How I Cured My Silent Reflux – by Don Daniels
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Acid reflux, in its various forms (not all of which include heartburn as a symptom!), affects around 1 in 8 people. Often it takes the form of coughing or excess mucus after eating, and it can trigger ostensibly random sweats, for example.
Don Daniels does an excellent job of demystifying the various kinds of acid reflux, explaining clearly and simply the mechanics of what is going on for each of them and why.
Further, he talks about the medications that can make things worse (and how and why), and supplements that can make it better (and supplements that can make it worse, too!), and a multiphase plan (diet on, meds weaned off, supplements on, supplements weaned off when asymptomatic, diet adjust to a new normal) to get free from acid reflux.
The writing style is simple, clear, and jargon-free, while referencing plenty of scientific literature, often quoting from it and providing sources, much like we often do at 10almonds. There are 50+ such references in all, for a 105-page book.
So, do also note that yes, it’s quite a short book for the price, but the content is of value and wouldn’t have benefitted from padding of the kind that many authors do just to make the book longer.
Bottom line: if you have, or suspect you may have, an acid reflux condition of any kind, then this book can guide you through fixing that.
Click here to check out How I Cured My Silent Reflux, and put up with it no longer!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
SuperLife – by Darin Olien
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We mostly know more or less what we’re supposed to be doing, at least to a basic level, when it comes to diet and exercise. So why don’t we do it?
Where Darin Olien excels in this one is making healthy living—mostly the dietary aspects thereof—not just simple, but also easy.
He gives principles we can apply rather than having to memorize lots of information… And his “this will generally be better than that” format also means that the feeling is one of reducing harm, increasing benefits, without needing to get absolutist about anything. And that, too, makes healthy living easier.
The book also covers some areas that a lot of books of this genre don’t—such as blood oxygenation, and maintenance of healthy pH levels—and aspects such as those are elements that help this book to stand out too.
Don’t be put off and think this is a dry science textbook, though—it’s not. In fact, the tone is light and the style is easy-reading throughout.
Bottom line: if you want to take an easy, casual, but scientifically robust approach to tweaking your health for the better, this book will enable you to do that.
Click here to check out SuperLife and start upgrading your health!
Share This Post
-
Vegan Eager for Milk Alternatives
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Q: Thanks for the info about dairy. As a vegan, I look forward to a future comment about milk alternatives
Thanks for bringing it up! What we research and write about is heavily driven by subscriber feedback, so notes like this really help us know there’s an audience for a given topic!
We’ll do a main feature on it, to do it justice. Watch out for Research Review Monday!
Share This Post
-
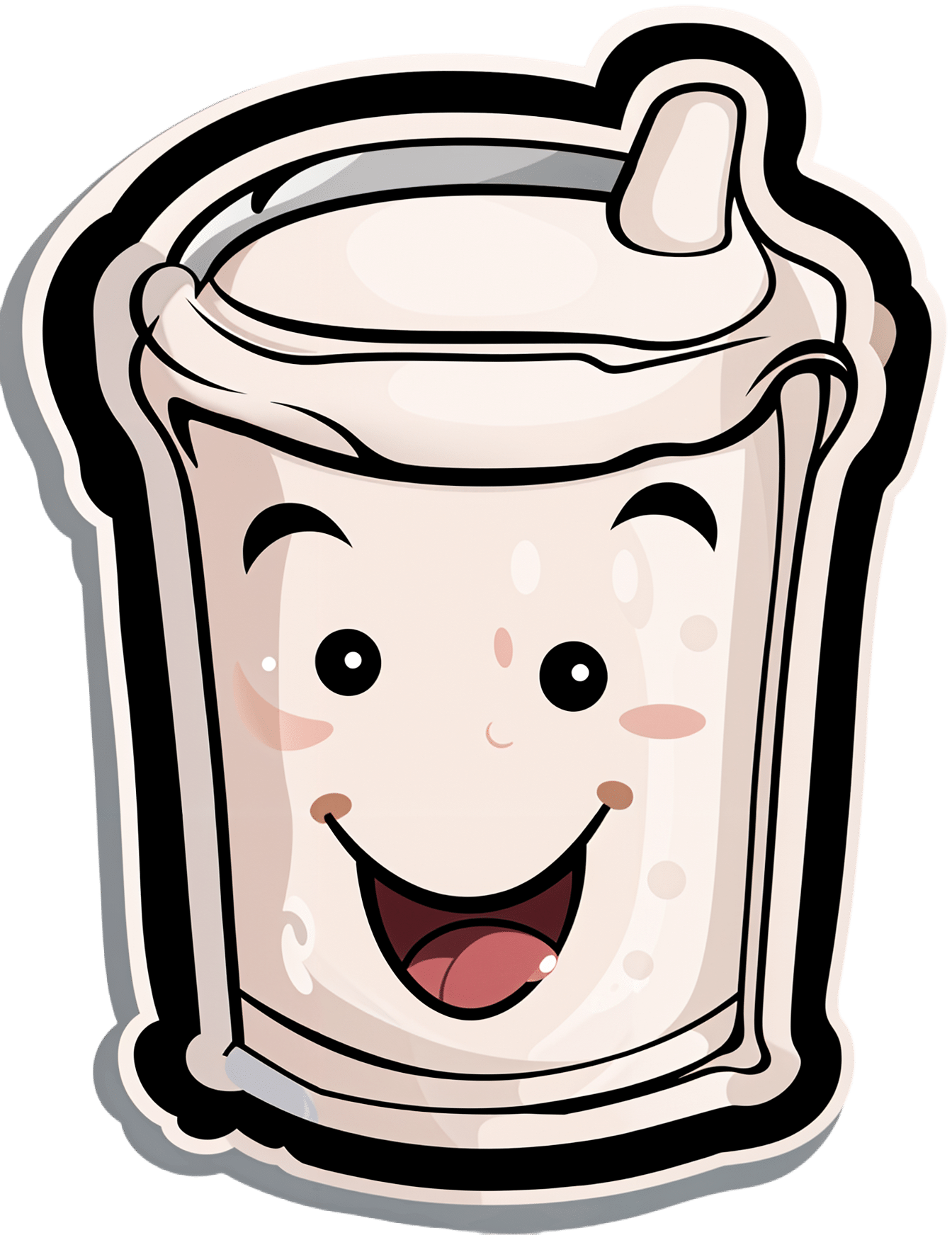
Cauliflower vs Carrot – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing cauliflower to carrot, we picked the cauliflower.
Why?
In terms of macros, cauliflower has nearly 2x the protein while carrot has nearly 2x the carbs and slightly more fiber; we’re calling it a tie in this category.
When it comes to vitamins, cauliflower has more of vitamins B2, B5, B6, B9, C, K, and choline, while carrot has more of vitamins A, B1, B3, and E. Thus, a 7:4 win for cauliflower here.
In the category of minerals, cauliflower has more iron, magnesium, manganese, phosphorus, selenium, and zinc, while carrot has more calcium, copper, and potassium. So, a 6:3 win for cauliflower here.
In short, for overall nutritional density, adding up the sections makes for a clear win for cauliflower, but of course, enjoy either or (preferably) both; diversity is good!
Want to learn more?
You might like to read:
What’s Your Plant Diversity Score?
Take care!
Share This Post
Related Posts
-
The Inflammation Spectrum – by Dr. Will Cole
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve previously reviewed Dr. Cole’s other book “Gut Feelings”, and now he’s back, this time to tackle inflammation.
The focus here is on understanding what things trigger inflammation in your body—personally yours, not someone else’s—by something close to the usual elimination process yes, but he offers a way of sliding into it gently instead of simply quitting all the things and gradually adding everything back in.
The next step he takes the reader through is eating not just to avoid triggering inflammation, but to actively combat it. From there, it should be possible for the reader to build an anti-inflammatory cookbook, that’s not only one’s own personal repertoire of cooking, but also specifically tailored to one’s own personal responses to different ingredients.
The style of this book is very pop-science, helpful, walking-the-reader-by-the-hand through the processes involved. Dr. Cole wants to make everything as easy as possible.
Bottom line: if your diet could use an anti-inflammatory revamp, this is a top-tier guidebook for doing just that.
Click here to check out The Inflammation Spectrum, find your food triggers and reset your system!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Studies of Parkinson’s disease have long overlooked Pacific populations – our work shows why that must change
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
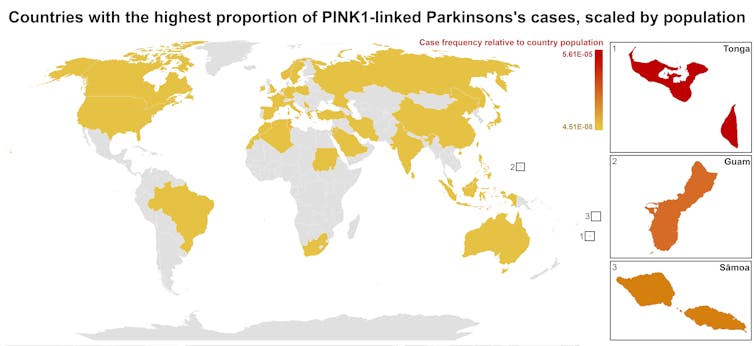
A form of Parkinson’s disease caused by mutations in a gene known as PINK1 has long been labelled rare. But our research shows it’s anything but – at least for some populations.
Our meta-analysis revealed that people in specific Polynesian communities have a much higher rate of PINK1-linked Parkinson’s than expected. This finding reshapes not only our understanding of who is most at risk, but also how soon symptoms may appear and what that might mean for treatment and testing.
Parkinson’s disease is often thought of as a single condition. In reality, it is better understood as a group of syndromes caused by different factors – genetic, environmental or a combination of both.
These varying causes lead to differences in disease patterns, progression and subsequent diagnosis. Recognising this distinction is crucial as it paves the way for targeted interventions and may even help prevent the disease altogether.
Shutterstock/sfam_photo Why we focus on PINK1-linked Parkinson’s
We became interested in this gene after a 2021 study highlighted five people of Samoan and Tongan descent living in New Zealand who shared the same PINK1 mutation.
Previously, this mutation had been spotted only in a few more distant places –Malaysia, Guam and the Philippines. The fact it appeared in people from Samoan and Tongan backgrounds suggested a historical connection dating back to early Polynesian migrations.
One person in 1,300 West Polynesians carries this mutation. This is a frequency well above what scientists usually classify as rare (below one in 2,200). This discovery means we may be overlooking entire communities in Parkinson’s research if we continue to assume PINK1-linked cases are uncommon.
This world map shows people in some Polynesian communities have a much higher rate of PINK1-linked Parkinson’s than the global population. Eden Yin, CC BY-SA Traditional understanding says PINK1-linked Parkinson’s is both rare and typically strikes younger people, mostly in their 30s or 40s, if they inherit two faulty copies of the gene. In other words, it’s considered a recessive condition, needing two matching puzzle pieces before the disease can unfold.
Our work challenges this view. We show that even one defective PINK1 gene can cause Parkinson’s at an average age of 43, much earlier than the typical onset after 65. That’s a significant departure from the standard belief that only people with two defective gene copies are at risk.
Why this matters for people with the disease
It’s not just genetics that challenge long-held views. Historically, PINK1-linked Parkinson’s was thought to lack some of the classic features of the disease, such as toxic clumps of alpha-synuclein protein.
In typical Parkinson’s, alpha-synuclein builds up in the brain, forming sticky clumps known as Lewy bodies. Our results, contrary to prior beliefs, show that alpha-synuclein pathology is present in 87.5% of PINK1 cases. This finding opens up a promising new avenue for future treatment development.
The biggest concern is early onset. PINK1-linked Parkinson’s can begin as early as 11 years old, although a more common starting point is around the mid-30s. This early onset means living longer with the disease, which can profoundly affect education, work opportunities and family life.
Current treatments (such as levodopa, a precursor of dopamine) help manage symptoms, but they’re not designed to address the root cause. If we know someone has a PINK1 mutation, scientists and clinicians can explore therapies for specific genetic pathways, potentially delivering relief beyond symptom management.
Sex differences add a layer of complexity
In Parkinson’s, generally, men are at higher risk and tend to develop symptoms earlier. However, our findings suggest the opposite pattern for PINK1-linked cases. Particularly, women with two defective copies of the gene experience onset earlier than men.
This highlights the need to consider sex-related factors in Parkinson’s research. Overlooking them risks missing key elements of the disease.
Genetic testing could be a game-changer for PINK1-linked Parkinson’s. Because it often appears earlier, doctors may not recognise it immediately, especially if they are more familiar with the common, later-onset form of Parkinson’s.
Early genetic testing could lead to a faster, more accurate diagnosis, allowing treatment to begin when interventions are most effective. It would help families understand how the disease is inherited, enabling relatives to get tested.
In some cases, where appropriate and culturally acceptable, embryo screening may be considered to prevent the passing of the faulty gene.
Knowing you have a PINK1 mutation could also make finding the right treatment more efficient. Instead of a lengthy trial-and-error process with different medications, doctors could use emerging therapies designed to target the underlying PINK1 mutation rather than relying on general Parkinson’s treatments meant for the broader population.
Addressing research gaps
These findings underscore how crucial it is to include diverse populations in health research.
Many communities, such as those in Samoa, Tonga and other Pacific nations, have had little to no involvement in global Parkinson’s genetics studies. This has created gaps in knowledge and real-world consequences for people who may not receive timely or accurate diagnoses.
Researchers, funding bodies and policymakers must prioritise projects beyond the usual focus on European or industrialised countries to ensure research findings and treatments are relevant to all affected populations.
To better diagnose and treat Parkinson’s, we need a more inclusive approach. Recognising that PINK1-linked Parkinson’s is not as rare as previously thought – and that genetics, sex differences and cultural factors all play a role – allows us to improve care for everyone.
By expanding genetic testing, refining treatments and ensuring research reflects the full spectrum of Parkinson’s, we can move closer to more precise diagnoses, targeted therapies and better support systems for all.
Victor Dieriks, Research Fellow in Health Sciences, University of Auckland, Waipapa Taumata Rau and Eden Paige Yin, PhD candidate in Health Sciences, University of Auckland, Waipapa Taumata Rau
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Avocado vs Goji Berries – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing avocado to goji berries, we picked the avocado.
Why?
It takes a special non-dried food to beat a dried food for nutritional density, but avocado manages it!
In terms of macros, avocados have more (famously health) fat; mostly monounsaturated with some polyunsaturated and a little bit of saturated, with some omega-3 and omega-6, in a healthy ratio. Meanwhile, goji berries have more fiber, carbs, and protein. As for glycemic indices, avocados are low GI (40), but goji berries are zero-GI, or, functionally, a negative glycemic index as (notwithstanding their sugar content!) they have an overall lowering effect on blood sugars. In short, both of these fruits have very different things to offer in the macros category, so we’re declaring this round a tie.
In the category of vitamins, avocados have more of vitamins A, B1, B2, B3, B5, B6, B7, B9, E, K, and choline, while goji berries have more vitamin C. A clear win for avocados!
When it comes to minerals, avocados have more copper, magnesium, manganese, phosphorus, potassium, selenium, and zinc, while goji berries have more calcium and iron. Another win for avocados!
In short, enjoy either or both (diversity is good), but for overall nutritional density, avocados win this superfood showdown today.
Want to learn more?
You might like to read:
What’s Your Plant Diversity Score?
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: