White Potato vs Sweet Potato – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing white potatoes to sweet potatoes, we picked the sweet potatoes.
Why?
In terms of macros, sweet potatoes are a little lighter on carbs and calories, though in the case of sugar and fiber, sweet potato has a few grams more of each, per potato. However, when an average sweet potato’s 7g of sugar are held against its 4g of fiber, this (much like with fruit!) not a sugar you need to avoid.
See also: Which Sugars Are Healthier, And Which Are Just The Same?
The glycemic index of a sweet potato is also lower than that of a white potato, so the sugars it does have are slower-release.
Sweet potatoes famously are good sources of vitamin A and beta-carotene, which important nutrients white potatoes cannot boast.
Both plants are equally good sources of potassium and vitamin C.
Summary
Both are good sources of many nutrients, and any nutritional health-hazards associated with them come with the preparation (for example, frying introduces unhealthy fats, and mashing makes the glycemic index skyrocket, and cooking with salt increases the salt content).
Baking either is great (consider stuffing them with delicious well-seasoned beans and/or tomatoes; if you make it yourself, pesto can be a great option too, as can cheese if you’re so-inclined and judicious with choice and quantity) and preserves almost all of their nutrients. Remember that nearly 100% of the fiber is in the skin, so you do want to eat that.
The deciding factor is: sweet potatoes are good sources of a couple more valuable nutrients that white potatoes aren’t, and come out as the overall healthiest for that reason.
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Falling vaccination rates put children at risk of preventable diseases. Governments need a new strategy to boost uptake
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Child vaccination is one of the most cost-effective health interventions. It accounts for 40% of the global reduction in infant deaths since 1974 and has led to big health gains in Australia over the past two decades.
Australia has been a vaccination success story. Ten years after we begun mass vaccination against polio in 1956, it was virtually eliminated. Our child vaccination rates have been among the best in the world.
But after peaking in 2020, child vaccination in Australia is falling. Governments need to implement a comprehensive strategy to boost vaccine uptake, or risk exposing more children to potentially preventable infectious diseases.
Yuri A/Shutterstock Child vaccination has been a triumph
Thirty years ago, Australia’s childhood vaccination rates were dismal. Then, in 1997, governments introduced the National Immunisation Program to vaccinate children against diseases such as diphtheria, tetanus, and measles.
Measures to increase coverage included financial incentives for parents and doctors, a public awareness campaign, and collecting and sharing local data to encourage the least-vaccinated regions to catch up with the rest of the country.
What followed was a public health triumph. In 1995, only 52% of one-year-olds were fully immunised. By 2020, Australia had reached 95% coverage for one-year-olds and five-year-olds. At this level, it’s difficult even for highly infectious diseases, such as measles, to spread in the community, protecting both the vaccinated and unvaccinated.
By 2020, 95% of children were vaccinated. Drazen Zigic/Shutterstock Gaps between regions and communities closed too. In 1999, the Northern Territory’s vaccination rate for one-year-olds was the lowest in the country, lagging the national average by six percentage points. By 2020, that gap had virtually disappeared.
The difference between vaccination rates for First Nations children and other children also narrowed considerably.
It made children healthier. The years of healthy life lost due to vaccine-preventable diseases for children aged four and younger fell by nearly 40% in the decade to 2015.
Some diseases have even been eliminated in Australia.
Our success is slipping away
But that success is at risk. Since 2020, the share of children who are fully vaccinated has fallen every year. For every child vaccine on the National Immunisation Schedule, protection was lower in 2024 than in 2020.
Gaps between parts of Australia are opening back up. Vaccination rates in the highest-coverage parts of Australia are largely stable, but they are falling quickly in areas with lower vaccination.
In 2018, there were only ten communities where more than 10% of one-year-old children were not fully vaccinated. Last year, that number ballooned to 50 communities. That leaves more areas vulnerable to disease and outbreaks.
While Noosa, the Gold Coast Hinterland and Richmond Valley (near Byron Bay) have persistently had some of the country’s lowest vaccination rates, areas such as Manjimup in Western Australia and Tasmania’s South East Coast have recorded big declines since 2018.
Missing out on vaccination isn’t just a problem for children.
One preprint study (which is yet to be peer-reviewed) suggests vaccination during pregnancy may also be declining.
Far too many older Australians are missing out on recommended vaccinations for flu, COVID, pneumococcal and shingles. Vaccination rates in aged care homes for flu and COVID are worryingly low.
What’s going wrong?
Australia isn’t alone. Since the pandemic, child vaccination rates have fallen in many high-income countries, including New Zealand, the United Kingdom and the United States.
Globally, in 2023, measles cases rose by 20%, and just this year, a measles outbreak in rural Texas has put at least 13 children in hospital.
Alarmingly, some regions in Australia have lower measles vaccination than that Texas county.
The timing of trends here and overseas suggests things shifted, or at least accelerated, during the pandemic. Vaccine hesitancy, fuelled by misinformation about COVID vaccines, is a growing threat.
This year, vaccine sceptic Robert F. Kennedy Jr was appointed to run the US health system, and Louisiana’s top health official has reportedly cancelled the promotion of mass vaccination.
In Australia, a recent survey found 6% of parents didn’t think vaccines were safe, and 5% believed they don’t work.
Those concerns are far more common among parents with children who are partially vaccinated or unvaccinated. Among the 2% of parents whose children are unvaccinated, almost half believe vaccines are not safe for their child, and four in ten believe vaccines didn’t work.
Other consequences of the pandemic were a spike in the cost of living, and a health system struggling to meet demand. More than one in ten parents said cost and difficulty getting an appointment were barriers to vaccinating their children.
There’s no single cause of sliding vaccination rates, so there’s no one solution. The best way to reverse these worrying trends is to work on all the key barriers at once – from a lack of awareness, to inconvenience, to lack of trust.
What governments should do
Governments should step up public health campaigns that counter misinformation, boost awareness of immunisation and its benefits, and communicate effectively to low-vaccination groups. The new Australian Centre for Disease Control should lead the charge.
Primary health networks, the regional bodies responsible for improving primary care, should share data on vaccination rates with GPs and pharmacies. These networks should also help make services more accessible to communities who are missing out, such as migrant groups and disadvantaged families.
State and local governments should do the same, sharing data and providing support to make maternal child health services and school-based vaccination programs accessible for all families.
Governments can communicate better about the benefits of vaccination. Yuri A/Shutterstock Governments should also be more ambitious about tackling the growing vaccine divides between different parts of the country. The relevant performance measure in the national vaccination agreement is weak. States must only increase five-year-old vaccination rates in four of the ten areas where it is lowest. That only covers a small fraction of low-vaccination areas, and only the final stage of child vaccination.
Australia needs to set tougher goals, and back them with funding.
Governments should fund tailored interventions in areas with the lowest rates of vaccination. Proven initiatives include training trusted community members as “community champions” to promote vaccinations, and pop-up clinics or home visits for free vaccinations.
At this time of year, childcare centres and schools are back in full swing. But every year, each new intake has less protection than the previous cohort. Governments are developing a new national vaccination strategy and must seize the opportunity to turn that trend around. If it commits to a bold national plan, Australia can get back to setting records for child vaccination.
Peter Breadon, Program Director, Health and Aged Care, Grattan Institute and Wendy Hu, Associate, Health Program, Grattan Institute
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
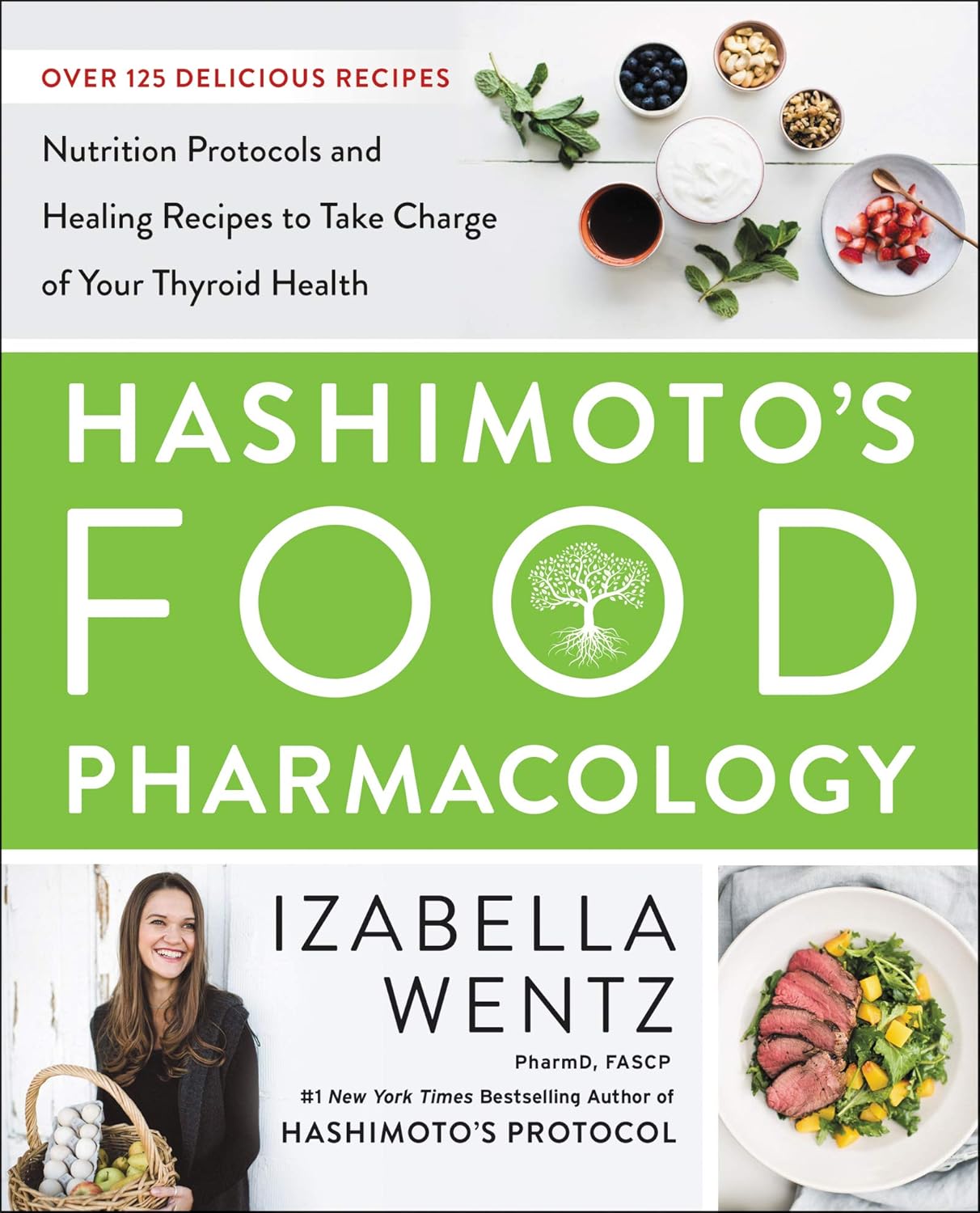
Hashimoto’s Food Pharmacology – by Dr. Izabella Wentz
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The author is a doctor of pharmacology, and we’ve featured her before as an expert on Hashimoto’s, which she has. She has recommendations about specific blood tests and medications, but in this book she’s mainly focussing on what she calls the “three Rs” of managing hypothyroidism:
- Remove the causes and triggers of your hypothyroidism, so far as possible
- Repair the damage caused to your body, especially your gut
- Replace the thyroid hormones and related things in which your body has become deficient
To this end, she provides recipes that avoid processed meats and unfermented dairy, and include plenty of nutrient-dense whole foods specifically tailored to meet the nutritional needs of someone with hypothyroidism.
A nice bonus of the presentation of recipes (of which there are 125, if we include things like “mint tea” and “tomato sauce” and “hot lemon water” as recipes) is explaining the thyroid-supporting elements of each recipe.
A downside for some will be that if you are vegetarian/vegan, this book is very much not, and since many recipes are paleo-style meat dishes, substitutions will change the nutritional profile completely.
Bottom line: if you have hypothyroidism (especially if: Hashimoto’s) and like meat, this will be a great recipe book for you.
Click here to check out Hashimoto’s Food Pharmacology, and get cooking!
Share This Post
-
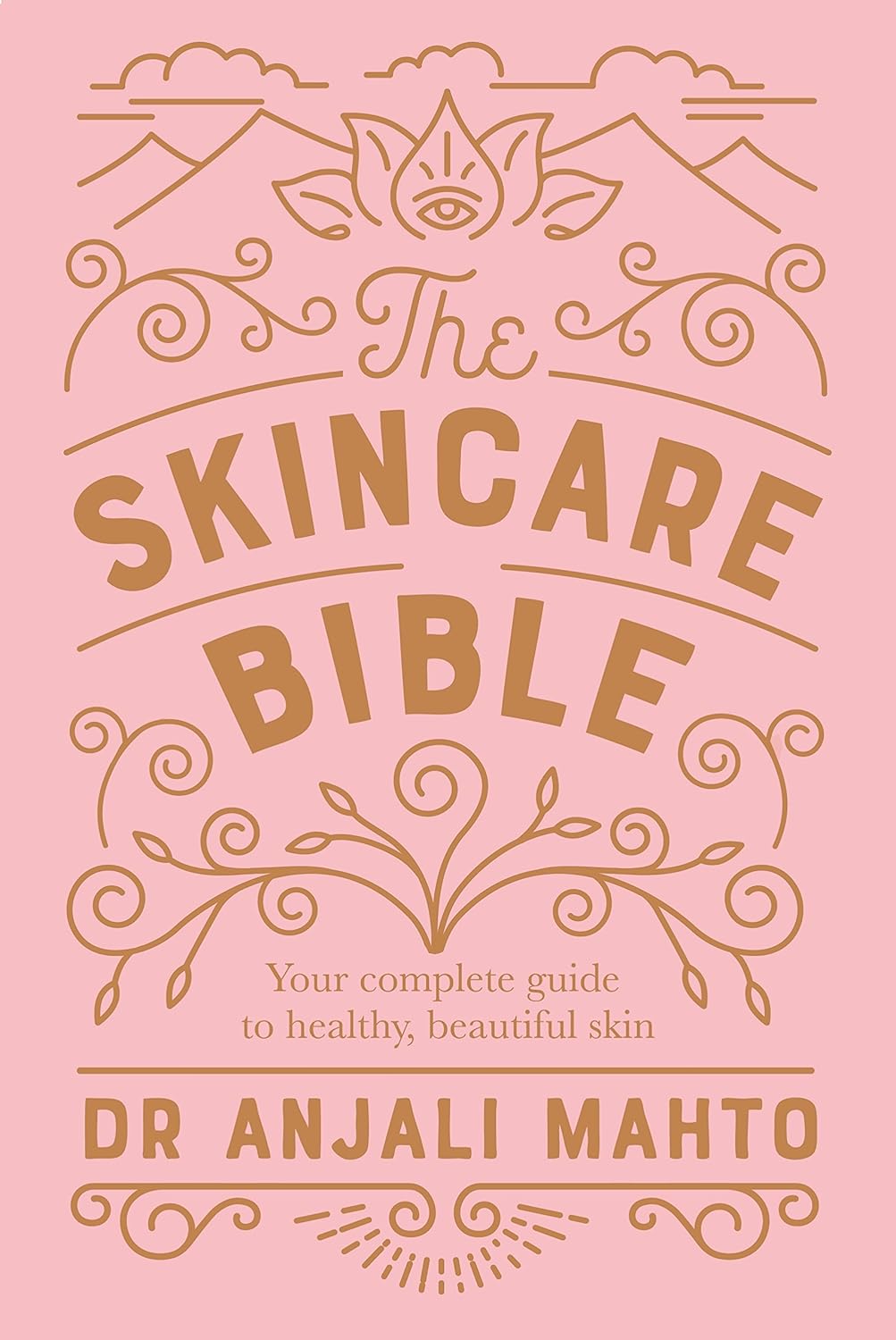
The Skincare Bible − by Dr. Anjali Mahto
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The subtitle claims this to be a “no-nonsense guide to great skin”, and while subtitle claims can often wildly overstate what’s being delivered, in this case, the book really is a no-nonsense guide to great skin.
The author is a dermatologist, and as such she speaks from her professional knowledge and experience, which is a lot more reliable than someone’s latest hack on TikTok.
She gives a quick crash course on what skin actually is and how it works, giving time to genetic considerations, cellular matters, and the grander-scale physical issues at hand, as well as what things affect it and how, ranging from diet to UV light to hormones and more.
We also get a clear explanation of regular skincare as well as specific skin concerns, ranging from minor inconveniences to skin cancer.
You may wonder if she covers anti-aging treatments, and yes, she does.
The style is (as indeed promised by the subtitle) no-nonsense, insofar as it’s straight to the point, no hype, and no padding, just plenty of information-dense content while still being very readable.
Bottom line: if you’d like to seriously look after your skin but aren’t a fan of every latest trend, this book will be a welcome guide.
Click here to check out The Skincare Bible, and enjoy great skin!
Share This Post
Related Posts
-
Antidepressants: Personalization Is Key!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Antidepressants: Personalization Is Key!
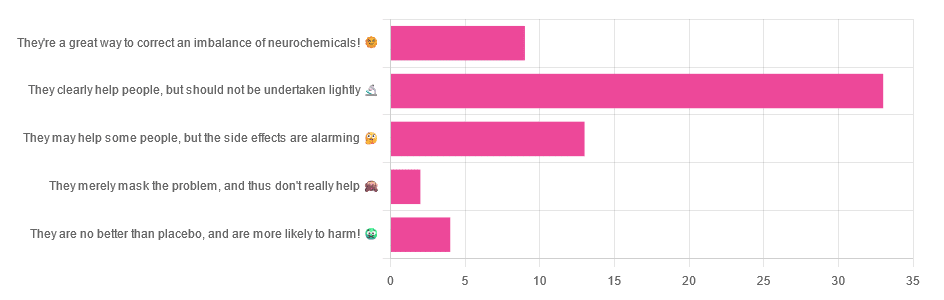
Yesterday, we asked you for your opinions on antidepressants, and got the above-depicted, below-described, set of responses:
- Just over half of respondents said “They clearly help people, but should not be undertaken lightly”
- Just over a fifth of respondents said “They may help some people, but the side effects are alarming”
- Just under a sixth of respondents said “They’re a great way to correct an imbalance of neurochemicals”
- Four respondents said “They are no better than placebo, and are more likely to harm”
- Two respondents said “They merely mask the problem, and thus don’t really help”
So what does the science say?
❝They are no better than placebo, and are more likely to harm? True or False?❞
True or False depending on who you are and what you’re taking. Different antidepressants can work on many different systems with different mechanisms of action. This means if and only if you’re not taking the “right” antidepressant for you, then yes, you will get only placebo benefits:
- Placebo Effect in the Treatment of Depression and Anxiety ← randomly assigned antidepressants are, shockingly, luck of the draw in usefulness
- Antidepressants versus placebo in major depression: an overview ← “wow this science is messy”
- Comparative efficacy and acceptability of 21 antidepressant drugs: a systematic review and network meta-analysis ← “oh look, it makes a difference which antidepressant we give to people”
Rather than dismissing antidepressants as worthless, therefore, it is a good idea to find out (by examination or trial and error) what kind of antidepressant you need, if you indeed do need such.
Otherwise it is like getting a flu shot and being surprised when you still catch a cold!
❝They merely mask the problem, and thus don’t really help: True or False?❞
False, categorically.
The problem in depressed people is the depressed mood. This may be influenced by other factors, and antidepressants indeed won’t help directly with those, but they can enable the person to better tackle them (more on this later).
❝They may help some people, but the side-effects are alarming: True or False?❞
True or False depending on more factors than we can cover here.
Side-effects vary from drug to drug and person to person, of course. As does tolerability and acceptability, since to some extent these things are subjective.
One person’s dealbreaker may be another person’s shrugworthy minor inconvenience at most.
❝They’re a great way to correct an imbalance of neurochemicals: True or False?❞
True! Contingently.
That is to say: they’re a great way to correct an imbalance of neurochemicals if and only if your problem is (at least partly) an imbalance of neurochemicals. If it’s not, then your brain can have all the neurotransmitters it needs, and you will still be depressed, because (for example) the other factors* influencing your depression have not changed.
*common examples include low self-esteem, poor physical health, socioeconomic adversity, and ostensibly bleak prospects for the future.
For those for whom the problem is/was partly a neurochemical imbalance and partly other factors, the greatest help the antidepressants give is getting the brain into sufficient working order to be able to tackle those other factors.
Want to know more about the different kinds?
Here’s a helpful side-by-side comparison of common antidepressants, what type they are, and other considerations:
Mind | Comparing Antidepressants
Want a drug-free approach?
You might like our previous main feature:
The Mental Health First-Aid That You’ll Hopefully Never Need
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Getting COMFY – by Jordan Gross
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s easy to see how good “morning people” seem to have it; it’s harder, it seems, to become one.
And, if we’re forced by circumstance to be the morning person we’re not? We all-too-easily find ourselves greeting each coming day without the joy that, in an ideal world, we might.
So, is it possible to learn this power? Jordan Gross has it mapped out for it us…
The “COMFY” of the title is indeed an acronym, and it stands for:
- Calm
- Openness
- Movement
- Funny
- You
There’s a chapter explaining each in detail, and they’re bookended with other chapters explaining more about the whys and the hows.
As you might expect, the key to a good morning starts the night before, but there’s also a formula to follow. Of course, you can change it up, mix and match if you like… but this book provides a base framework to build from, which is something that can make a huge difference!
Bottom line: it’s a highly enjoyable book to read, and also provides genuine powerful help to bring us the brighter happier mornings we deserve—the set-up to the perfect day!
Click here to check out “Getting COMFY” and perk up your mornings—you deserve it!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Heart Healthy Diet Plan – by Stephen William
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve covered heart-healthy cooking books before, but variety is good, and boredom is an enemy of health, so let’s shake it up with a fresh stack of recipes!
After a brief overview of the relevant science (which if you’re a regular 10almonds reader, probably won’t be new to you), the author takes the reader on a 28-day journey. Yes, we know the subtitle says 30 days, but unless they carefully hid the other two days somewhere we didn’t find, there are “only” 28 inside. Perhaps the publisher heard it was a month and took creative license. Or maybe there’s a different edition. Either way…
Rather than merely giving a diet plan (though yes, he also does that), he gives a wide range of “spotlight ingredients”, such that many of the recipes, while great in and of themselves, can also be jumping-off points for those of us who like to take recipes and immediately do our own things to them.
Each day gets a breakfast, lunch, dinner, and he also covers drinks, desserts, and such like.
Notwithstanding the cover art being a lot of plants, the recipes are not entirely plant-based; there are a selection of fish dishes (and other seafood, e.g. shrimp) and also some dairy products (e.g. Greek yoghurt). The recipes are certainly very “plant-forward” though and many are just plants. If you’re a strict vegan though, this probably isn’t the book for you.
Bottom line: if you’d like to cook heart-healthy but are often stuck wondering “aaah, what to cook again today?”, then this is the book to get you out of any culinary creative block!
Click here to check out the Heart Healthy Diet Plan, and widen your heart-healthy repertoire!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: