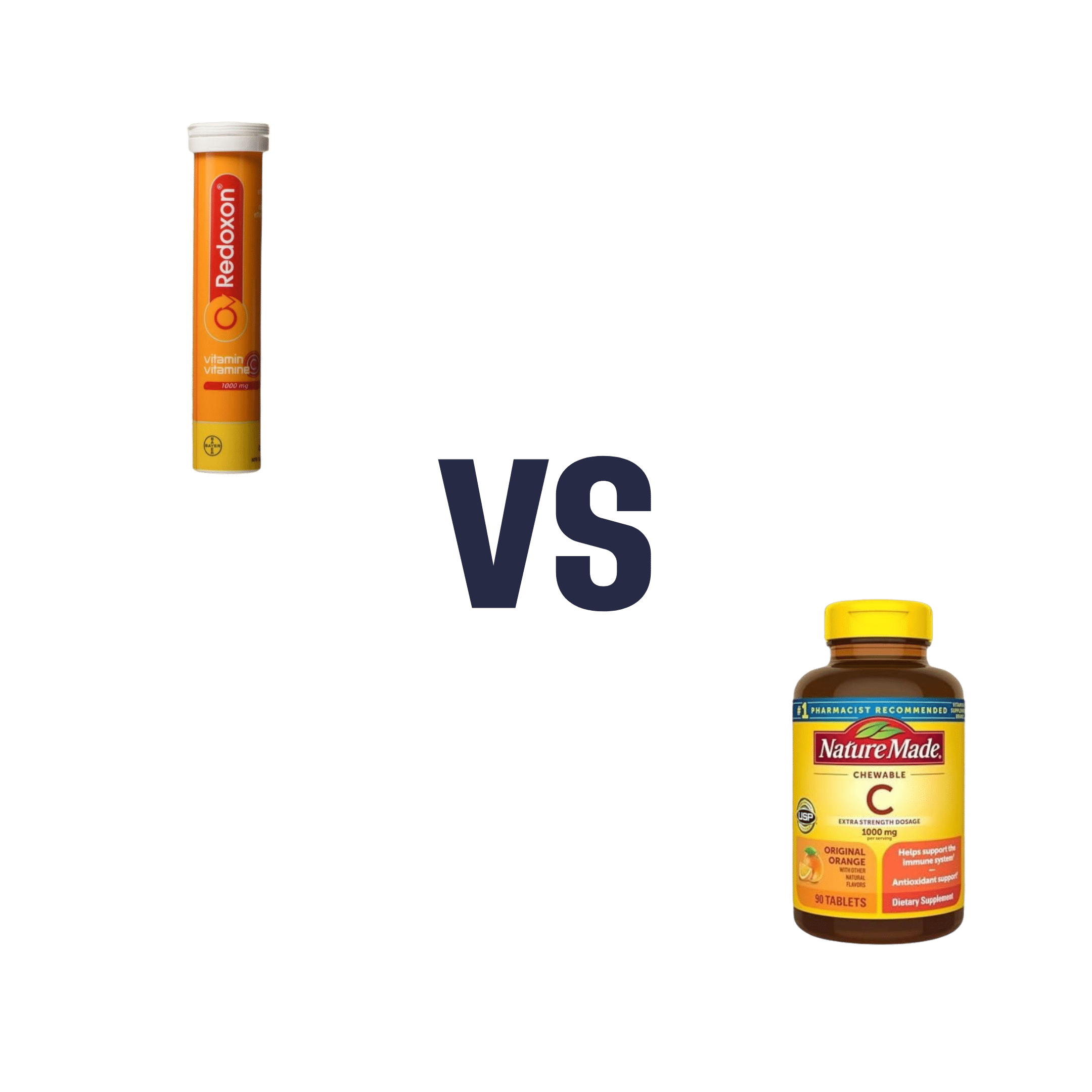
Vitamin C (Drinkable) vs Vitamin C (Chewable) – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing vitamin C (drinkable) to vitamin C (chewable), we picked the drinkable.
Why?
First let’s look at what’s more or less the same in each:
- The usable vitamin C content is comparable
- The bioavailability is comparable
- The additives to hold it together are comparable
So what’s the difference?
With the drinkable, you also drink a glass of water
If you’d like to read more about how to get the most out of the vitamins you take, you can do so here:
Are You Wasting Your Vitamins? Maybe, But You Don’t Have To
If you’d like to get some of the drinkable vitamin C, here’s an example product on Amazon
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
What is silicosis and what does research say about it?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Silicosis is a progressive, debilitating and sometimes fatal lung disease caused by breathing silica dust from cutting, drilling, chipping or grinding materials such as granite, sandstone, slate or artificial stone. The dust gets trapped in the lung tissue, causing inflammation, scarring and permanent damage.
Silicosis is a job-related lung disease and has no cure. The disease mostly affects workers in construction, stone countertop fabrication, mining, and even those who sandblast and stonewash denim jeans to create a ‘worn out’ look.
Silica is one of the most common minerals in nature. About 59% of the Earth’s crust is made of silica, found in quartz, granite, sandstone, slate and sand. Historically, people at the highest risk for the disease have worked in natural environments — mining, digging tunnels or doing quarry work. The disease was first documented by the Greek physician Hippocrates, who in 430 B.C. described breathing disorders in metal diggers.
But in recent decades there’s been renewed attention to the disease due to its more rapid progression and severity among younger workers. Research has shown that the culprit is artificial stone mostly used for countertops for kitchens and bathrooms, which has a very high silica content.
The new generation of coal miners is also at an increased risk of silicosis, in addition to black lung, because layers of coal have become thinner, forcing them to dig deeper into rock, as explained in a joint investigation by the Pittsburgh Post-Gazette and the Medill Investigative Lab at Northwestern University published on Dec. 4. CBS Sunday Morning also had a report on the same issue among West Virginia coal miners, aired as part of its Dec. 10 episode.
Silicosis in modern industries
Artificial, or engineered, stone used for countertops, also known as “quartz,” is formed from finely crushed rocks mixed with resin. Quartz is a natural mineral, but man-made products like many quartz countertops consist of not just quartz, but also resin, colors and other materials that are used to style and strengthen them.
The silica content of artificial stone is about 90%, compared with the 3% silica content of natural marble and 30% silica content in granite stones, according to the authors of a 2019 systematic review published in the International Journal of Environmental Research and Public Health.
The first reported case of silicosis associated with working with artificial stone was from Italy in 2010, according to a 2020 study published in Allergy. Since then, more studies have documented the growing number of cases among artificial stone workers, many of whom are from marginalized populations, such as immigrants.
A July 2023 study published in JAMA Internal Medicine found that in California, the disease mainly occurred among young Latino immigrant men. The disease was severe in most men by the time they sought care.
An August 2022 study, published in Occupational & Environmental Medicine, analyzing the Global Silicosis Registry, with workers in Israel, Spain, Australia and the U.S., found “a substantial emerging population of workers worldwide with severe and irreversible silica-associated diseases,” due to exposure from silica dust from engineered stone.
Other modern occupations such as denim sandblasting, work on dental prostheses, manufacturing of electrical cables and working on jewelry and semi-precious stones also put workers at risk of silicosis.
In the wake of modern-day silicosis cases, researchers have called for larger studies to better understand the disease and the discovery of effective treatments.
In the U.S. about 2.3 million workers are exposed to silica dust on the job, according to the American Lung Association. Other estimates show approximately 10 million workers in India, 3.2 million in the European Union and 2 million in Brazil work with material containing silica.
However, “the reporting system for occupational injuries and illnesses in the United States fails to capture many cases, leading to a poor understanding of silicosis incidence and prevalence,” writes Ryan F. Hoy, who has published extensively on the topic, in a June 2022 article in Respirology.
A 2015 study in the Morbidity & Mortality Weekly Report found the annual number of silicosis deaths declined from 185 people in 1999 to 111 in 2013, but the decline appeared to have leveled off between 2010 and 2013, the authors write. Another 2015 study in MMWR, examining silicosis deaths between 2001 and 2010, found the death rate from silicosis was significantly higher among Black people compared with whites and other races. Men also have a significantly higher death rate from silicosis than women.
The 2019 Global Burden of Disease Study estimates that more than 12,900 people worldwide die from silicosis each year.
Silicosis has no cure, but it’s preventable when workers have access to proper respiratory protection and are educated on safe practices set by regulatory bodies such as the U.S. National Institute for Occupational Safety and Health. The European Network on Silica also has guidelines on handling and using materials containing silica. A March 2023 study published in Environmental Science and Pollution Research International finds that “education, training, and marketing strategies improve respirator use, while training and education motivate workers to use dust control measures.”
Silicosis symptoms and treatment
Symptoms of silicosis include cough, fatigue, shortness of breath and chest pain. There’s no specific test for silicosis. The first signs may show in an abnormal chest X-ray and a slowly developing cough, according to the American Lung Association.
Silicosis symptoms don’t appear right away in most cases, usually taking several years to develop working with silica dust. However, studies indicate that symptoms of silicosis due to exposure to artificial stone appear quicker than exposure to natural silica sources, potentially due to the higher concentration of silica in artificial stone.
There are three types of silicosis: acute (most commonly caused by working with artificial stone), accelerated and chronic, depending on the level of exposure to silica dust, according to the Centers for Disease Control and Prevention, which explains the severity of each type on its website.
Complications from silicosis can include tuberculosis, lung cancer, chronic bronchitis, kidney disease and autoimmune disorders. In some cases, silicosis can cause severe scarring of the lung tissue, leading to a condition called progressive massive fibrosis, or PMF. Some patients may require a lung transplant.
Lung damage from silicosis is irreversible, so treatment of silicosis is aimed at slowing down the disease and relieving its symptoms.
In 1995, the World Health Organization called for the elimination of silicosis by 2030, but research studies and news stories show it remains a threat to many workers.
Below, we have gathered several studies on the topic to help journalists bolster their reporting with academic research.
Research roundup
Artificial Stone Associated Silicosis: A Systematic Review
Veruscka Leso, et al. International Journal of Environmental Research and Public Health, February 2019.This systematic review aims to verify the association between exposure to silica dust in artificial stone and the development of silicosis.
Researchers narrowed down their selection from 75 papers to seven studies that met their inclusion criteria. The seven studies were from Australia, Israel and Spain. Most of the studies are observational and impede a definite association between exposure to silica while working with artificial stone and developing silicosis, the authors note.
However, “the unusually high incidence of the disease that was reported over short periods of investigations, and the comparable occupational histories of affected workers, all being involved in the manufacture and manipulation of engineered stones, may indicate a cause-effect relationship of this type.”
The review of studies reveals a lack of basic preventive measures such as lack of access to disposable masks; lack of information and training on the dangers of silica dust; and lack of periodic medical examinations, including a chest X-ray, among workers. There was limited environmental monitoring of dust levels at the workplace. Also, there was no dust suppression system, such as the use of water when polishing the stones, or effective ventilation. Machinery and tools weren’t properly set up and didn’t undergo routine checks, the authors write.
The authors recommend environmental monitoring for assessing silica levels in the workplace and verifying the effectiveness of personal protections. They also recommend the health surveillance of workers exposed to silica dust.
“Stakeholders, manufacturers, occupational risk prevention services, insurance companies for occupational accidents and diseases, business owners, occupational health physicians, general practitioners, and also employees should be engaged, not only in designing/planning processes and operational working environments, but also in assessing the global applicability of proactive preventive and protective measures to identify and control crystalline silica exposure, especially in new and unexpected exposure scenarios, the full extent of which cannot yet be accurately predicted,” they write.
Silica-Related Diseases in the Modern World
Ryan F. Hoy and Daniel C. Chambers. Allergy, November 2020.The study is a review of the mineralogy of silica, epidemiology, clinical and radiological features of the various forms of silicosis and other diseases associated with exposure to silica.
The primary factor associated with the development of silicosis is the intensity and duration of cumulative exposure to silica dust. Most countries regulate silica dust occupational exposure limits, generally in the range of 0.05 mg/m3 to 0.1 mg/m3, although the risk of dust exposure to workers still remains high at those levels.
The study provides a list of activities that could expose workers to silica dust. They include abrasive blasting of sand and sandstone; cement and brick manufacturing; mixing, glazing or sculpting of china, ceramic and pottery; construction involving bricklaying, concrete cutting, paving and demolition; sandblasting denim jeans; working with and polishing dental materials; mining and related milling; handling raw material during paint manufacturing; road and highway construction and repair; soap and cosmetic production; blasting and drilling tunnels; and waste incineration.
“Despite the large number of workers in the construction sector, there have been few studies of [silica dust] exposure in this industry,” the authors note.
Other than silicosis, conditions associated with silica exposure include sarcoidosis, an inflammatory disease that commonly affects the lungs and lymph nodes, autoimmune disease, lung cancer and pulmonary infections.
“Recent outbreaks of silica-associated disease highlight the need for constant vigilance to identify and control new and well-established sources of silica exposure. While there are currently no effective treatments for silicosis, it is a completely preventable lung disease,” the authors write.
A Systematic Review of the Effectiveness of Dust Control Measures Adopted to Reduce Workplace Exposure
Frederick Anlimah, Vinod Gopaldasani, Catherine MacPhail and Brian Davies. Environmental Science and Pollution Research International, March 2023.This study provides an overview of various interventions and their effectiveness in preventing exposure to silica dust based on a review of 133 studies from 16 countries, including the U.S., Canada, China, India, Taiwan and Australia, and published between 2010 and 2020.
These dust control measures range from simple work practices such as the use of respirators to more sophisticated technologies, such as water and air curtains and foam technology, the authors note.
The review finds increasing research interest in dust reduction, mainly in China. But overall, regulatory influence remains inadequate in preventing miners’ exposure to silica dust.
“Results from the review suggest that adopted interventions increase knowledge, awareness, and attitudes about respirator usage and generate positive perceptions about respirator usage while reducing misconceptions,” the authors write. “Interventions can increase the use, proper use, and frequency of use of respirators and the adoption readiness for dust controls but may not provide sustained motivation in workers for the continual use of dust controls or [personal protective equipment.]”
Notes from the Field: Surveillance of Silicosis Using Electronic Case Reporting — California, December 2022–July 2023
Jennifer Flattery, et al. Morbidity and Mortality Weekly Report, November 2023.This study examines the use of electronic case reporting to identify silicosis cases in California. Electronic case reporting, or eCR, is the automated, real-time exchange of case report information between electronic health records at health facilities at state and local public health agencies in the U.S. It is a joint effort between the Association of Public Health Laboratories, the Council of State and Territorial Epidemiologists, and the CDC. Currently, 208 health conditions can be reported using eCR. All 50 states and other U.S.-affiliated jurisdictions are connected to eCR. Once a public health agency receives a case report, it reaches out to the patient for contact tracing or other actions.
From October 2022 to July 2023, the California Department of Public Health received initial silicosis case reports for 41 individuals. A review of medical records confirmed 19 cases and 16 probable cases. Six of the 41 cases were considered unlikely to be silicosis after a review of medical records.
Notably, engineered stone countertop fabrication was a significant source of exposure, especially among Hispanic and Latino workers.
At least seven of the 19 confirmed cases were associated with the fabrication of engineered stone — quartz — countertops. The 19 patients’ ages ranged from 33 to 51 and all were Hispanic or Latino. One patient died and two had both lungs replaced. One was evaluated for a lung transplant.
The median age of the 35 patients with probable or confirmed silicosis was 65, ranging from 33 to 89 years, and 91% were men.
“It is important that health care providers routinely ask patients about their work as an important determinant of health,” the authors write. “Being aware of the risks associated with work exposures, as well as the regulations, medical monitoring, and prevention strategies that address those risks can help guide patient care.”
Additional research
Understanding the Pathogenesis of Engineered Stone-Associated Silicosis: The Effect of Particle Chemistry on the Lung Cell Response
Chandnee Ramkissoon, et al. Respirology, December 2023.Silicosis, Tuberculosis and Silica Exposure Among Artisanal and Small-Scale Miners: A Systematic Review and Modelling Paper
Patrick Howlett, et al. PLOS Global Public Health, September 2023.Silicosis Among Immigrant Engineered Stone (Quartz) Countertop Fabrication Workers in California
Jane C. Fazio, et al. JAMA Internal Medicine, July 2023.Silicosis and Tuberculosis: A Systematic Review and Meta-Analysis
P. Jamshidi, et al. Pulmonology, June 2023.From Basic Research to Clinical Practice: Considerations for Treatment Drugs for Silicosis
Rou Li, Huimin Kang and Shi Chen. International Journal of Molecular Science, May 2023.Silicosis After Short-Term Exposure
J. Nowak-Pasternak, A. Lipińska-Ojrzanowska and B. Świątkowska. Occupational Medicine, January 2023.Occupational Silica Exposure and Dose-Response for Related Disorders—Silicosis, Pulmonary TB, AIDs and Renal Diseases: Results of a 15-Year Israeli Surveillance
Rachel Raanan, et al. International Journal of Environmental Research and Public Health, November 2022.Demographic, Exposure and Clinical Characteristics in a Multinational Registry of Engineered Stone Workers with Silicosis
Jeremy Tang Hua, et al. Occupational & Environmental Medicine, August 2022.Current Global Perspectives on Silicosis — Convergence of Old and Newly Emergent Hazards
Ryan F. Hoy, et al. Respirology, March 2022.The Association Between Silica Exposure, Silicosis and Tuberculosis: A systematic Review and Metal-Analysis
Rodney Ehrlich, Paula Akugizibwe, Nandi Siegfried and David Rees. BMC Public Health, May 2021.Silicosis, Progressive Massive Fibrosis and Silico-Tuberculosis Among Workers with Occupational Exposure to Silica Dusts in Sandstone Mines of Rajasthan State
Subroto Nandi, Sarang Dhatrak, Kamalesh Sarkar. Journal of Family Medicine and Primary Care, February 2021.Artificial Stone Silicosis: Rapid Progression Following Exposure Cessation
Antonio León-Jiménez, et al. Chest, September 2020.Silica-Associated Lung Disease: An Old-World Exposure in Modern Industries
Hayley Barnes, Nicole S.L. Goh, Tracy L. Leong and Ryan Hoy. Respirology, September 2019.Australia Reports on Audit of Silicosis for Stonecutters
Tony Kirby. The Lancet, March 2019.Artificial Stone-Associated Silicosis: A Rapidly Emerging Occupational Lung Disease
Ryan F. Hoy, et al. Occupational & Environmental Medicine, December 2017.This article first appeared on The Journalist’s Resource and is republished here under a Creative Commons license.
Share This Post
-
Maca Root’s Benefits For The Mood And The Ability
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Maca Root: What It Does And Doesn’t Do
Maca root, or Lepidium meyenii, gets thought of as a root vegetable, though it’s in fact a cruciferous vegetable and more closely related to cabbage—notwithstanding that it also gets called “Peruvian ginseng”.
- Nutritionally, it’s full of all manner of nutrients (vitamins, minerals, fiber, and a wide array of phytochemicals)
- Medicinally, it’s long enjoyed traditional use against a wide variety of illnesses, including respiratory infections and inflammatory diseases.
It’s also traditionally an aphrodisiac.
Is it really anti-inflammatory?
Probably not… Unless fermented. This hasn’t been studied deeply, but a 2023 study found that non-fermented and fermented maca root extracts had opposite effects in this regard:
However, this was an in vitro study, so we can’t say for sure that the results will carry over to humans.
Is it really an aphrodisiac?
Actually yes, it seems so. Here’s a study in which 45 women with antidepressant-induced sexual dysfunction found it significantly improved both libido and sexual function:
❝In summary, maca root may alleviate antidepressant-induced sexual dysfunction as women age, particularly in the domain of orgasm❞
~ Dr. Christina Dording et al.
Read in full: A Double-Blind Placebo-Controlled Trial of Maca Root as Treatment for Antidepressant-Induced Sexual Dysfunction in Women
As for men, well these mice (not technically men) found it beneficial too:
Effects of combined extracts of Lepidium meyenii and Allium tuberosum Rottl. on [e-word] dysfunction
(pardon the censorship; we’re trying to avoid people’s spam filters)
It did also improve fertility (and, actually in real men this time):
Does Lepidium meyenii (Maca) improve seminal quality?
Oh, to be in the mood
Here’s an interesting study in which 3g/day yielded significant mood improvement in these 175 (human) subjects:
And yes, it was found to be “well-tolerated” which is scientist-speak for “this appears to be completely safe, but we don’t want to commit ourselves to an absolutist statement and we can’t prove a negative”.
Oh, to have the energy
As it turns out, maca root does also offer benefits in this regard too:
(that’s not an added ingredient; it’s just a relevant chemical that the root naturally contains)
Want to try some?
We don’t sell it, but here for your convenience is an example product on Amazon 😎
Enjoy!
Share This Post
-
I’m a medical forensic examiner. Here’s what people can expect from a health response after a sexual assault
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
An estimated one in five women and one in 16 men in Australia have experienced sexual violence.
After such a traumatic experience, it’s understandable many are unsure if they want to report it to the police. In fact, less than 10% of Australian women who experience sexual assault ever make a police report.
In Australia there is no time limit on reporting sexual assault to police. However, there are tight time frames for collecting forensic evidence, which can sometimes be an important part of the police investigation, whether it’s commenced at the time or later.
This means the decision of whether or not to undergo a medical forensic examination needs to be made quite quickly after an assault.
I work as a medical forensic examiner. Here’s what you can expect if you present for a medical forensic examination after a sexual assault.
fizkes/Shutterstock A team of specialists
There are about 100 sexual assault services throughout Australia providing 24-hour care. As with other areas of health care, there are extra challenges in regional and rural areas, where there are often further distances to travel and staff shortages.
Sexual assault services in Australia are free regardless of Medicare status. To find your nearest service you can call 1800 RESPECT (1800 737 732) or Full Stop Australia (1800 385 578) who can also provide immediate telephone counselling support.
It’s important to call the local sexual assault service before turning up. They can provide the victim-survivor with information and advice to prevent delays and make the process as helpful as possible.
The consultation usually occurs in a hospital emergency department which has a designated forensic suite, or in a specialised forensic service.
The victim-survivor is seen by a doctor or nurse trained in medical and forensic care. There’s a sexual assault counsellor, crisis worker or social worker present to support the patient and offer counselling advice. This is called an “integrated response” with medical and psychosocial staff working together.
In most cases the victim-survivor can have their own support person present too.
Depending on what the victim-survivor wants, the doctor or nurse will take a history of the assault to guide any medical care which may be needed (such as emergency contraception) and to guide the examination.
Sexual assault services are always very aware of giving victim-survivors a choice about having a medical forensic examination. If a person presents to a sexual assault service, they can receive counselling and medical care without undergoing a forensic examination if they do not wish to. https://www.youtube.com/embed/CGlbTgia0Ek?wmode=transparent&start=0 Sexual assault services are inclusive of all genders.
Collecting forensic samples
Samples collected during a medical forensic examination can sometimes identify the perpetrator’s DNA or intoxicating substances (alcohol or drugs that might be relevant to the investigation). The window of opportunity to collect these samples can be as short as 12 hours, or up to 5–7 days, depending on the nature of the sexual assault.
In most of Australia, an adult who has experienced a recent sexual assault can be offered a medical forensic examination without making a report to police.
Depending on the state or territory, the forensic samples can usually be stored for 3 to 12 months (up to 100 years in Tasmania). This allows the victim-survivor time to decide if they want to release them to police for processing.
The doctor or nurse will collect the samples using a sexual assault investigation kit, or a “rape kit”.
Collecting these samples might involve taking swabs to try to detect DNA from external and internal genital areas and anywhere there may have been DNA transfer. This can be from skin cells, where the perpetrator touched the victim-survivor, or from bodily fluids including semen or saliva.
The doctor or nurse carrying out the examination do their best to minimise re-traumatisation, by providing the victim-survivor information, choices and control at every step of the process.
The victim-survivor can usually have a support person with them. Monkey Business Images/Shutterstock How about STIs and pregnancy?
During the consultation, the doctor or nurse will address any concerns about sexually transmitted infections (STIs) and pregnancy, if applicable.
In most cases the risk of STIs is small. But follow-up testing at 1–2 weeks for infections such as chlamydia and gonorrhoea, and at 6–12 weeks for infections such as syphilis and HIV, is usually recommended.
Emergency contraception (sometimes called the “morning after pill”) can be provided to prevent pregnancy. It can be taken up to five days after sexual assault (but the sooner the better) with follow-up pregnancy testing recommended at 2–3 weeks.
Things have improved over time
When I was a junior doctor in the late 90s, taking forensic swabs was usually the responsibility of the busy obstetrics and gynaecology trainee in the emergency department, who was often managing multiple patients and had little training in forensics. There was also usually no supportive counsellor.
Anecdotally, both the doctor and the patient were traumatised by this experience. Research shows that when specialised, integrated services are not provided, victim-survivors’ feelings of powerlessness are magnified.
But the way we carry out medical forensic examinations after sexual assault in Australia has improved over the years.
With patient-centred practices, and designated forensic and counselling staff, the experience for the patient is thought to be empowering rather than re-traumatising.
Our research
In new research published in the Australian Journal of General Practice, my colleagues and I explored the experience of the medical forensic examination from the victim-survivor’s perspective.
We surveyed 291 patients presenting to a sexual assault service in New South Wales (where I work) over four years.
Some 75% of patients reported the examination was reassuring and another 20% reported it was OK. Only 2% reported that it was traumatising. The majority (98%) said they would recommend a friend present to a sexual assault service if they were in a similar situation.
While patients spoke positively about the care they received, many commented that the sexual assault service was not visible enough. They didn’t know how to find it or even that it existed.
We know many victim-survivors don’t present to a sexual assault service or undergo a medical forensic examination after a sexual assault. So we need to do more to increase the visibility of these services.
The National Sexual Assault, Family and Domestic Violence Counselling Line – 1800 RESPECT (1800 737 732) – is available 24 hours a day, seven days a week for any Australian who has experienced, or is at risk of, family and domestic violence and/or sexual assault.
Mary Louise Stewart, Senior Career Medical Officer, Northern Sydney Local Health District; PhD Candidate, University of Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
When Science Brings Hope
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
There’s a lot of bad news out there at present, including in the field of healthcare. So as some measure of respite from that, here’s some good news from the world of health science, including some actionable things to do:
Run for your life! Or casually meander for your life; that’s fine too.
Those who enjoy the equivalent of an average of 160mins slow (3mph) walking per day also enjoy the greatest healthspan. Now, there may be an element of two-way causality here (moving more means we live longer, but also, sometimes people move less because of having crippling disabilities, which are themselves not great for healthspan, as well as having the knock-on effect of reducing movement, and so such conditions yield and anti-longevity double-whammy), but for any who are able to, increasing the amount of time per day spend moving, ultimately results (on average) in a lot of extra days in life that we’ll then get to spend moving.
Depending on how active or not you are already, every extra 1 hour walked could add two hours and 49 minutes to life expectancy:
Read in full: Americans over 40 could live extra 5 years if they were all as active as top 25% of population, modeling study suggests
Related: The Doctor Who Wants Us To Exercise Less & Move More
Re-teaching your brain to heal itself
Cancer is often difficult to treat, and brain tumors can be amongst the most difficult with which to contend. Not only is everything in there very delicate, but also it’s the hardest place in the body to get at—not just surgically, but even chemically, because of the blood-brain barrier. To make matters worse, brain tumors such as glioblastoma weaken the function of T-cells (whose job it is to eliminate the cancer) by prolonged exposure.
Research has found a way to restore the responsiveness of these T-cells to immune checkpoint inhibitors, allowing them to go about their cancer-killing activities unimpeded:
Read in full: New possibilities for treating intractable brain tumors unveiled
Related: 5 Ways To Beat Cancer (And Other Diseases)
Here’s to your good health!
GLP-1 receptor agonists, originally developed to fight diabetes and now enjoying popularity as weight loss adjuvants, work in large part by cutting down food cravings by interfering with the chemical messaging about such.
As a bonus, it seems that they also can reduce alcohol cravings, especially by targetting the brain’s reward center; this was based on a large review of studies looking at how GLP-1RA use affects alcohol use, alcohol-related health problems, hospital visits, and brain reactions to alcohol cues:
Read in full: Diabetes medication may be effective in helping people drink less alcohol, research finds
Related: How To Reduce Or Quit Alcohol
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Better With Age – by Dr. Alan Castel
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This one isn’t about the biology of aging, so much as (as the subtitle promises) the psychology of it.
Dr. Castel first covers the grounds of what “successful aging” is, and the benefits that can be expected from doing it right. Spoiler, it’s not just “reduced decline”, there are numerous things that actually get better, too.
We also learn how our memory works differently—it can be worse, of course, but it can also be just different, in a way that tends to tie in with vastness of the accumulated knowledge over the years, allowing for easiest access to the things the brain thinks are most important—ranging from expertise in a certain field, to life-experience “wisdom”.
There’s a lot of advice that’s mostly not going to be anything new to regular readers of 10almonds, in terms of staying sharp with an active lifestyle and a well-nourished brain.
The style is very soft pop-science; there are citations dotted throughout, but mostly this is more of a “curl up with a book” book, not a textbook.
In the category of subjective criticism, it can be a little repetitive (but for those who like repetition for ease of learning, you will love this), and his name-dropping habit gets quite eyeroll-worthy quite quickly.
Bottom line: if you’d like to learn about the very many ways in which “over the hill” is simply defeatist pessimism, then this book can help you to ensure you do better.
Click here to check out Better With Age, and get better with age!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Yes, we still need chickenpox vaccines
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
For people who grew up before a vaccine was available, chickenpox is largely remembered as an unpleasant experience that almost every child suffered through. The highly contagious disease tore through communities, leaving behind more than a few lasting scars.
For many children, chickenpox was much more than a week or two of itchy discomfort. It was a serious and sometimes life-threatening infection.
Prior to the chickenpox vaccine’s introduction in 1995, 90 percent of children got chickenpox. Those children grew into adults with an increased risk of developing shingles, a disease caused by the same virus—varicella-zoster—as chickenpox, which lies dormant in the body for decades.
The vaccine changed all that, nearly wiping out chickenpox in the U.S. in under three decades. The vaccine has been so successful that some people falsely believe the disease no longer exists and that vaccination is unnecessary. This couldn’t be further from the truth.
Vaccination spares children and adults from the misery of chickenpox and the serious short- and long-term risks associated with the disease. The CDC estimates that 93 percent of children in the U.S. are fully vaccinated against chickenpox. However, outbreaks can still occur among unvaccinated and under-vaccinated populations.
Here are some of the many reasons why we still need chickenpox vaccines.
Chickenpox is more serious than you may remember
For most children, chickenpox lasts around a week. Symptoms vary in severity but typically include a rash of small, itchy blisters that scab over, fever, fatigue, and headache.
However, in one out of every 4,000 chickenpox cases, the virus infects the brain, causing swelling. If the varicella-zoster virus makes it to the part of the brain that controls balance and muscle movements, it can cause a temporary loss of muscle control in the limbs that can last for months. Chickenpox can also cause other serious complications, including skin, lung, and blood infections.
Prior to the U.S.’ approval of the vaccine in 1995, children accounted for most of the country’s chickenpox cases, with over 10,000 U.S. children hospitalized with chickenpox each year.
The chickenpox vaccine is very effective and safe
Chickenpox is an extremely contagious disease. People without immunity have a 90 percent chance of contracting the virus if exposed.
Fortunately, the chickenpox vaccine provides lifetime protection and is around 90 percent effective against infection and nearly 100 percent effective against severe illness. It also reduces the risk of developing shingles later in life.
In addition to being incredibly effective, the chickenpox vaccine is very safe, and serious side effects are extremely rare. Some people may experience mild side effects after vaccination, such as pain at the injection site and a low fever.
Although infection provides immunity against future chickenpox infections, letting children catch chickenpox to build up immunity is never worth the risk, especially when a safe vaccine is available. The purpose of vaccination is to gain immunity without serious risk.
The chickenpox vaccine is one of the greatest vaccine success stories in history
It’s difficult to overstate the impact of the chickenpox vaccine. Within five years of the U.S. beginning universal vaccination against chickenpox, the disease had declined by over 80 percent in some regions.
Nearly 30 years after the introduction of the chickenpox vaccine, the disease is almost completely wiped out. Cases and hospitalizations have plummeted by 97 percent, and chickenpox deaths among people under 20 are essentially nonexistent.
Thanks to the vaccine, in less than a generation, a disease that once swept through schools and affected nearly every child has been nearly eliminated. And, unlike vaccines introduced in the early 20th century, no one can argue that improved hygiene, sanitation, and health helped reduce chickenpox cases beginning in the 1990s.
Having chickenpox as a child puts you at risk of shingles later
Although most people recover from chickenpox within a week or two, the virus that causes the disease, varicella-zoster, remains dormant in the body. This latent virus can reactivate years after the original infection as shingles, a tingling or burning rash that can cause severe pain and nerve damage.
One in 10 people who have chickenpox will develop shingles later in life. The risk increases as people get older as well as for those with weakened immune systems.
Getting chickenpox as an adult can be deadly
Although chickenpox is generally considered a childhood disease, it can affect unvaccinated people of any age. In fact, adult chickenpox is far deadlier than pediatric cases.
Serious complications like pneumonia and brain swelling are more common in adults than in children with chickenpox. One in 400 adults who get chickenpox develops pneumonia, and one to two out of 1,000 develop brain swelling.
Vaccines have virtually eliminated chickenpox, but outbreaks still happen
Although the chickenpox vaccine has dramatically reduced the impact of a once widespread disease, declining immunity could lead to future outbreaks. A Centers for Disease Control and Prevention analysis found that chickenpox vaccination rates dropped in half of U.S. states in the 2022-2023 school year compared to the previous year. And more than a dozen states have immunization rates below 90 percent.
In 2024, New York City and Florida had chickenpox outbreaks that primarily affected unvaccinated and under-vaccinated children. With declining public confidence in routine vaccines and rising school vaccine exemption rates, these types of outbreaks will likely become more common.
The CDC recommends that children receive two chickenpox vaccine doses before age 6. Older children and adults who are unvaccinated and have never had chickenpox should also receive two doses of the vaccine.
For more information, talk to your health care provider.
This article first appeared on Public Good News and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: