When Doctors Make House Calls, Modern-Style!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
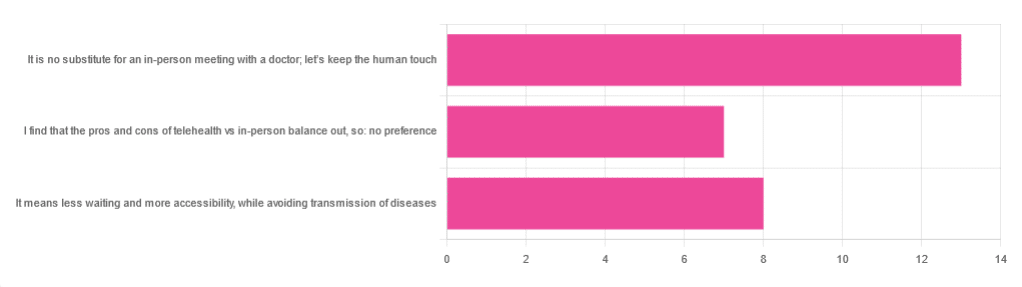
In Tuesday’s newsletter, we asked you foryour opinion of telehealth for primary care consultations*, and got the above-depicted, below-described, set of responses:
- About 46% said “It is no substitute for an in-person meeting with a doctor; let’s keep the human touch”
- About 29% said “It means less waiting and more accessibility, while avoiding transmission of diseases”
- And 25 % said “I find that the pros and cons of telehealth vs in-person balance out, so: no preference”
*We specified that by “primary care” we mean the initial consultation with a non-specialist doctor, before receiving treatment or being referred to a specialist. By “telehealth” we mean by videocall or phonecall.
So, what does the science say?
A quick note first
Because telehealth was barely a thing (statistically speaking) before the first stages of the COVID pandemic, compared to how it is now, most of the science for this is young, and a lot of the science simply hasn’t been done yet, and/or has not been published yet, because the process can take years.
Because of this, some studies we do have aren’t specifically about primary care, and are sometimes about specialists. We think this should not affect the results much, but it bears highlighting.
Nevertheless, we’ll do what we can with the science we have!
Telehealth is more accessible than in-person consultations: True or False?
True, for most people. For example…
❝Data was found from a variety of emergency and non-emergency departments of primary, secondary, and specialised healthcare.
Satisfaction was high among recipients of healthcare, scoring 9-10 on a scale of 0-10 or ranging from 73.3% to 100%.
Convenience was rated high in every specialty examined. Satisfaction of clinicians was high throughout the specialities despite connection failure and concerns about confidentiality of information.❞
whereas…
❝Nonetheless, studies reported perception of increased barriers to accessing care and inequalities for vulnerable patients especially in older people❞
~ Ibid.
Source: Satisfaction with telemedicine use during COVID-19 pandemic in the UK: a systematic review
Now, perception of those things does necessarily equate to an actual increased barrier, but it is reasonable that someone who thinks something is inaccessible will be less inclined to try to access it.
The quality of care provided via telehealth is as good as in-person: True or False?
True, ostensibly, with caveats. The caveats are:
- We’re going offreported patient satisfaction, not objective patient health outcomes (we found little* science as yet for the relative incidence of misdiagnosis, for example—which kind of thing will take time to be revealed).
- We’re also therefore speaking (as statistics do) for the significant majority of people. However, if we happen to be (statistically speaking) an insignificant minority, well, that just sucks for us personally.
*we did find some, but it wasn’t very helpful yet. For example:
An electronic trigger to detect telemedicine-related diagnostic errors
this one does look at the incidence of diagnostic errors, but provides no control group (i.e. otherwise-comparable in-person consultations) for comparison.
While most oft-considered demographic groups reported comparable patient satisfaction (per race, gender, and socioeconomic status, for example), there was one outlier variable, which was age (as we quoted from that first study above).
However!
Looking under the hood of these stats, it seems that age is not the real culprit, so much as technological illiteracy, which is heavily correlated with age:
❝Lower eHealth literacy is associated with more negative attitudes towards I/C technology in healthcare. This trend is consistent across diverse demographics and regions. ❞
Source: Meta-analysis: eHealth literacy and attitudes towards internet/computer technology
There are things that can be done at an in-person consultation that can’t be done by telehealth: True or False?
True, of course. It is incredibly rare that we will cite “common sense”, (as sometimes “common sense” is actually “common mistakes” and is simply and verifiably wrong), but in this case, as one 10almonds subscriber put it:
❝The doctor uses his five senses to assess. This cannot be attained over the phone❞
~ 10almonds subscriber
A quick note first: if your doctor is using their sense of taste to diagnose you, please get a different doctor, because they should definitely not be doing that!
Not in this century, anyway… Once upon a time, diabetes was diagnosed by urine-tasting (and yes, that was a fairly reliable method).
However, nowadays indeed a doctor will use sight, sound, touch, and sometimes even smell.
In a videocall we’re down to two of those senses (sight and sound), and in a phonecall, down to one (sound) and even that is hampered. Your doctor cannot, for example, use a stethoscope over the phone.
With this in mind, it really comes down to what you need from your doctor in that consultation.
- If you’re 99% sure that what you need is to be prescribed an antidepressant, that probably doesn’t need a full physical.
- If you’re 99% sure that what you need is a referral, chances are that’ll be fine by telehealth too.
- If your doctor is 99% sure that what you need is a verbal check-up (e.g. “How’s it been going for you, with the medication that I prescribed for you a month ago?”, then again, a call is probably fine.
If you have a worrying lump, or an unhappy bodily discharge, or an unexplained mysterious pain? These things, more likely an in-person check-up is in order.
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:

Why Psyllium Is Healthy Through-And-Through
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Psyllium is the powder of the husk of the seed of the plant Plantago ovata.
It can be taken as a supplement, and/or used in cooking.
What’s special about it?
It is fibrous, and the fiber is largely soluble fiber. It’s a “bulk-forming laxative”, which means that (dosed correctly) it is good against both constipation (because it’s a laxative) and diarrhea (because it’s bulk-forming).
See also, because this is Research Review Monday and we provide papers for everything:
In other words, it will tend things towards being a 3 or 4 on the Bristol Stool Scale ← this is not pretty, but it is informative.
Before the bowels
Because of how it increases the viscosity of substances it finds itself in, psyllium slows stomach-emptying, and thus improves feelings of satiety.
Here’s a study in which taking psyllium before breakfast and lunch resulted in increased satiety between meals, and reduction in food-related cravings:
Satiety effects of psyllium in healthy volunteers
Prebiotic benefits
We can’t digest psyllium, but our gut bacteria can—somewhat! Because they can only digest some of the psyllium fibers, that means the rest will have the stool-softening effect, while we also get the usual in-gut benefits from prebiotic fiber first too:
The Effect of Psyllium Husk on Intestinal Microbiota in Constipated Patients and Healthy Controls
Cholesterol-binding
Psyllium can bind to cholesterol during the digestive process. Why only “can”? Well, if you don’t consume cholesterol (for example, if you are vegan), then there won’t be cholesterol in the digestive tract to bind to (yes, we do need some cholesterol to live, but like most animals, we can synthesize it ourselves).
What this cholesterol-binding action means is that the dietary cholesterol thus bound cannot enter the bloodstream, and is simply excreted instead:
Heart health beyond cholesterol
Psyllium supplementation can also help lower high blood pressure but does not significantly lower already-healthy blood pressure, so it can be particularly good for keeping things in safe ranges:
❝Given the overarching benefits and lack of reported side effects, particularly for hypertensive patients, health care providers and clinicians should consider the use of psyllium supplementation for the treatment or abatement of hypertension, or hypertensive symptoms.❞
Read in full: The effect of psyllium supplementation on blood pressure: a systematic review and meta-analysis of randomized controlled trials ← you can see the concrete numbers here
Is it safe?
Psyllium is first and foremost a foodstuff, and is considered very safe unless you have an allergy (which is rare, but possible).
However, it is still recommended to start at a low dose and work up, because anything that changes your gut microbiota, even if it changes it for the better, will be easiest if done slowly (or else, you will hear about it from your gut).
Want to try some?
We don’t sell it, but here for your convenience is an example product on Amazon
Enjoy!
Share This Post

6-Minute Core Strength – by Dr. Jonathan Su
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We don’t normally do author biographies here, but in this case it’s worth noting that Dr. Su is a physiotherapist, military rehab expert, and an IAYT yoga therapist. So, these things together certainly do lend weight to his advice.
About the “6-minute” thing: this is in the style of the famous “7-minute workout” and “5 Minutes’ Physical Fitness” etc, and refers to how long each exercise session should take. The baseline is one such session per day, though of course doing more than one set of 6 minutes each time is a bonus if you wish to do so.
The exercises are focused on core strength, but they also include hip and shoulder exercises, since these are after all attached to the core, and hip and shoulder mobility counts for a lot.
A particular strength of the book is in troubleshooting mistakes of the kind that aren’t necessarily visible from photos; in this case, Dr. Su explains what you need to go for in a certain exercise, and how to know if you are doing it correctly. This alone is worth the cost of the book, in this reviewer’s opinion.
Bottom line: if you want core strength and want it simple yet comprehensive, this book can guide you.
Click here to check out 6-Minute Core Strength, and strengthen yours!
Share This Post

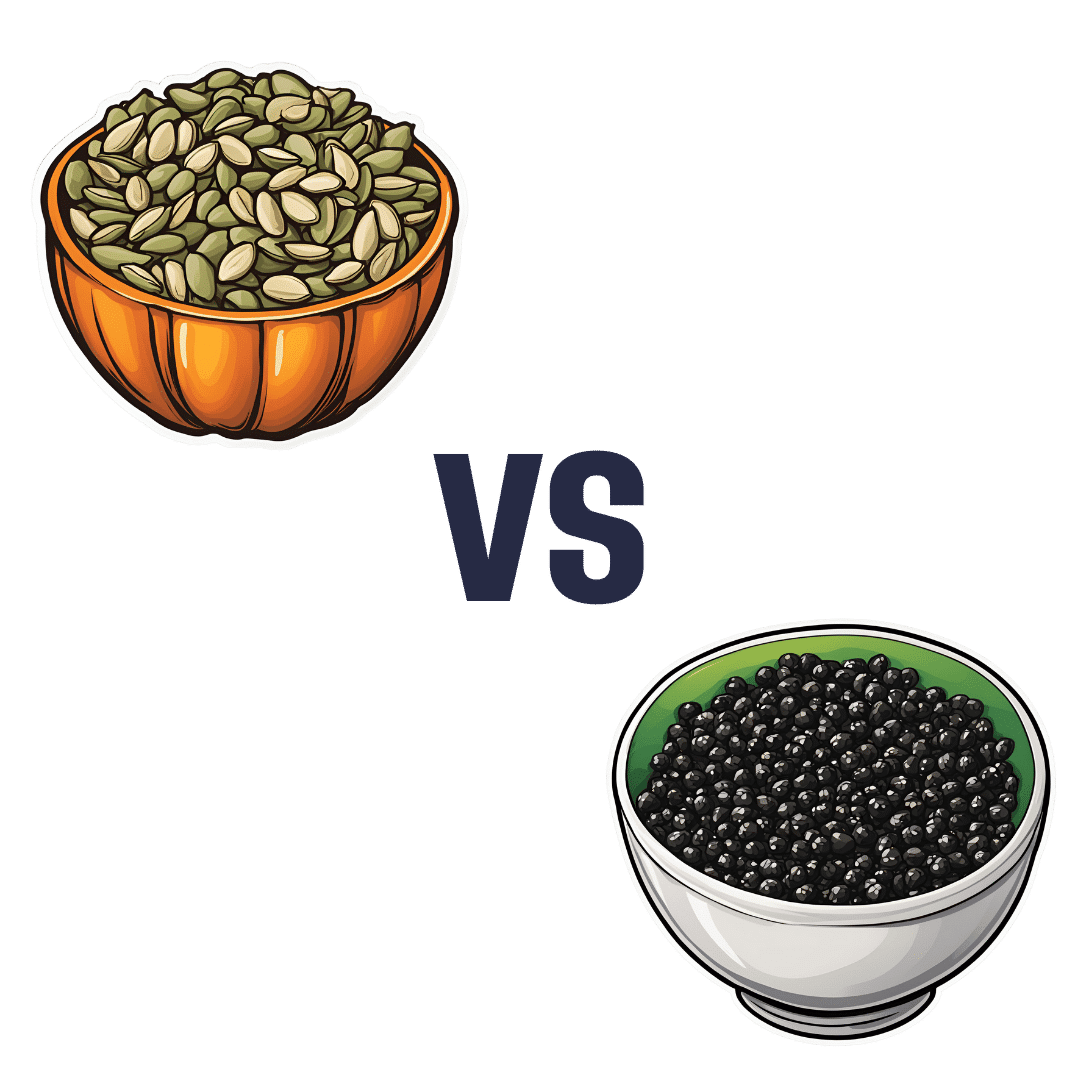
Pumpkin Seeds vs Watermelon Seeds – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing pumpkin seeds to watermelon seeds, we picked the watermelon.
Why?
Starting with the macros: pumpkin seeds have a lot more carbs, while watermelon seeds have a lot more protein, despite pumpkin seeds being famous for such. They’re about equal on fiber. In terms of fats, watermelon seeds are higher in fats, and yes, these are healthy fats, mostly polyunsaturated.
When it comes to vitamins, pumpkin seeds are marginally higher in vitamins A and C, while watermelon seeds are a lot higher in vitamins B1, B2, B3, B5, B6, and B9. An easy win for watermelon seeds here.
In the category of minerals, despite being famous for zinc, pumpkin seeds are higher only in potassium, while watermelon seeds are higher in iron, magnesium, manganese, and phosphorus; the two seeds are equal on calcium, copper, and zinc. Another win for watermelon seeds.
In short, enjoy both, but watermelon has more to offer. Of course, if buying just the seeds and not the whole fruit, it’s generally easier to find pumpkin seeds than watermelon seeds, so do bear in mind that pumpkin seeds’ second place isn’t that bad here—it’s just a case of a very nutritious food looking bad by standing next to an even better one.
Want to learn more?
You might like to read:
Seed Saving Secrets – by Alice Mirren
Take care!
Share This Post
Related Posts

The Surprising Link Between Type 2 Diabetes & Alzheimer’s
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Surprising Link Between Type 2 Diabetes & Alzheimer’s

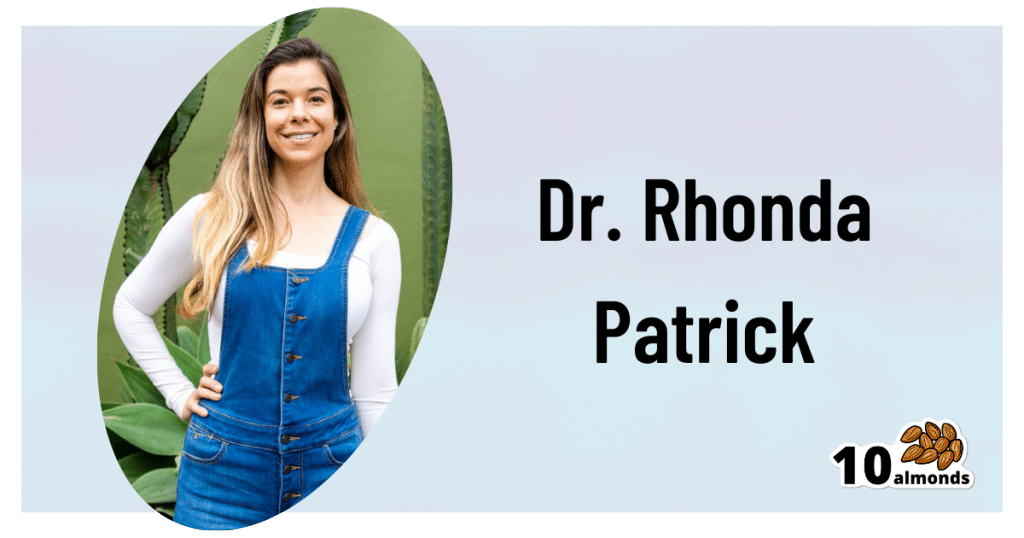
This is Dr. Rhonda Patrick. She’s a biomedical scientist with expertise in the areas of aging, cancer, and nutrition. In the past five years she has expanded her research of aging to focus more on Alzheimer’s and Parkinson’s, as she has a genetic predisposition to both.
What does that genetic predisposition look like? People who (like her) have the APOE-ε4 allele have a twofold increased risk of Alzheimer’s disease—and if you have two copies (i.e., one from each of two parents), the risk can be up to tenfold. Globally, 13.7% of people have at least one copy of this allele.
So while getting Alzheimer’s or not is not, per se, hereditary… The predisposition to it can be passed on.
What’s on her mind?
Dr. Patrick has noted that, while we don’t know for sure the causes of Alzheimer’s disease, and can make educated guesses only from correlations, the majority of current science seems to be focusing on just one: amyloid plaques in the brain.
This is a worthy area of research, but ignores the fact that there are many potential Alzheimer’s disease mechanisms to explore, including (to count only mainstream scientific ideas):
- The amyloid hypothesis
- The tau hypothesis
- The inflammatory hypothesis
- The cholinergic hypothesis
- The cholesterol hypothesis
- The Reelin hypothesis
- The large gene instability hypothesis
…as well as other strongly correlated factors such as glucose hypometabolism, insulin signalling, and oxidative stress.
If you lost your keys and were looking for them, and knew at least half a dozen places they might be, how often would you check the same place without paying any attention to the others?
To this end, she notes about those latter-mentioned correlated factors:
❝50–80% of people with Alzheimer’s disease have type 2 diabetes; there is definitely something going on❞
There’s another “smoking gun” for this too, because dysfunction in the blood vessels and capillaries that line the blood-brain barrier seem to be a very early event that is common between all types of dementia (including Alzheimer’s) and between type 2 diabetes and APOE-ε4.
Research is ongoing, and Dr. Patrick is at the forefront of that. However, there’s a practical take-away here meanwhile…
What can we do about it?
Dr. Patrick hypothesizes that if we can reduce the risk of type 2 diabetes, we may reduce the risk of Alzheimer’s with it.
Obviously, avoiding diabetes if possible is a good thing to do anyway, but if we’re aware of an added risk factor for Alzheimer’s, it becomes yet more important.
Of course, all the usual advices apply here, including a Mediterranean diet and regular moderate exercise.
Three other things Dr. Patrick specifically recommends (to reduce both type 2 diabetes risk and to reduce Alzheimer’s risk) include:
(links are to her blog, with lots of relevant science for each)
You can also hear more from Dr. Patrick personally, as a guest on Dr. Peter Attia’s podcast recently. She discusses these topics in much greater detail than we have room for in our newsletter:
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:

How Useful Are Our Dreams
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What’s In A Dream?
We were recently asked:
❝I have a question or a suggestion for coverage in your “Psychology Sunday”. Dreams: their relevance, meanings ( if any) interpretations? I just wondered what the modern psychological opinions are about dreams in general.❞
~ 10almonds subscriber
There are two main schools of thought, and one main effort to reconcile those two. The third one hasn’t quite caught on so far as to be considered a “school of thought” yet though.
The Top-Down Model (Psychoanalysts)
Psychoanalysts broadly follow the theories of Freud, or at least evolved from there. Freud was demonstrably wrong about very many things. Most of his theories have been debunked and ditched—hence the charitable “or at least evolved from there” phrasing when it comes to modern psychoanalytic schools of thought. Perhaps another day, we’ll go into all the ways Freud went wrong. However, for today, one thing he wasn’t bad at…
According to Freud, our dreams reveal our subconscious desires and fears, sometimes directly and sometimes dressed in metaphor.
Examples of literal representations might be:
- sex dreams (revealing our subconscious desires; perhaps consciously we had not thought about that person that way, or had not considered that sex act desirable)
- getting killed and dying (revealing our subconscious fear of death, not something most people give a lot of conscious thought to most of the time)
Examples of metaphorical representations might be:
- dreams of childhood (revealing our subconscious desires to feel safe and nurtured, or perhaps something else depending on the nature of the dream; maybe a return to innocence, or a clean slate)
- dreams of being pursued (revealing our subconscious fear of bad consequences of our actions/inactions, for example, responsibilities to which we have not attended, debts are a good example for many people; or social contact where the ball was left in our court and we dropped it, that kind of thing)
One can read all kinds of guides to dream symbology, and learn such arcane lore as “if you dream of your teeth crumbling, you have financial worries”, but the truth is that “this thing means that other thing” symbolic equations are not only highly personal, but also incredibly culture-bound.
For example:
- To one person, bees could be a symbol of feeling plagued by uncountable small threats; to another, they could be a symbol of abundance, or of teamwork
- One culture’s “crow as an omen of death” is another culture’s “crow as a symbol of wisdom”
- For that matter, in some cultures, white means purity; in others, it means death.
Even such classically Freudian things as dreaming of one’s mother and/or father (in whatever context) will be strongly informed by one’s own waking-world relationship (or lack thereof) with same. Even in Freud’s own psychoanalysis, the “mother” for the sake of such analysis was the person who nurtured, and the “father” was the person who drew the nurturer’s attention away, so they could be switched gender roles, or even different people entirely than one’s parents.
The only real way to know what, if anything, your dreams are trying to tell you, is to ask yourself. You can do that…
- by reflection and personal interrogation (see for example: The Easiest Way To Take Up Journaling)
- or by externalising parts of your subconscious (as in Internal Family Systems therapy)
- or by talking directly to your subconscious where it is, by means of lucid dreaming.
The idea with lucid dreaming is that since any dream character is a facet of your subconscious generated by your own mind, by talking to that character you can ask questions directly of your subconscious (the popular 2010 movie “Inception” was actually quite accurate in this regard, by the way).
To read more about how to do this kind of self-therapy through lucid dreaming, you might want to check out this book we reviewed previously; it is the go-to book of lucid dreaming enthusiasts, and will honestly give you everything you need in one go:
Lucid Dreaming: A Concise Guide to Awakening in Your Dreams and in Your Life – by Dr. Stephen LaBerge
The Bottom-Up Model (Neuroscientists)
This will take a lot less writing, because it’s practically a null hypothesis (i.e., the simplest default assumption before considering any additional evidence that might support or refute it; usually some variant of “nothing unusual going on here”).
The Bottom-Up model holds that our brains run regular maintenance cycles during REM sleep (a biological equivalent of defragging a computer), and the brain interprets these pieces of information flying by and, because of the mind’s tendency to look for patterns, fills in the rest (much like how modern generative AI can “expand” a source image to create more of the same and fill in the blanks), resulting in the often narratively wacky, but ultimately random, vivid hallucinations that we call dreams.
The Hybrid Model (per Cartwright, 2012)
This is really just one woman’s vision, but it’s an incredibly compelling one, that takes the Bottom-Up model and asks “what if we did all that bio-stuff, and then our subconscious mind influenced the interpretation of the random patterns, to create dreams that are subjectively meaningful, and thus do indeed represent our subconscious?
It’s best explained in her own words, though, so it’s time for another book recommendation (we’ve reviewed this one before, too):
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:

Life After Death? (Your Life; A Loved One’s Death)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Show Must Go On
We’ve previously written about the topics of death and dying. It’s not cheery, but it is important to tackle.
Sooner is better than later, in the case of:
Preparations For Managing Your Own Mortality
And for those who are left behind, of course it is hardest of all:
What Grief Does To Your Body (And How To Manage It)
But what about what comes next? For those who are left behind, that is.
Life goes on
In cases when the death is that of a close loved one, the early days after death can seem like a surreal blur. How can the world go ticking on as normal when [loved one] is dead?
But incontrovertibly, it does, so we can only ask again: how?
And, we get to choose that, to a degree. The above-linked article about grief gives a “101” rundown, but it’s (by necessity, for space) a scant preparation for one of the biggest challenges in life that most of us will ever face.
For many people, processing grief involves a kind of “saying goodbye”. For others, it doesn’t, as in the following cases of grieving the loss of one’s child—something no parent should ever have to face, but it happens:
Dr. Ken Druck | The Love That Never Dies
(with warning, the above article is a little heavy)
In short: for those who choose not to “say goodbye” in the case of the death of a loved one, it’s more often not a case of cold neglect, but rather the opposite—a holding on. Not in the “denial” sense of holding on, but rather in the sense of “I am not letting go of this feeling of love, no matter how much it might hurt to hold onto; it’s all I have”.
What about widows, and love after death?
Note: we’ll use the feminine “widow” here as a) it’s the most common and b) most scientific literature focuses on widows, but there is no reason why most of the same things won’t also apply to widowers.
We say “most”, as society does tend to treat widows and widowers differently, having different expectations about a respectful mourning period, one’s comportment during same, and so on.
As an aside: most scientific literature also assumes heterosexuality, which is again statistically reasonable, and for the mostpart the main difference is any extra challenges presented by non-recognition of marriages, and/or homophobic in-laws. But otherwise, grief is grief, and as the saying goes, love is love.
One last specificity before we get into the meat of this: we are generally assuming marriages to be monogamous here. Polyamorous arrangements will likely sidestep most of these issues completely, but again, they’re not the norm.
Firstly, there’s a big difference between remarrying (or similar) after being widowed, and remarrying (or similar) after a divorce, and that largely lies in the difference of how they begin. A divorce is (however stressful it may often be) more often seen as a transition into a new period of freedom, whereas bereavement is almost always felt as a terrible loss.
The science, by the way, shows the stats for this; people are less likely to remarry, and slower to remarry if they do, in instances of bereavement rather than divorce, for example:
Timing of Remarriage Among Divorced and Widowed Parents
Love after death: the options
For widows, then, there seem to be multiple options:
- Hold on to the feelings for one’s deceased partner; never remarry
- Grieve, move on, find new love, relegating the old to history
- Try to balance the two (this is tricky but can be done*)
*Why is balancing the two tricky, and how can it be done?
It’s tricky because ultimately there are three people’s wishes at hand:
- The deceased (“they would want me to be happy” vs “I feel I would be betraying them”—which two feelings can also absolutely come together, by the way)
- Yourself (whether you actually want to get a new partner, or just remain single—this is your 100% your choice either way, and your decision should be made consciously)
- The new love (how comfortable are they with your continued feelings for your late love, really?)
And obviously only two of the above can be polled for opinions, and the latter one might say what they think we want to hear, only to secretly and/or later resent it.
One piece of solid advice for the happily married: talk with your partner now about how you each would feel about the other potentially remarrying in the event of your death. Do they have your pre-emptive blessing to do whatever, do you ask a respectable mourning period first (how long?), would the thought just plain make you jealous? Be honest, and bid your partner be honest too.
One piece of solid advice for everyone: make sure you, and your partner(s), as applicable, have a good emotional safety net, if you can. Close friends or family members that you genuinely completely trust to be there through thick and thin, to hold your/their hand through the emotional wreck that will likely follow.
Because, while depression and social loneliness are expected and looked out for, it’s emotional loneliness that actually hits the hardest, for most people:
Longitudinal Examination of Emotional Functioning in Older Adults After Spousal Bereavement
…which means that having even just one close friend or family member with whom one can be at one’s absolute worst, express emotions without censure, not have to put on the socially expected appearance of emotional stability… Having that one person (ideally more, but having at least one is critical) can make a huge difference.
But what if a person has nobody?
That’s definitely a hard place to be, but here’s a good starting point:
How To Beat Loneliness & Isolation
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: