Burned Out By Tuesday?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Avoiding Burnout, The Active Way
This is Dr. Claudine Holt. She’s double board-certified, in Occupational & Environmental Medicine, and Lifestyle Medicine.
In short: preventative medicine in all parts of our life.
Hopefully, you are reading this bright-eyed and bushy-tailed and ready to take on another exciting day in this wonderful, beautiful world!
On the other hand, it’s possible that you’re reading this semi-focussed, looking for a crumb of dopamine as much as you are looking for information.
If you’ve ever had the “What a week!” / “It’s only Tuesday” moment, this one’s for you.
What does Dr. Holt want us to know?
You can recover from burnout without guilt
Sometimes, we overreach ourselves. Sometimes, life overreaches us! Sometimes it’s not that we overcommitted—it’s just that we were taking each day as it comes, but sometimes several days gang up on us at once.
Sometimes, even, we can feel exhausted when it seems like we haven’t done anything.
Note: if you feel exhausted and it seems like you haven’t done anything, then be aware: you are exhausted for a reason!
What that reason might be may vary, but contrary to popular belief, energy does not just vanish. It went somewhere.
This goes double if you have any chronic illness(es), even if you’re not aware of having had a flare-up, chances are you were just exceptionally busy (on a cellular level).
And it’s easy to think that “mere” cellular activity shouldn’t be exhausting, but that is 100% of where our energy transactions happen—whether or not we are consciously aware of them!
See also: Eat To Beat Chronic Fatigue ← yes, this also covers when you are too exhausted to shop and cook like a TV chef
Dr. Holt specializes in working with burned out medical professionals (and also specifically specializes in working with women), but there are lessons for everyone in her advice. For example:
Fiction: ”Medicine is my calling–it’s who I am.”
Fact: You are more than medicine! Remember that your career is just one aspect of your life. Don’t forget to create your big-picture vision and tend the garden of the other areas of your life too.
Read more: Dr. Claudine Holt | Burnout: Fact vs Fiction
This same thing can go for whatever part of your identity frequently follows “I’m a…”, and is somewhere that you put a lot of your energy; it could equally be a non-professional job like “homemaker”, or a relational status like “husband”, or a cultural identifier like “Christian”, or a hobby like “gardener” (assuming that is not also your profession, in which case, same item, different category).
Indeed, a lot of women especially get hit by “the triple burden” of professional work, housework, and childcare. And it’s not even necessarily that we resent any of those things or feel like they’re a burden; we (hopefully) love our professions, homes, children. But, here’s the thing:
No amount of love will add extra hours to the day.
So what does she recommend doing about it, when sometimes we’re juggling things that can’t be dropped?
Start simple, but start!
Dr. Holt recommends to start with a smile (yes even if, and sometimes especially when, the circumstances do not feel like they merit it), and deploy some CBT tools:
Two Hacks to Quickly Rise Above Burnout (Or Any Circumstance)
We’ve expanded on this topic here:
With a more level head on, it becomes easier to take on the next step, which creating healthy boundaries—and that doesn’t just mean with other people!
It also means slaying our own perfectionism and imposter syndrome—both things that will have us chasing our tails 36 hours per day if we let them.
See also:
- Perfectionism, And How To Make Yours Work For You
- Imposter Syndrome (And Why Almost Everyone Has It)
❝Burnout is the culture of our times. A culture that expects us to do more and think our way out of everything. A culture that asks for more than the body can bear. Unfortunately, even though the situation might not be of our creation, burnout culture is our inheritance.
An inheritance we can either perpetuate—or change—depending on what we embody.❞
Source: The Embodied MD on Burnout with Dr Claudine Holt
That “embodiment” is partly our choices and actions that we bring and own just as we bring and own our body—and it’s partly our relationship with our body itself, and learning to love it, and work with it to achieve wonderful things, instead of just getting through the day.
Which yes, does also mean making space for good diet, exercise, sleep and so forth, per:
These Top Five Things Make The Biggest Difference To Health
Want to know more?
You might like to check out Dr. Holt’s website:
The Embodied M.D. | Burnout Coach
…where she also offers resources such as a blog and a podcast.
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
We analysed almost 1,000 social media posts about 5 popular medical tests. Most were utterly misleading
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When Kim Kardashian posted on Instagram about having had a full-body MRI, she enthused that the test can be “life saving”, detecting diseases in the earliest stages before symptoms arise.
What Kardashian neglected to say was there’s no evidence this expensive scan can bring benefits for healthy people. She also didn’t mention it can carry harms including unnecessary diagnoses and inappropriate treatments.
With this post in mind, we wanted to explore what influencers are telling us about medical tests.
In a new study published today in JAMA Network Open, we analysed nearly 1,000 Instagram and TikTok posts about five popular medical tests which can all do more harm than good to healthy people, including the full-body MRI scan.
We found the overwhelming majority of these posts were utterly misleading.
C-R-V/Shutterstock 5 controversial tests
Before we get into the details of what we found, a bit about the five tests included in our study.
While these tests can be valuable to some, all five carry the risk of overdiagnosis for generally healthy people. Overdiagnosis is the diagnosis of a condition which would have never caused symptoms or problems. Overdiagnosis leads to overtreatment, which can cause unnecessary side effects and stress for the person, and wasted resources for the health system.
As an example, estimates suggest 29,000 cancers a year are overdiagnosed in Australia alone.
Overdiagnosis is a global problem, and it’s driven in part by healthy people having tests like these. Often, they’re promoted under the guise of early screening, as a way to “take control” of your health. But most healthy people simply don’t need them.
These are the five tests we looked at:
The full-body MRI scan claims to test for up to 500 conditions, including cancer. Yet there is no proven benefit of the scan for healthy people, and a real risk of unnecessary treatment from “false alarm” diagnoses.
The “egg timer” test (technically known as the AMH, or anti-mullarian hormone test) is often falsely promoted as a fertility test for healthy women. While it may be beneficial for women within a fertility clinic setting, it cannot reliably predict the chance of a woman conceiving, or menopause starting. However, low results can increase fear and anxiety, and lead to unnecessary and expensive fertility treatments.
Multi-cancer early detection blood tests are being heavily marketed as the “holy grail of cancer detection”, with claims they can screen for more than 50 cancers. In reality, clinical trials are still a long way from finished. There’s no good evidence yet that the benefits will outweigh the harms of unnecessary cancer diagnoses.
The gut microbiome test of your stool promises “wellness” via early detection of many conditions, from flatulence to depression, again without good evidence of benefit. There’s also concern that test results can lead to wasted resources.
Testosterone testing in healthy men is not supported by any high-quality evidence, with concerns direct-to-consumer advertising leads men to get tested and take testosterone replacement therapy unnecessarily. Use of testosterone replacement therapy carries its own risk of potential harms with the long-term safety in relation to heart disease and mortality still largely unknown.
Multi-cancer early detection blood tests are heavily marketed. Yuri A/Shutterstock What we found
Together with an international group of health researchers, we analysed 982 posts pertaining to the above tests from across Instagram and TikTok. The posts we looked at came from influencers and account holders with at least 1,000 followers, some with a few million followers. In total, the creators of the posts we included had close to 200 million followers.
Even discounting the bots, that’s a massive amount of influence (and likely doesn’t reflect their actual reach to non-followers too).
The vast majority of posts were misleading, failing to even mention the possibility of harm arising from taking one of these tests. We found:
- 87% of posts mentioned test benefits, while only 15% mentioned potential harms
- only 6% of posts mentioned the risk of overdiagnosis
- only 6% of posts discussed any scientific evidence, while 34% of posts used personal stories to promote the test
- 68% of influencers and account holders had financial interests in promoting the test (for example, a partnership, collaboration, sponsorship or selling for their own profit in some way).
Further analysis revealed medical doctors were slightly more balanced in their posts. They were more likely to mention the harms of the test, and less likely to have a strongly promotional tone.
The vast majority of posts we looked at were misleading. DimaBerlin/Shutterstock As all studies do, ours had some limitations. For example, we didn’t analyse comments connected to posts. These may give further insights into the information being provided about these tests, and how social media users perceive them.
Nonetheless, our findings add to the growing body of evidence showing misleading medical information is widespread on social media.
What can we do about it?
Experts have proposed a range of solutions including pre-bunking strategies, which means proactively educating the public about common misinformation techniques.
However, solutions like these often place responsibility on the individual. And with all the information on social media to navigate, that’s a big ask, even for people with adequate health literacy.
What’s urgently needed is stronger regulation to prevent misleading information being created and shared in the first place. This is especially important given social media platforms including Instagram are moving away from fact-checking.
In the meantime, remember that if information about medical tests promoted by influencers sounds too good to be true, it probably is.
Brooke Nickel, NHMRC Emerging Leader Research Fellow, University of Sydney; Joshua Zadro, NHMRC Emerging Leader Research Fellow, Sydney Musculoskeletal Health, University of Sydney, and Ray Moynihan, Assistant Professor, Faculty of Health Sciences & Medicine, Bond University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Food Expiration Dates Don’t Mean What Most People Think They Mean
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Have you ever wondered why rock salt that formed during the Precambrian era has a label on it saying that it expires next month? To take something more delicate, how about eggs that expire next Thursday; isn’t that oddly specific for something that is surely affected by many variables? What matters, and what doesn’t?
Covering their assets
The US in particular wastes huge amounts of food, with 37% of food waste coming from households. Confusion over date labels is a major contributor, accounting for 20% of household food waste. Many people misinterpret these labels, often discarding food that is still safe to eat—which is good for the companies selling the food, because then they get to sell you more.
Date labels were introduced in the 70s with the “open dating” system to indicate optimal freshness, not safety. These dates are often conservative, set by manufacturers to ensure food is consumed at its best quality and encourage repeat purchases. However, many foods remain safe well past their labeled dates, including shelf-stable items like pasta, rice, and canned goods, as well as frozen foods stored properly.
Some foods do pose safety risks, especially meat and dairy products, as well as many grain-based foods, all of which which can harbor harmful bacteria. Infant formula labels are strictly regulated for safety. However, most date labels are not linked to health risks, leading to unnecessary waste.
When it comes down to it, our senses of sight, smell, and taste are more reliable than dates on packaging. Some quick pointers and caveats:
- If it has changed color in some way that’s not associated with a healthily ripening fruit or vegetable, that’s probably bad
- If it is moldy, that’s probably bad (but the degree of badness varies from food to food; see the link beneath today’s video for more on that)
- If a container has developed droplets of water on the inside when it didn’t have those before, that’s probably bad (it means something is respiring, and is thus alive, that probably shouldn’t be)
- If it smells bad, that’s probably bad—however this is not a good safety test, because a bad smell may often mean you are inhaling mold spores, which are not good for your lungs.
- If it tastes different than that food usually does, that’s probably bad (especially if it became bitter, pungent, tangy, sour, or cheesy, and does nor normally taste that way).
Some places have trialled clearer labelling, for example a distinction between “expires” and merely “best before”, but public awareness about the distinction is low. Some places have trialled removing dates entirely, to oblige the consumer to use their own senses instead. This is good for the seller in a different way than household food waste is, because it means the seller will have less in-store waste (because they can still sell something that might previously have been labelled as expired).
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Take care!
Share This Post
-
What pathogen might spark the next pandemic? How scientists are preparing for ‘disease X’
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Before the COVID pandemic, the World Health Organization (WHO) had made a list of priority infectious diseases. These were felt to pose a threat to international public health, but where research was still needed to improve their surveillance and diagnosis. In 2018, “disease X” was included, which signified that a pathogen previously not on our radar could cause a pandemic.
While it’s one thing to acknowledge the limits to our knowledge of the microbial soup we live in, more recent attention has focused on how we might systematically approach future pandemic risks.
Former US Secretary of Defense Donald Rumsfeld famously talked about “known knowns” (things we know we know), “known unknowns” (things we know we don’t know), and “unknown unknowns” (the things we don’t know we don’t know).
Although this may have been controversial in its original context of weapons of mass destruction, it provides a way to think about how we might approach future pandemic threats.
Anna Shvets/Pexels Influenza: a ‘known known’
Influenza is largely a known entity; we essentially have a minor pandemic every winter with small changes in the virus each year. But more major changes can also occur, resulting in spread through populations with little pre-existing immunity. We saw this most recently in 2009 with the swine flu pandemic.
However, there’s a lot we don’t understand about what drives influenza mutations, how these interact with population-level immunity, and how best to make predictions about transmission, severity and impact each year.
The current H5N1 subtype of avian influenza (“bird flu”) has spread widely around the world. It has led to the deaths of many millions of birds and spread to several mammalian species including cows in the United States and marine mammals in South America.
Human cases have been reported in people who have had close contact with infected animals, but fortunately there’s currently no sustained spread between people.
While detecting influenza in animals is a huge task in a large country such as Australia, there are systems in place to detect and respond to bird flu in wildlife and production animals.
Scientists are continually monitoring a range of pathogens with pandemic potential. Edward Jenner/Pexels It’s inevitable there will be more influenza pandemics in the future. But it isn’t always the one we are worried about.
Attention had been focused on avian influenza since 1997, when an outbreak in birds in Hong Kong caused severe disease in humans. But the subsequent pandemic in 2009 originated in pigs in central Mexico.
Coronaviruses: an ‘unknown known’
Although Rumsfeld didn’t talk about “unknown knowns”, coronaviruses would be appropriate for this category. We knew more about coronaviruses than most people might have thought before the COVID pandemic.
We’d had experience with severe acute respiratory syndrome (SARS) and Middle Eastern respiratory syndrome (MERS) causing large outbreaks. Both are caused by viruses closely related to SARS-CoV-2, the coronavirus that causes COVID. While these might have faded from public consciousness before COVID, coronaviruses were listed in the 2015 WHO list of diseases with pandemic potential.
Previous research into the earlier coronaviruses proved vital in allowing COVID vaccines to be developed rapidly. For example, the Oxford group’s initial work on a MERS vaccine was key to the development of AstraZeneca’s COVID vaccine.
Similarly, previous research into the structure of the spike protein – a protein on the surface of coronaviruses that allows it to attach to our cells – was helpful in developing mRNA vaccines for COVID.
It would seem likely there will be further coronavirus pandemics in the future. And even if they don’t occur at the scale of COVID, the impacts can be significant. For example, when MERS spread to South Korea in 2015, it only caused 186 cases over two months, but the cost of controlling it was estimated at US$8 billion (A$11.6 billion).
COVID could be regarded as an ‘unknown known’. Markus Spiske/Pexels The 25 viral families: an approach to ‘known unknowns’
Attention has now turned to the known unknowns. There are about 120 viruses from 25 families that are known to cause human disease. Members of each viral family share common properties and our immune systems respond to them in similar ways.
An example is the flavivirus family, of which the best-known members are yellow fever virus and dengue fever virus. This family also includes several other important viruses, such as Zika virus (which can cause birth defects when pregnant women are infected) and West Nile virus (which causes encephalitis, or inflammation of the brain).
The WHO’s blueprint for epidemics aims to consider threats from different classes of viruses and bacteria. It looks at individual pathogens as examples from each category to expand our understanding systematically.
The US National Institute of Allergy and Infectious Diseases has taken this a step further, preparing vaccines and therapies for a list of prototype pathogens from key virus families. The goal is to be able to adapt this knowledge to new vaccines and treatments if a pandemic were to arise from a closely related virus.
Pathogen X, the ‘unknown unknown’
There are also the unknown unknowns, or “disease X” – an unknown pathogen with the potential to trigger a severe global epidemic. To prepare for this, we need to adopt new forms of surveillance specifically looking at where new pathogens could emerge.
In recent years, there’s been an increasing recognition that we need to take a broader view of health beyond only thinking about human health, but also animals and the environment. This concept is known as “One Health” and considers issues such as climate change, intensive agricultural practices, trade in exotic animals, increased human encroachment into wildlife habitats, changing international travel, and urbanisation.
This has implications not only for where to look for new infectious diseases, but also how we can reduce the risk of “spillover” from animals to humans. This might include targeted testing of animals and people who work closely with animals. Currently, testing is mainly directed towards known viruses, but new technologies can look for as yet unknown viruses in patients with symptoms consistent with new infections.
We live in a vast world of potential microbiological threats. While influenza and coronaviruses have a track record of causing past pandemics, a longer list of new pathogens could still cause outbreaks with significant consequences.
Continued surveillance for new pathogens, improving our understanding of important virus families, and developing policies to reduce the risk of spillover will all be important for reducing the risk of future pandemics.
This article is part of a series on the next pandemic.
Allen Cheng, Professor of Infectious Diseases, Monash University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
Apple vs Apricot – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
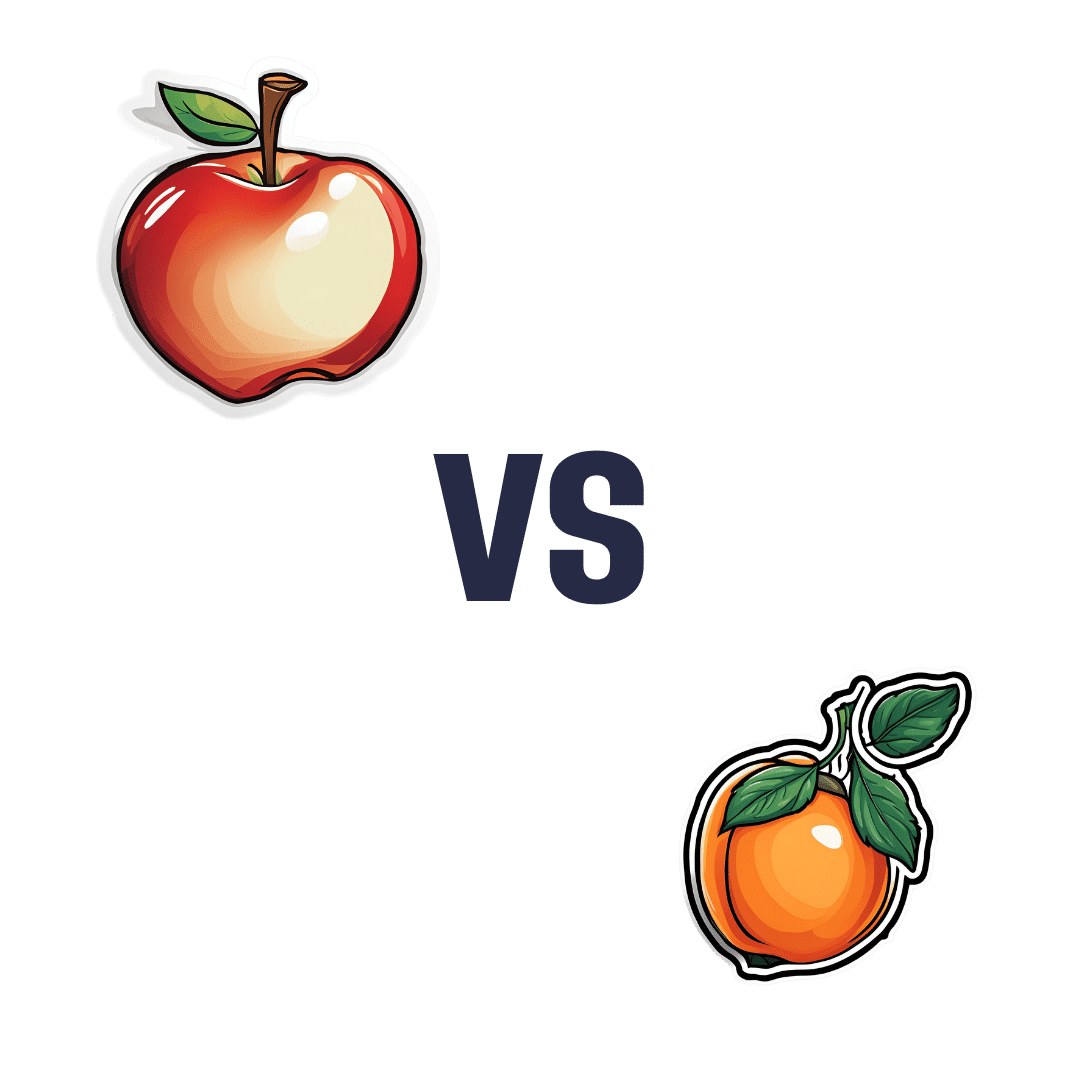
When comparing apple to apricot, we picked the apricot.
Why?
In terms of macros, there’s not too much between them; apples are higher in carbs and only a little higher in fiber, which disparity makes for a slightly higher glycemic index, but it’s not a big difference and they are both low GI foods.
Micronutrients, however, set these two fruits apart:
In the category of vitamins, apple is a tiny bit higher in choline, while apricots are higher in vitamins A, B1, B2, B3, B5, B6, B9, C, E, and K—in most cases, by quite large margins, too. All in all, a clear and easy win for apricots.
When it comes to minerals, apples are not higher in any minerals, while apricots are higher in calcium, copper, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc. There’s simply no contest here.
In short, if an apple a day keeps the doctor away, then an apricot will give the doctor a nice weekend break somewhere.
Want to learn more?
You might like to read:
Top 8 Fruits That Prevent & Kill Cancer
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How Intermittent Fasting Reduces Heart Attack Risk (Directly, Not Via Weight Control!)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve written before about the benefits of intermittent fasting, such as:
- Intermittent Fasting: What’s The Truth?
- 16/8 Intermittent Fasting For Beginners
- Before You Eat Breakfast: 3 Surprising Facts About Intermittent Fasting
Intermittent fasting is mostly enjoyed for its metabolic benefits, such as How To Prevent And Reverse Type 2 Diabetes.
We also covered a very related topic, with intermittent fasting once again being on the suggestions list:
Improve Your Insulin Sensitivity! ← this is actually more important even that blood sugar control itself, important as that latter is!
So, how does it work to reduce heart attack risk?
While intermittent fasting can be used as a weight loss tool (it also doesn’t have to be—it depends on what you eat and what you’re doing in terms of exercise, amongst other factors), this isn’t about that.
Although it is also worth mentioning that intermittent fasting does reduce the risks associated with diabetes, hypercholesterolemia, cancer, Alzheimer’s, and more, as well as generally improving cardiovascular health by reducing blood pressure, cholesterol, and insulin resistance, amongst other metrics.
However, this is about platelet aggregation. Or in whole: platelet activation, aggregation, and thrombosis.
A team of scientists, Dr. Shimo Dai et al., investigated the effects of alternate-day intermittent fasting on platelets and thrombosis, in two quite different, but both important, demographics:
- Humans with coronary artery disease
- Mice with the ApoE gene (the Alzheimer’s risk gene)
Why the mice? Because they wanted to check the level of cerebral ischemia-reperfusion injury (the damage that occurs after a stroke), and no ethics board will let scientists slice up human participants brains at will.
In both cases, the intermittent fasting group enjoyed protective effects that the control group (ad libitum eating) did not.
Specifically, reduced platelet activation, as well as reduced platelet aggregation. Just to be clear:
- Platelet activation = platelets getting deployed
- Platelet aggregation = platelets sticking together
Both are required for thrombosis, which occurs when the platelets, having been activated and aggregated (which is their job, for example to stop bleeding in the case of an injury), block one or more blood vessels.
A healthy level of platelet activation and aggregation rests in the sweet spot wherefrom it can stop bleeding, without stopping blood circulation.
This was found to be associated with increased levels of indole-3-propionic acid (IPA), which is created by certain gut bacteria (C. sporogenes), who proliferate enthusiastically during intermittent fasting.
In few words:
- intermittent fasting triggers the C. sporogenes to proliferate,
- which increases IPA levels,
- which reduces platelet activation and aggregation,
- which reduces the risk of thrombosis,
- and thus reduces the risk of heart attack.
We may hypothesize that this may be a reason to not do intermittent fasting if you have a bleeding disorder, and consult your doctor if you’re on blood thinners.
For everyone else, this is one more thing that makes intermittent fasting a very healthful practice!
You can find the paper itself here:
And here’s a pop-science article that gets more technical than we have, if you’d like a middle-ground in terms of complexity:
Intermittent fasting cuts heart attack risk by preventing dangerous blood clots
Want to try intermittent fasting, but it sounds hard?
Check out this:
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Secret to Mental Health – by George Pransky
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This book (and its author) have a sizeable popular following, so it definitely can be said that it has been well-received by many people. The premise in this book is that there is fundamentally nothing wrong with anybody’s brain, and rather everything can be broken down into:
- Mind (the energy and intelligence that animates all life)
- Consciousness (the capacity to be aware of one’s life and experiences)
- Thought (the ability to think, allowing individuals to create their personal experience of reality)
The author explains, over the course of 145 pages, that where anyone with any perceived mental health issue is going wrong is by either lacking self-awareness (Consciousness) or erring by creating an undesirable personal experience of reality (Thought).
In terms of the science of this, frequent references are made to “there is evidence that shows”, “new discoveries about mental health suggest…”, etc, but this claimed evidence is never actually presented, just alluded to. Where many books would have a bibliography, this one has simply a collection of what the author has titled “interesting case studies, conversations, papers, and discussions” (there are no actual case studies or papers; it is just a collection of anecdotes).
The style is… Honestly, in this reviewer’s opinion, barely readable. But, apparently lots of people love it, so your mileage may vary.
We don’t usually delve too far into claimed credentials, but because of the interesting writing style and the bold claims without evidence, we were curious as to where this PhD came from, and apparently it came from a now-shut-down diploma mill that was described by the court as “a complete scam”.
Bottom line: we can’t recommend this one, but we read it so that you don’t have to, and we hope that publishing this review will help reassure you that when we do recommend a book, we mean it!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: