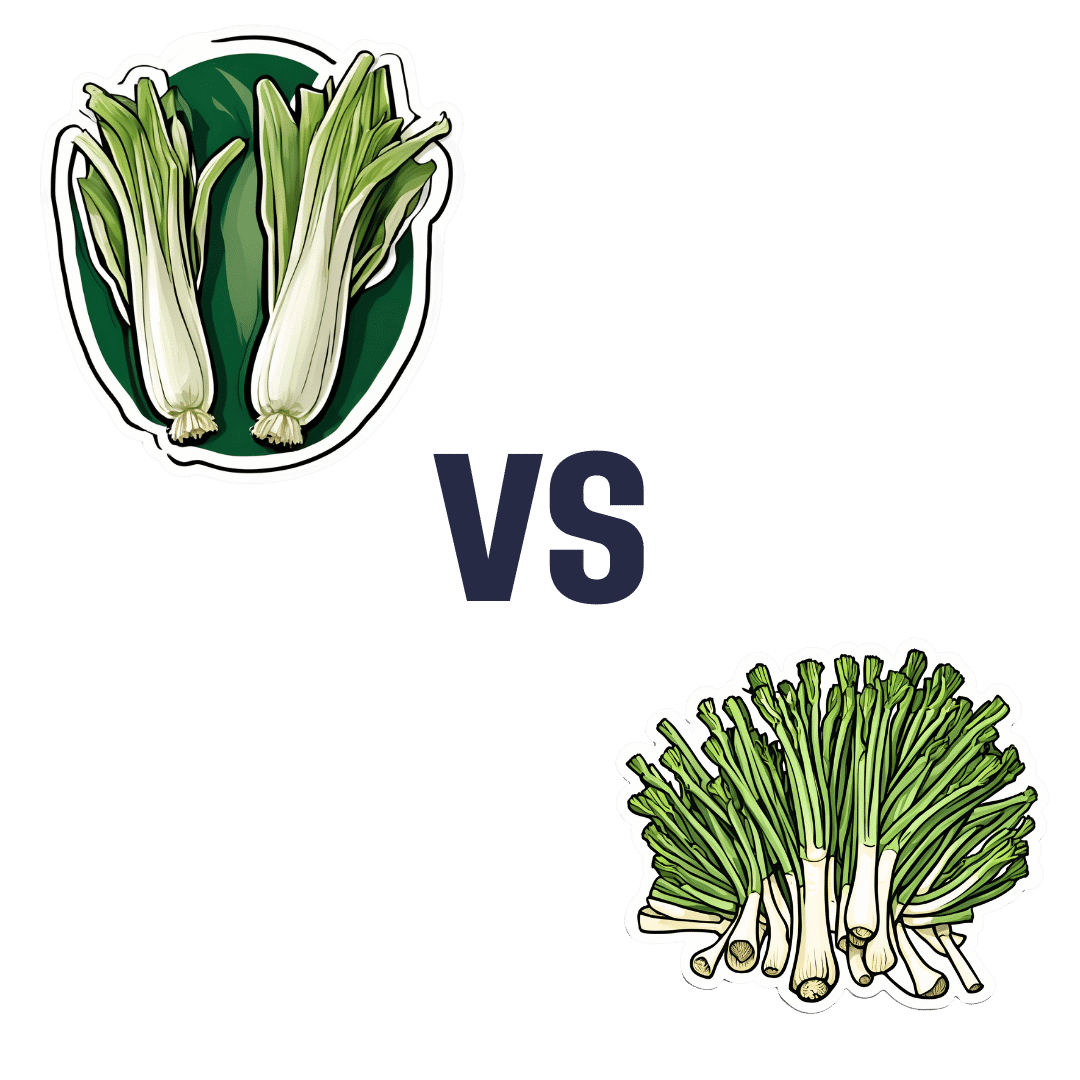
Leek vs Scallions – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing leek to scallions, we picked the leek.
Why?
In terms of macros, scallions might have a point: scallions have the lower glycemic index, thanks to leek having more carbs for the same amount of fiber. That said, leek already has a low glycemic index, so this is not a big deal.
When it comes to vitamins, leek has more of vitamins B1, B2, B3, B5, B6, B9, E, and choline, while scallions have more of vitamins A, C, and K. Noteworthily, a cup of chopped leek already provides the daily dose of vitamins A and K, and the difference in levels of vitamin C is minimal. All in all, an easy 8:3 win for leeks here, even without taking that into account.
In the category of minerals, leek has more calcium, copper, iron, magnesium, manganese, phosphorus, potassium, and selenium, while scallions have a little more zinc.
Both of these allium-family plants (i.e., related to garlic) have an abundance of polyphenols, especially kaempferol.
Of course, enjoy whatever goes best with your meal, but if you’re looking for nutritional density, then leek is where it’s at.
Want to learn more?
You might like to read:
The Many Health Benefits Of Garlic
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Thinking about cosmetic surgery? New standards will force providers to tell you the risks and consider if you’re actually suitable
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
People considering cosmetic surgery – such as a breast augmentation, liposuction or face lift – should have extra protection following the release this week of new safety and quality standards for providers, from small day-clinics through to larger medical organisations.
The new standards cover issues including how these surgeries are advertised, psychological assessments before surgery, the need for people to be informed of risks associated with the procedure, and the type of care people can expect during and afterwards. The idea is for uniform standards across Australia.
The move is part of sweeping reforms of the cosmetic surgery industry and the regulation of medical practitioners, including who is allowed to call themselves a surgeon.
It is heartening to see these reforms, but some may say they should have come much sooner for what’s considered a highly unregulated area of medicine.
Why do people want cosmetic surgery?
Australians spent an estimated A$473 million on cosmetic surgery procedures in 2023.
The major reason people want cosmetic surgery relates to concerns about their body image. Comments from their partners, friends or family about their appearance is another reason.
The way cosmetic surgery is portrayed on social media is also a factor. It’s often portrayed as an “easy” and “accessible” fix for concerns about someone’s appearance. So such aesthetic procedures have become far more normalised.
The use of “before” and “after” images online is also a powerful influence. Some people may think their appearance is worse than the “before” photo and so they think cosmetic intervention is even more necessary.
People don’t always get the results they expect
Most people are satisfied with their surgical outcomes and feel better about the body part that was previously concerning them.
However, people have often paid a sizeable sum of money for these surgeries and sometimes experienced considerable pain as they recover. So a positive evaluation may be needed to justify these experiences.
People who are likely to be unhappy with their results are those with unrealistic expectations for the outcomes, including the recovery period. This can occur if people are not provided with sufficient information throughout the surgical process, but particularly before making their final decision to proceed.
What’s changing?
According to the new standards, services need to ensure their own advertising is not misleading, does not create unreasonable expectations of benefits, does not use patient testimonials, and doesn’t offer any gifts or inducements.
For some clinics, this will mean very little change as they were not using these approaches anyway, but for others this may mean quite a shift in their advertising strategy.
It will likely be a major challenge for clinics to monitor all of their patient communication to ensure they adhere to the standards.
It is also not quite clear how the advertising standards will be monitored, given the expanse of the internet.
What about the mental health assessment?
The new standards say clinics must have processes to ensure the assessment of a patient’s general health, including psychological health, and that information from a patient’s referring doctor be used “where available”.
According to the guidelines from the Medical Board of Australia, which the standards are said to complement, all patients must have a referral, “preferably from their usual general practitioner or if that is not possible, from another general practitioner or other specialist medical practitioner”.
While this is a step in the right direction, we may be relying on medical professionals who may not specialise in assessing body image concerns and related mental health conditions. They may also have had very little prior contact with the patient to make their clinical impressions.
So these doctors need further training to ensure they can perform assessments efficiently and effectively. People considering surgery may also not be forthcoming with these practitioners, and may view them as “gatekeepers” to surgery they really want to have.
Ideally, mental health assessments should be performed by health professionals who are extensively trained in the area. They also know what other areas should be explored with the patient, such as the potential impact of trauma on body image concerns.
Of course, there are not enough mental health professionals, particularly psychologists, to conduct these assessments so there is no easy solution.
Ultimately, this area of health would likely benefit from a standard multidisciplinary approach where all health professionals involved (such as the cosmetic surgeon, general practitioner, dermatologist, psychologist) work together with the patient to come up with a plan to best address their bodily concerns.
In this way, patients would likely not view any of the health professionals as “gatekeepers” but rather members of their treating team.
If you’re considering cosmetic surgery
The Australian Commission on Safety and Quality in Health Care, which developed the new standards, recommended taking these four steps if you’re considering cosmetic surgery:
-
have an independent physical and mental health assessment before you commit to cosmetic surgery
-
make an informed decision knowing the risks
-
choose your practitioner, knowing their training and qualifications
-
discuss your care after your operation and where you can go for support.
My ultimate hope is people safely receive the care to help them best overcome their bodily concerns whether it be medical, psychological or a combination.
Gemma Sharp, Associate Professor, NHMRC Emerging Leadership Fellow & Senior Clinical Psychologist, Monash University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
-
Butter vs Margarine
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Butter vs Margarine
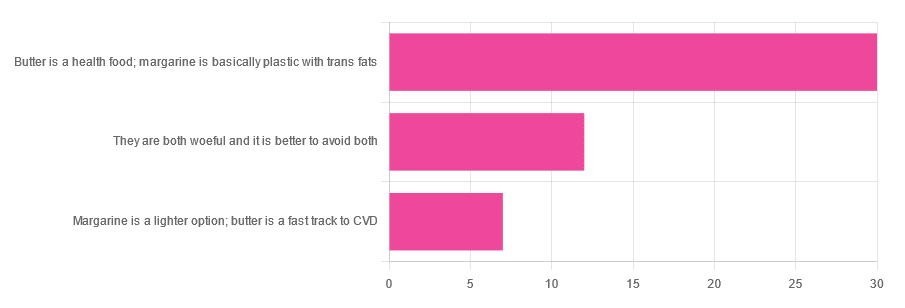
Yesterday, we asked you for your (health-related) opinion on butter vs margarine, and got the above-depicted, below-described, set of responses:
- A little over 60% said butter is a health food and margarine is basically plastic with trans fats
- A little over 20% said that both are woeful and it’s better to avoid both
- A little over 10% said that margarine is a lighter option, and butter is a fast track to cardiovascular disease.
Comments included (we will summarize/paraphrase, for space):
- “…in moderation, though”
- “I’m vegan so I use vegan butter but I know it’s not great, so I use it sparingly”
- “butter is healthy if and only if it’s grass-fed”
- “margarine has unpronounceable ingredients”
To address those quickly:
- “…in moderation” is a stipulation with which one can rarely go too far wrong
- Same! Speaking for myself (your writer here, hi) and not for the company
- Grass-fed is indeed better; alas that so little of it is grass-fed, in the US!
- Butter contains eicosatrienoic acid, linolelaidic acid, and more*. Sometimes big words don’t mean that something is worse for the health, though!
So, what does the science say?
Butter is a health food: True or False?
True or False, depending on amount! Moderation is definitely key, but we’ll return to that (and why not to have more than a small amount of butter) later. But it is a rich source of many nutrients, iff it’s grass-fed, anyway.
The nutritional profile of something isn’t a thing that’s too contentious, so rather than take too much time on it, in this case we’ll point you back up to the scientific paper we linked above, or if you prefer a pop-science rendering, here’s a nice quick rundown:
7 Reasons to Switch to Grass-Fed Butter
Margarine is basically plastic with trans fats: True or False?
False and usually False now, respectively, contingently.
On the first part: chemically, it’s simply not “basically plastic” and everything in it is digestible
On the second part: it depends on the margarine, and here’s where it pays to read labels. Historically, margarines all used to be high in trans fats (which are indeed woeful for the health). Nowadays, since trans fats have such a (well-earned) bad press, there are increasingly many margarines with low (or no) trans fats, and depending on your country, it may be that all margarines no longer have such:
❝It’s a public health success story. Consumers no longer have to worry about reading product nutritional labels to see if they contain hydrogenated oils and trans fats. They can just know that they no longer do❞
Source: Margarines now nutritionally better than butter after hydrogenated oil ban
So this is one where the science is clear (trans fats are unequivocally bad), but the consumer information is not always (it may be necessary to read labels, to know whether a margarine is conforming to the new guidelines).
Butter is a fast track to cardiovascular disease: True or False?
True or False depending on amount. In moderation, predictably it’s not a big deal.
But for example, the World Health Organization recommends that saturated fats (of which butter is a generous source) make up no more than 10% of our calorie intake:
Source: Saturated fatty acid and trans-fatty acid intake for adults and children: WHO guideline
So if you have a 2000 kcal daily intake, that would mean consuming not more than 200 kcal from butter, which is approximately two tablespoons.
If you’d like a deeper look into the complexities of saturated fats (for and against), you might like our previous main feature specifically about such:
Can Saturated Fats Be Healthy?
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: