What is mitochondrial donation? And how might it help people have a healthy baby one day?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Mitochondria are tiny structures in cells that convert the food we eat into the energy our cells need to function.
Mitochondrial disease (or mito for short) is a group of conditions that affect this ability to generate the energy organs require to work properly. There are many different forms of mito and depending on the form, it can disrupt one or more organs and can cause organ failure.
There is no cure for mito. But an IVF procedure called mitochondrial donation now offers hope to families affected by some forms of mito that they can have genetically related children free from mito.
After a law to allow mitochondrial donation in Australia was passed in 2022, scientists are now preparing for a clinical trial to see if mitochondrial donation is safe and works.

What is mitochondrial disease?
There are two types of mitochondrial disease.
One is caused by faulty genes in the nuclear DNA, the DNA we inherit from both our parents and which makes us who we are.
The other is caused by faulty genes in the mitochondria’s own DNA. Mito caused by faulty mitochondrial DNA is passed down through the mother. But the risk of disease is unpredictable, so a mother who is only mildly affected can have a child who develops serious disease symptoms.
Mitochondrial disease is the most common inherited metabolic condition affecting one in 5,000 people.
Some people have mild symptoms that progress slowly, while others have severe symptoms that progress rapidly. Mito can affect any organ, but organs that need a lot of energy such as brain, muscle and heart are more often affected than other organs.
Mito that manifests in childhood often involves multiple organs, progresses rapidly, and has poor outcomes. Of all babies born each year in Australia, around 60 will develop life-threatening mitochondrial disease.
What is mitochondrial donation?
Mitochondrial donation is an experimental IVF-based technique that offers people who carry faulty mitochondrial DNA the potential to have genetically related children without passing on the faulty DNA.
It involves removing the nuclear DNA from the egg of someone who carries faulty mitochondrial DNA and inserting it into a healthy egg donated by someone not affected by mito, which has had its nuclear DNA removed.
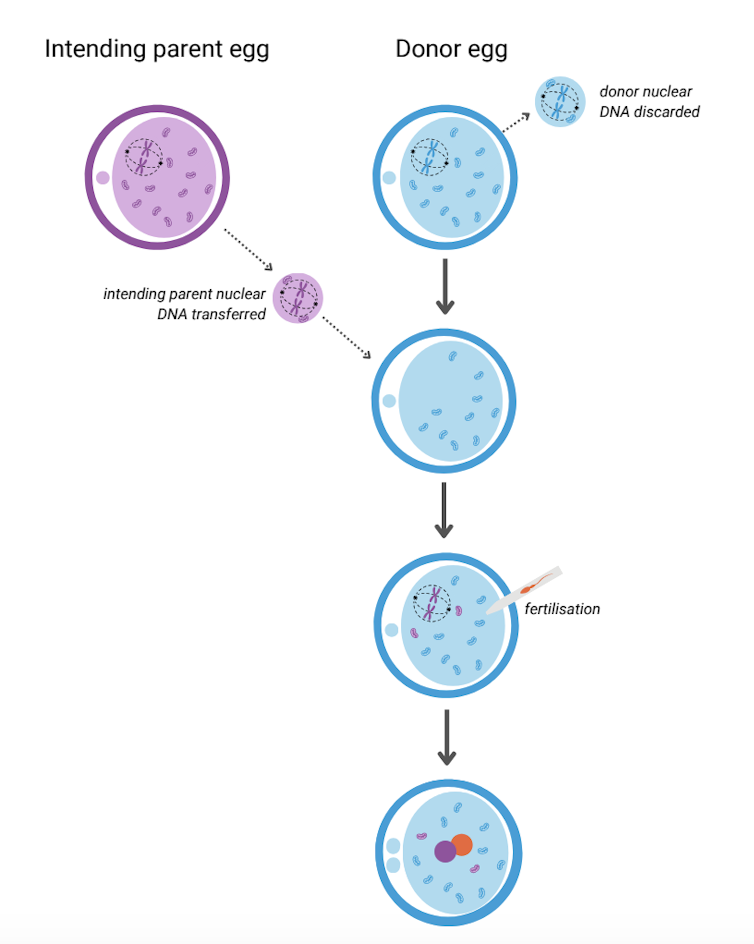
The resulting egg has the nuclear DNA of the intending parent and functioning mitochondria from the donor. Sperm is then added and this allows the transmission of both intending parents’ nuclear DNA to the child.
A child born after mitochondrial donation will have genetic material from the three parties involved: nuclear DNA from the intending parents and mitochondrial DNA from the egg donor. As a result the child will likely have a reduced risk of mito, or no risk at all.

This highly technical procedure requires specially trained scientists and sophisticated equipment. It also requires both the person with mito and the egg donor to have hormone injections to stimulate the ovaries to produce multiple eggs. The eggs are then retrieved in an ultrasound-guided surgical procedure.
Mitochondrial donation has been pioneered in the United Kingdom where a handful of babies have been born as a result. To date there have been no reports about whether they are free of mito.
Maeve’s Law
After three years of public consultation The Mitochondrial Donation Law Reform (Maeve’s Law) Bill 2021 was passed in the Australian Senate in 2022, making mitochondrial donation legal in a research and clinical trial setting.
Maeve’s law stipulates strict conditions including that clinics need a special licence to perform mitochondrial donation.
To make sure mitochondrial donation works and is safe before it’s introduced into Australian clinical practice, the law also specifies that initial licences will be issued for pre-clinical and clinical trial research and training.
We’re expecting one such licence to be issued for the mitoHOPE (Healthy Outcomes Pilot and Evaluation) program, which we are part of, to perfect the technique and conduct a clinical trial to make sure mitochondrial donation is safe and effective.
Before starting the trial, a preclinical research and training program will ensure embryologists are trained in “real-life” clinical conditions and existing mitochondrial donation techniques are refined and improved. To do this, many human eggs are needed.
The need for donor eggs
One of the challenges with mitochondrial donation is sourcing eggs. For the preclinical research and training program, frozen eggs can be used, but for the clinical trial “fresh” eggs will be needed.
One possible source of frozen eggs is from people who have stored eggs they don’t intend to use.
A recent study looked at data on the outcomes of eggs stored at a Melbourne clinic from 2012 to 2021. Over the ten-year period, 1,132 eggs from 128 patients were discarded. No eggs were donated to research because the clinics where the eggs were stored did not conduct research requiring donor eggs.
However, research shows that among people with stored eggs, the number one choice for what to do with eggs they don’t need is to donate them to research.
This offers hope that, given the opportunity, those who have eggs stored that they don’t intend to use might be willing to donate them to mitochondrial donation preclinical research.
As for the “fresh” eggs needed in the future clinical trial, this will require individuals to volunteer to have their ovaries stimulated and eggs retrieved to give those people impacted by mito a chance to have a healthy baby. Egg donors may be people who are friends or relatives of those who enter the trial, or it might be people who don’t know someone affected by mito but would like to help them conceive.
At this stage, the aim is to begin enrolling participants in the clinical trial in the next 12 to 18 months. However this may change depending on when the required licences and ethics approvals are granted.
Karin Hammarberg, Senior Research Fellow, Global and Women’s Health, School of Public Health & Preventive Medicine, Monash University; Catherine Mills, Professor of Bioethics, Monash University; Mary Herbert, Professor, Anatomy & Developmental Biology, Monash University, and Molly Johnston, Research fellow, Monash Bioethics Centre, Monash University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Is “Extra Virgin” Worth It?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝I was wondering, is the health difference important between extra virgin olive oil and regular?❞
Assuming that by “regular” you mean “virgin and still sold as a food product”, then there are health differences, but they’re not huge. Or at least: not nearly so big as the differences between those and other oils.
Virgin olive oil (sometimes simply sold as “olive oil”, with no claims of virginity) has been extracted by the same means as extra virgin olive oil, that is to say: purely mechanical.
The difference is that extra virgin olive oil comes from the first pressing*, so the free fatty acid content is slightly lower (later checked and validated and having to score under a 0.8% limit for “extra virgin” instead of 2% limit for a mere “virgin”).
*Fun fact: in Arabic, extra virgin is called “البكر الممتاز“, literally “the amazing first-born”, because of this feature!
It’s also slightly higher in mono-unsaturated fatty acids, which is a commensurately slight health improvement.
It’s very slightly lower in saturated fats, which is an especially slight health improvement, as the saturated fats in olive oil are amongst the healthiest saturated fats one can consume.
On which fats are which:
The truth about fats: the good, the bad, and the in-between
And our own previous discussion of saturated fats in particular:
Can Saturated Fats Be Healthy?
Probably the strongest extra health-benefit of extra virgin is that while that first pressing squeezes out oil with the lowest free fatty acid content, it squeezes out oil with the highest polyphenol content, along with other phytonutrients:
If you enjoy olive oil, then springing for extra virgin is worth it if that’s not financially onerous, both for health reasons and taste.
However, if mere “virgin” is what’s available, it’s no big deal to have that instead; it still has a very similar nutritional profile, and most of the same benefits.
Don’t settle for less than “virgin”, though.
While some virgin olive oils aren’t marked as such, if it says “refined” or “blended”, then skip it. These will have been extracted by chemical means and/or blended with completely different oils (e.g. canola, which has a very different nutritional profile), and sometimes with a dash of virgin or extra virgin, for the taste and/or so that they can claim in big writing on the label something like:
a blend of
EXTRA VIRGIN OLIVE OIL
and other oils…despite having only a tiny amount of extra virgin olive oil in it.
Different places have different regulations about what labels can claim.
The main countries that produce olives (and the EU, which contains and/or directly trades with those) have this set of rules:
International Olive Council: Designations and definitions of Olive Oils
…which must be abided by or marketers face heavy fines and sanctions.
In the US, the USDA has its own set of rules based on the above:
USDA | Olive Oil and Olive-Pomace Oil Grades and Standards
…which are voluntary (not protected by law), and marketers can pay to have their goods certified if they want.
So if you’re in the US, look for the USDA certification or it really could be:
- What the USDA calls “US virgin olive oil not fit for human consumption”, which in the IOC is called “lamp oil”*
- crude pomace-oil (oil made from the last bit of olive paste and then chemically treated)
- canola oil with a dash of olive oil
- anything yellow and oily, really
*This technically is virgin olive oil insofar as it was mechanically extracted, but with defects that prevent it from being sold as such, such as having a free fatty acid content above the cut-off, or just a bad taste/smell, or some sort of contamination.
See also: Potential Health Benefits of Olive Oil and Plant Polyphenols
(the above paper has a handy infographic if you scroll down just a little)
Where can I get some?
Your local supermarket, probably, but if you’d like to get some online, here’s an example product on Amazon for your convenience
Enjoy!
Share This Post
-
Exercises for Aging-Ankles
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Can Ankles Deterioration be Stopped?
As we all know (or have experienced!), Ankle mobility deteriorates with age.
We’re here to argue that it’s not all doom and gloom!
(In fact, we’ve written about keeping our feet, and associated body parts, healthy here).
This video by “Livinleggings” (below) provides a great argument that yes, ankle deterioration can be stopped, or even reversed. It’s a must-watch for anyone from yoga enthusiasts to gym warriors who might be unknowingly crippling their ankle-health.
How We Can Prioritise Our Ankles
Poor ankle flexibility isn’t just an inconvenience – it’s a direct route to knee issues, hip hiccups, and back pain. More importantly, ankle strength is a core component of building overall mobility.
With 12 muscles in the ankle, it can be overwhelming to work out which to strengthen – and how. But fear not, we can prioritise three of the twelve: the calf duo (gastrocnemius and soleus) and the shin’s main muscle, the tibialis anterior.
The first step is to test yourself! A simple wall test reveals any hidden truths about your ankle flexibility. Go to the 1:55 point in the video to see how it’s done.
If you can’t do it, you’ve got work to be done.
If you read the book we recommended on great functional exercises for seniors, then you may already be familiar with some super ankle exercises.
Otherwise, these four ankle exercises are a great starting point:
How did you find that video? If you’ve discovered any great videos yourself that you’d like to share with fellow 10almonds readers, then please do email them to us!
Share This Post
-
If you’re worried about inflammation, stop stressing about seed oils and focus on the basics
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
You’ve probably seen recent claims online seed oils are “toxic” and cause inflammation, cancer, diabetes and heart disease. But what does the research say?
Overall, if you’re worried about inflammation, cancer, diabetes and heart disease there are probably more important things to worry about than seed oils.
They may or may not play a role in inflammation (the research picture is mixed). What we do know, however, is that a high-quality diet rich in unprocessed whole foods (fruits, vegetables, nuts, seeds, grains and lean meats) is the number one thing you can to do reduce inflammation and your risk of developing diseases.
Rather than focusing on seed oils specifically, reduce your intake of processed foods more broadly and focus on eating fresh foods. So don’t stress out too much about using a bit of seed oils in your cooking if you are generally focused on all the right things.
What are seed oils?
Seed oils are made from whole seeds, such as sunflower seeds, flax seeds, chia seeds and sesame seeds. These seeds are processed to extract oil.
The most common seed oils found at grocery stores include sesame oil, canola oil, sunflower oil, flaxseed oil, corn oil, grapeseed oil and soybean oil.
Seed oils are generally affordable, easy to find and suitable for many dishes and cuisines as they often have a high smoke point.
However, most people consume seed oils in larger amounts through processed foods such as biscuits, cakes, chips, muesli bars, muffins, dipping sauces, deep-fried foods, salad dressings and margarines.
These processed foods are “discretionary”, meaning they’re OK to have occasionally. But they are not considered necessary for a healthy diet, nor recommended in our national dietary guidelines, the Australian Guide for Healthy Eating.
Seed oils often have a high smoke point.
Gleb Usovich/ShutterstockI’ve heard people say seed oils ‘promote inflammation’. Is that true?
There are two essential types of omega fatty acids: omega-3 and omega-6. These are crucial for bodily functions, and we must get them through our diet since our bodies cannot produce them.
While all oils contain varying levels of fatty acids, some argue an excessive intake of a specific omega-6 fatty acid in seed oils called “linoleic acid” may contribute to inflammation in the body.
There is some evidence linoleic acid can be converted to arachidonic acid in the body and this may play a role in inflammation. However, other research doesn’t support the idea reducing dietary linoleic acid affects the amount of arachidonic acid in your body. The research picture is not clear cut.
But if you’re keen to reduce inflammation, the best thing you can do is aim for a healthy diet that is:
- high in antioxidants (found in fruits and vegetables)
- high in “healthy”, unsaturated fatty acids (found in fatty fish, some nuts and olive oil, for example)
high in fibre (found in carrots, cauliflower, broccoli and leafy greens) and prebiotics (found in onions, leeks, asparagus, garlic and legumes)
low in processed foods.
If reducing inflammation is your goal, it’s probably more meaningful to focus on these basics than on occasional use of seed oils.
Choose foods high in fibre (like many vegetables) and prebiotics (like legumes).
Kiian Oksana/ShutterstockWhat about seed oils and heart disease, cancer or diabetes risk?
Some popular arguments against seed oils come from data from single studies on this topic. Often these are observational studies where researchers do not make changes to people’s diet or lifestyle.
To get a clearer picture, we should look at meta-analyses, where scientists combine all the data available on a topic. This helps us get a better overall view of what’s going on.
A 2022 meta-analysis of randomised controlled trials investigated the relationship between supplementation with omega-6 fatty acid (often found in seed oils) and cardiovascular disease risk (meaning disease relating to the heart and blood vessels).
The researchers found omega-6 intake did not affect the risk for cardiovascular disease or death but that further research is needed for firm conclusions. Similar findings were observed in a 2019 review on this topic.
The World Health Organization published a review and meta-analysis in 2022 of observational studies (considered lower quality evidence compared to randomised controlled trials) on this topic.
They looked at omega-6 intake and risk of death, cardiovascular disease, breast cancer, mental health conditions and type 2 diabetes. The findings show both advantages and disadvantages of consuming omega-6.
The findings reported that, overall, higher intakes of omega-6 were associated with a 9% reduced risk of dying (data from nine studies) but a 31% increased risk of postmenopausal breast cancer (data from six studies).
One of the key findings from this review was about the ratio of omega-3 fatty acids to omega-6 fatty acids. A higher omega 6:3 ratio was associated with a greater risk of cognitive decline and ulcerative colitis (an inflammatory bowel condition).
A higher omega 3:6 ratio was linked to a 26% reduced risk of depression. These mixed outcomes may be a cause of confusion among health-conscious consumers about the health impact of seed oils.
Overall, the evidence suggests that a high intake of omega-6 fatty acids from seed oils is unlikely to increase your risk of death and disease.
However, more high-quality intervention research is needed.
The importance of increasing your omega-3 fatty acids
On top of the mixed outcomes, there is clear evidence increasing the intake of omega-3 fatty acids (often found in foods such as fatty fish and walnuts) is beneficial for health.
While some seed oils contain small amounts of omega-3s, they are not typically considered rich sources.
Flaxseed oil is an exception and is one of the few seed oils that is notably high in alpha-linolenic acid (sometimes shortened to ALA), an omega-3 fatty acid.
If you are looking to increase your omega-3 intake, it’s better to focus on other sources such as fatty fish (salmon, mackerel, sardines), chia seeds, hemp seeds, walnuts, and algae-based supplements. These foods are known for their higher omega-3 content compared to seed oils.
The bottom line
At the end of the day, it’s probably OK to include small quantities of seed oils in your diet, as long as you are mostly focused on eating fresh, unprocessed foods.
The best way to reduce your risk of inflammation, heart disease, cancer or diabetes is not to focus so much on seed oils but rather on doing your best to follow the Australian Guide for Healthy Eating.
Lauren Ball, Professor of Community Health and Wellbeing, The University of Queensland and Emily Burch, Lecturer, Southern Cross University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
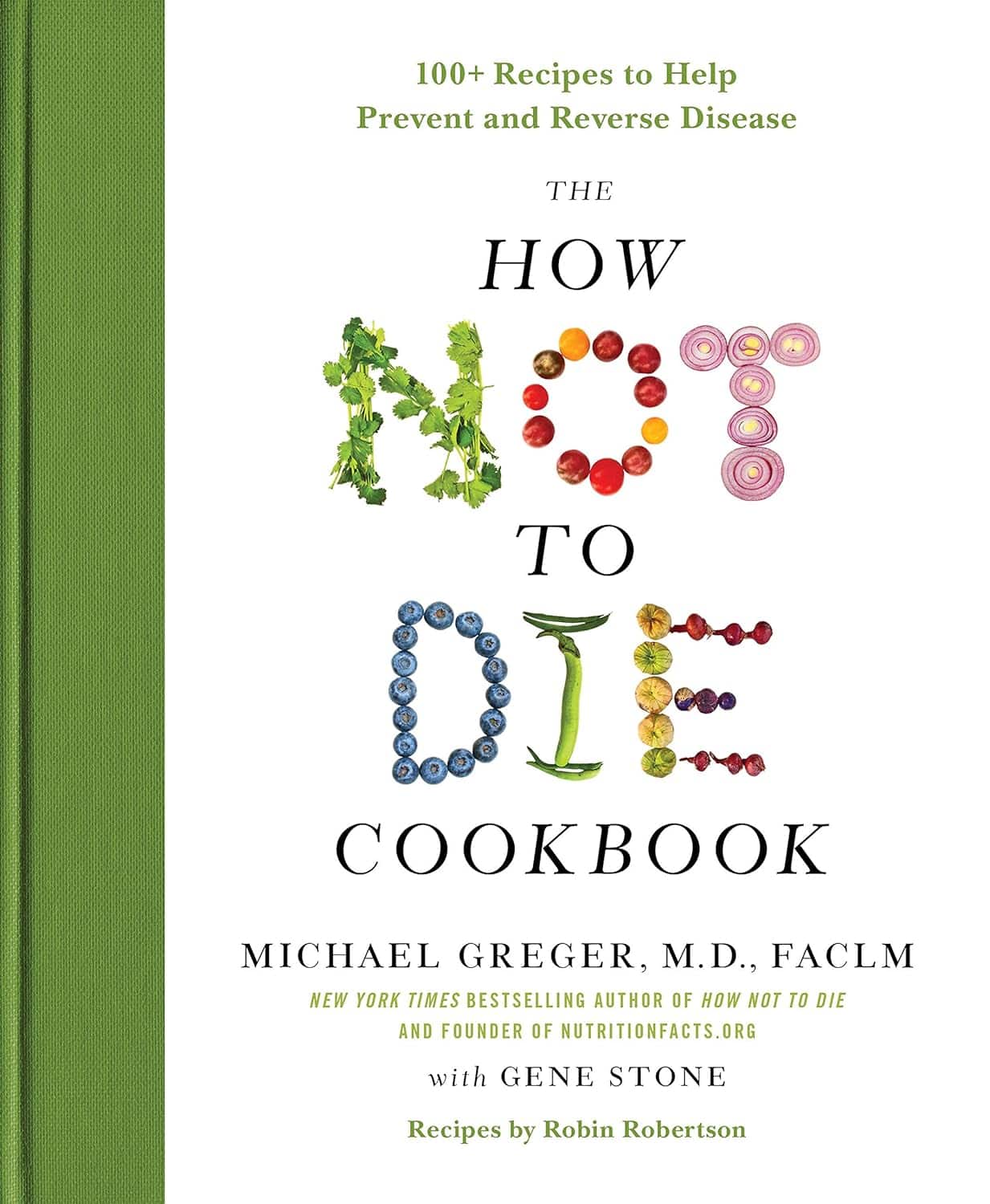
The How Not to Die Cookbook – by Dr. Michael Greger
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve previously reviewed Dr. Greger’s “How Not To Die”, which is excellent and/but very science-dense.
This book is different, in that the science is referenced and explained throughout, but the focus is the recipes, and how to prepare delicious healthy food in accordance with the principles laid out in How Not To Die.
It also follows “Dr Greger’s Daily Dozen“, that is to say, the 12 specific things he advises we make sure to have every day, and thus helps us to include them in an easy, no-fuss fashion.
The recipes themselves are by Robin Robertson, and/but with plenty of notes by Dr Greger; they clearly collaborated closely in creating them.
The ingredients are all things one can find in any well-stocked supermarket, so unless you live in a food desert, you can make these things easily.
And yes, the foods are delicious too.
Bottom line: if you’re interested in cooking according to perhaps the most science-based dietary system out there, then this book is a top-tier choice.
Click here to check out The How Not To Die Cookbook, and live well!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Alpha, beta, theta: what are brain states and brain waves? And can we control them?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
There’s no shortage of apps and technology that claim to shift the brain into a “theta” state – said to help with relaxation, inward focus and sleep.
But what exactly does it mean to change one’s “mental state”? And is that even possible? For now, the evidence remains murky. But our understanding of the brain is growing exponentially as our methods of investigation improve.
Brain-measuring tech is evolving
Currently, no single approach to imaging or measuring brain activity gives us the whole picture. What we “see” in the brain depends on which tool we use to “look”. There are myriad ways to do this, but each one comes with trade-offs.
We learnt a lot about brain activity in the 1980s thanks to the advent of magnetic resonance imaging (MRI).
Eventually we invented “functional MRI”, which allows us to link brain activity with certain functions or behaviours in real time by measuring the brain’s use of oxygenated blood during a task.
We can also measure electrical activity using EEG (electroencephalography). This can accurately measure the timing of brain waves as they occur, but isn’t very accurate at identifying which specific areas of the brain they occur in.
Alternatively, we can measure the brain’s response to magnetic stimulation. This is very accurate in terms of area and timing, but only as long as it’s close to the surface.
What are brain states?
All of our simple and complex behaviours, as well as our cognition (thoughts) have a foundation in brain activity, or “neural activity”. Neurons – the brain’s nerve cells – communicate by a sequence of electrical impulses and chemical signals called “neurotransmitters”.
Neurons are very greedy for fuel from the blood and require a lot of support from companion cells. Hence, a lot of measurement of the site, amount and timing of brain activity is done via measuring electrical activity, neurotransmitter levels or blood flow.
We can consider this activity at three levels. The first is a single-cell level, wherein individual neurons communicate. But measurement at this level is difficult (laboratory-based) and provides a limited picture.
As such, we rely more on measurements done on a network level, where a series of neurons or networks are activated. Or, we measure whole-of-brain activity patterns which can incorporate one or more so-called “brain states”.
According to a recent definition, brain states are “recurring activity patterns distributed across the brain that emerge from physiological or cognitive processes”. These states are functionally relevant, which means they are related to behaviour.
Brain states involve the synchronisation of different brain regions, something that’s been most readily observed in animal models, usually rodents. Only now are we starting to see some evidence in human studies.
Various kinds of states
The most commonly-studied brain states in both rodents and humans are states of “arousal” and “resting”. You can picture these as various levels of alertness.
Studies show environmental factors and activity influence our brain states. Activities or environments with high cognitive demands drive “attentional” brain states (so-called task-induced brain states) with increased connectivity. Examples of task-induced brain states include complex behaviours such as reward anticipation, mood, hunger and so on.
In contrast, a brain state such as “mind-wandering” seems to be divorced from one’s environment and tasks. Dropping into daydreaming is, by definition, without connection to the real world.
We can’t currently disentangle multiple “states” that exist in the brain at any given time and place. As mentioned earlier, this is because of the trade-offs that come with recording spatial (brain region) versus temporal (timing) brain activity.
Brain states vs brain waves
Brain state work can be couched in terms such as alpha, delta and so forth. However, this is actually referring to brain waves which specifically come from measuring brain activity using EEG.
EEG picks up on changing electrical activity in the brain, which can be sorted into different frequencies (based on wavelength). Classically, these frequencies have had specific associations:
- gamma is linked with states or tasks that require more focused concentration
- beta is linked with higher anxiety and more active states, with attention often directed externally
- alpha is linked with being very relaxed, and passive attention (such as listening quietly but not engaging)
- theta is linked with deep relaxation and inward focus
- and delta is linked with deep sleep.
Brain wave patterns are used a lot to monitor sleep stages. When we fall asleep we go from drowsy, light attention that’s easily roused (alpha), to being relaxed and no longer alert (theta), to being deeply asleep (delta).
Can we control our brain states?
The question on many people’s minds is: can we judiciously and intentionally influence our brain states?
For now, it’s likely too simplistic to suggest we can do this, as the actual mechanisms that influence brain states remain hard to detangle. Nonetheless, researchers are investigating everything from the use of drugs, to environmental cues, to practising mindfulness, meditation and sensory manipulation.
Controversially, brain wave patterns are used in something called “neurofeedback” therapy. In these treatments, people are given feedback (such as visual or auditory) based on their brain wave activity and are then tasked with trying to maintain or change it. To stay in a required state they may be encouraged to control their thoughts, relax, or breathe in certain ways.
The applications of this work are predominantly around mental health, including for individuals who have experienced trauma, or who have difficulty self-regulating – which may manifest as poor attention or emotional turbulence.
However, although these techniques have intuitive appeal, they don’t account for the issue of multiple brain states being present at any given time. Overall, clinical studies have been largely inconclusive, and proponents of neurofeedback therapy remain frustrated by a lack of orthodox support.
Other forms of neurofeedback are delivered by MRI-generated data. Participants engaging in mental tasks are given signals based on their neural activity, which they use to try and “up-regulate” (activate) regions of the brain involved in positive emotions. This could, for instance, be useful for helping people with depression.
Another potential method claimed to purportedly change brain states involves different sensory inputs. Binaural beats are perhaps the most popular example, wherein two different wavelengths of sound are played in each ear. But the evidence for such techniques is similarly mixed.
Treatments such as neurofeedback therapy are often very costly, and their success likely relies as much on the therapeutic relationship than the actual therapy.
On the bright side, there’s no evidence these treatment do any harm – other than potentially delaying treatments which have been proven to be beneficial.
Susan Hillier, Professor: Neuroscience and Rehabilitation, University of South Australia
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Lost Art of Silence – by Sarah Anderson
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
From “A Room Of One’s Own” to “Silent Mondays”, from spiritual retreats to noise-cancelling headphones, this book covers the many benefits of silence—and a couple of downsides too.
In an age where most things are available at the touch of a button, a little peaceful solitude can come at quite a premium, but what it offers can effect all manner of physical changes, from reduced stress responses to increased neurogenesis (growing new brain cells).
The tone throughout is a combination of personal and pop-science, and it’s very motivating to find a little more space-between-the-things in life.
The book is best enjoyed in a quiet room.
Bottom line: if you get the feeling sometimes that you could rest and recover fully and properly if you could just find the downtime, this book will help you find exactly that.
Click here to check out the Lost Art of Silence, and find peace and strength in it!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: