How does cancer spread to other parts of the body?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
All cancers begin in a single organ or tissue, such as the lungs or skin. When these cancers are confined in their original organ or tissue, they are generally more treatable.
But a cancer that spreads is much more dangerous, as the organs it spreads to may be vital organs. A skin cancer, for example, might spread to the brain.
This new growth makes the cancer much more challenging to treat, as it can be difficult to find all the new tumours. If a cancer can invade different organs or tissues, it can quickly become lethal.
When cancer spreads in this way, it’s called metastasis. Metastasis is responsible for the majority (67%) of cancer deaths.
Cells are supposed to stick to surrounding tissue
Our bodies are made up of trillions of tiny cells. To keep us healthy, our bodies are constantly replacing old or damaged cells.
Each cell has a specific job and a set of instructions (DNA) that tells it what to do. However, sometimes DNA can get damaged.
This damage might change the instructions. A cell might now multiply uncontrollably, or lose a property known as adherence. This refers to how sticky a cell is, and how well it can cling to other surrounding cells and stay where it’s supposed to be.
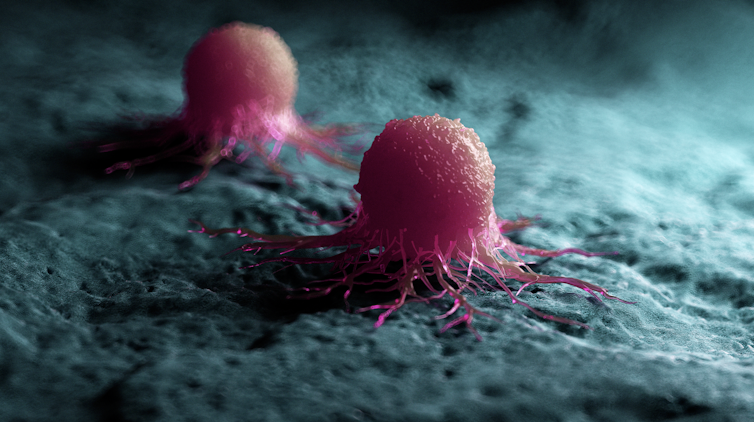
If a cancer cell loses its adherence, it can break off from the original tumour and travel through the bloodstream or lymphatic system to almost anywhere. This is how metastasis happens.
Many of these travelling cancer cells will die, but some will settle in a new location and begin to form new cancers.
Scipro/Shutterstock
Particular cancers are more likely to metastasise to particular organs that help support their growth. Breast cancers commonly metastasise to the bones, liver, and lungs, while skin cancers like melanomas are more likely to end up in the brain and heart.
Unlike cancers which form in solid organs or tissues, blood cancers like leukaemia already move freely through the bloodstream, but can escape to settle in other organs like the liver or brain.
When do cancers metastasise?
The longer a cancer grows, the more likely it is to metastasise. If not caught early, a patient’s cancer may have metastasised even before it’s initially diagnosed.
Metastasis can also occur after cancer treatment. This happens when cancer cells are dormant during treatment – drugs may not “see” those cells. These invisible cells can remain hidden in the body, only to wake up and begin growing into a new cancer months or even years later.
For patients who already have cancer metastases at diagnosis, identifying the location of the original tumour – called the “primary site” – is important. A cancer that began in the breast but has spread to the liver will probably still behave like a breast cancer, and so will respond best to an anti-breast cancer therapy, and not anti-liver cancer therapy.
As metastases can sometimes grow faster than the original tumour, it’s not always easy to tell which tumour came first. These cancers are called “cancers of unknown primary” and are the 11th most commonly diagnosed cancers in Australia.
One way to improve the treatment of metastatic cancer is to improve our ways of detecting and identifying cancers, to ensure patients receive the most effective drugs for their cancer type.
What increases the chances of metastasis and how can it be prevented?
If left untreated, most cancers will eventually acquire the ability to metastasise.
While there are currently no interventions that specifically prevent metastasis, cancer patients who have their tumours surgically removed may also be given chemotherapy (or other drugs) to try and weed out any hidden cancer cells still floating around.
The best way to prevent metastasis is to diagnose and treat cancers early. Cancer screening initiatives such as Australia’s cervical, bowel, and breast cancer screening programs are excellent ways to detect cancers early and reduce the chances of metastasis.

Peakstock/Shutterstock
New screening programs to detect cancers early are being researched for many types of cancer. Some of these are simple: CT scans of the body to look for any potential tumours, such as in England’s new lung cancer screening program.
Using artificial intelligence (AI) to help examine patient scans is also possible, which might identify new patterns that suggest a cancer is present, and improve cancer detection from these programs.
More advanced screening methods are also in development. The United States government’s Cancer Moonshot program is currently funding research into blood tests that could detect many types of cancer at early stages.
One day there might even be a RAT-type test for cancer, like there is for COVID.
Will we be able to prevent metastasis in the future?
Understanding how metastasis occurs allows us to figure out new ways to prevent it. One idea is to target dormant cancer cells and prevent them from waking up.
Directly preventing metastasis with drugs is not yet possible. But there is hope that as research efforts continue to improve cancer therapies, they will also be more effective at treating metastatic cancers.
For now, early detection is the best way to ensure a patient can beat their cancer.
Sarah Diepstraten, Senior Research Officer, Blood Cells and Blood Cancer Division, Walter and Eliza Hall Institute and John (Eddie) La Marca, Senior Resarch Officer, Walter and Eliza Hall Institute
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
What Your Mucus Says About Your Health
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s not a sexy topic (unless perhaps you have a fetish), but it is a useful topic to know about.
So, let’s get down to business with this much-maligned bodily fluid:
What is mucus? And why?
Sometimes, it can seem that mucus only exists to be an inconvenience, and to convey disease.
And… Actually, that’s mostly true.
While some kinds of mucus have other jobs beyond the scope of today’s article (did you know semen is mostly mucus? If not, now you do), the primary job of most of our mucus is to stop things (especially pathogens) going where they shouldn’t.
So, in essence, it really does exist to be an inconvenience—to pathogens. And to convey those pathogens to where they can be disposed of safely, either outside of the body, or to be an easy meal (what with being stuck in mucus, and thus at least moderately immobilized) for our various active immune cells. To make matters worse for the pathogens, there are (usually) enzymes in our mucus that have antimicrobial properties, too.
Some of mucus’s protective role can be in other ways too, such as by lining our stomach. You know, the stomach that contains the acid that can dissolve meat, despite us also being made of meat.
The slimiest rainbow
Ok, maybe not the slimiest rainbow—there’s probably a YouTube slime channel producing more colors. But, our noses are capable of dispensing astonishing quantities of mucus sometimes, and the color can vary widely, so here’s what we can know from that:
Clear
This is as it should be, in good health. If you’re getting lots of it but it’s clear, then it’s usually allergies, but watch out in case it changes color, heralding an infection. This “clear is how it looks when in ideal health”, by the way, is why when someone is sobbing in abject grief, any mucus that shows up to add to that picture will generally be clear.
White
As above, but now inflamed. Inflammation is usually something we don’t want, but in the case of a threat from a pathogen, we actually do want acute inflammation like this—the body is assembling its armies, of which, the most visible (when they appear in mass) are white blood cells. Because of their abundant presence at this stage, the mucus will also become thicker.
Yellow
As above, but the battle is now truly underway, and the yellow color comes from dead white blood cells. This does not, however, mean the battle is necessarily going badly—the body treats its white blood cells as very disposable fighters, and their deaths in large numbers are expected and normal when doing battle.
Green
As above, but neutrophils (a specific kind of white blood cell) have joined the party. They release an enzyme that colors the mucus green—and kills a lot of pathogens. Popular lore says that green mucus means a bacterial infection, but it’s not always so; these can be deployed against viruses too, depending on various factors beyond the scope of this article (but generally pertaining to severity). In any case, this too does not mean the battle is necessarily going badly, but it does express that your body is taking it very seriously—and you should, too.
Red
Nothing to do with infections, usually—it’s just a little blood (the red kind, this time). Usually it got into the mucus because the mucus membrane got damaged, usually due to some kind of physical trauma (e.g. very vigorous nose-blowing, poking things up the nose, etc) or sometimes if the air is very dry (then the mucus itself can dry out, and become stabby inside the nose; when more mucus is produced, it gets infused with blood from the injury).
Pink
As above, but combined with the “white” stage of infection response.
Orange
As above, but combined with the “yellow” stage of infection response.
Brown
As above, but the blood has oxidized—or, as a completely alterative possibility, it could mean you have been breathing a lot of pollutants. Smoke of various kinds (from fires, from smoking, etc) can cause this.
Black
There are various possible explanations here and all of them are bad. Get thee to a doctor. Superficial examples include:
- Fungal infection (you thought toxic black mold was bad when it was on the wall of the house, wait until it’s on the walls of your respiratory system)
- Blood, in abundance, oxidized (which begs the question of what caused that, but certainly: something wrong is not right)
- Pollutants again, but this time at absurd levels of exposure
That last one might sound very transient and self-correcting, but it’s not, and it comes with many increased short- and long-term health risks.
Want to know more?
Knowledge is power, so read up, and stay well:
- Beyond Supplements: The Real Immune-Boosters!
- The Cold Truth About Respiratory Infections
- Why Some People Get Sick More (And How To Not Be One Of Them)
Take care!
Share This Post
-
Their First Baby Came With Medical Debt. These Illinois Parents Won’t Have Another.
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
JACKSONVILLE, Ill. — Heather Crivilare was a month from her due date when she was rushed to an operating room for an emergency cesarean section.
The first-time mother, a high school teacher in rural Illinois, had developed high blood pressure, a sometimes life-threatening condition in pregnancy that prompted doctors to hospitalize her. Then Crivilare’s blood pressure spiked, and the baby’s heart rate dropped. “It was terrifying,” Crivilare said.
She gave birth to a healthy daughter. What followed, though, was another ordeal: thousands of dollars in medical debt that sent Crivilare and her husband scrambling for nearly a year to keep collectors at bay.
The Crivilares would eventually get on nine payment plans as they juggled close to $5,000 in bills.
“It really felt like a full-time job some days,” Crivilare recalled. “Getting the baby down to sleep and then getting on the phone. I’d set up one payment plan, and then a new bill would come that afternoon. And I’d have to set up another one.”
Crivilare’s pregnancy may have been more dramatic than most. But for millions of new parents, medical debt is now as much a hallmark of having children as long nights and dirty diapers.
About 12% of the 100 million U.S. adults with health care debt attribute at least some of it to pregnancy or childbirth, according to a KFF poll.
These people are more likely to report they’ve had to take on extra work, change their living situation, or make other sacrifices.
Overall, women between 18 and 35 who have had a baby in the past year and a half are twice as likely to have medical debt as women of the same age who haven’t given birth recently, other KFF research conducted for this project found.
“You feel bad for the patient because you know that they want the best for their pregnancy,” said Eilean Attwood, a Rhode Island OB-GYN who said she routinely sees pregnant women anxious about going into debt.
“So often, they may be coming to the office or the hospital with preexisting debt from school, from other financial pressures of starting adult life,” Attwood said. “They are having to make real choices, and what those real choices may entail can include the choice to not get certain services or medications or what may be needed for the care of themselves or their fetus.”
Best-Laid Plans
Crivilare and her husband, Andrew, also a teacher, anticipated some of the costs.
The young couple settled in Jacksonville, in part because the farming community less than two hours north of St. Louis was the kind of place two public school teachers could afford a house. They saved aggressively. They bought life insurance.
And before Crivilare got pregnant in 2021, they enrolled in the most robust health insurance plan they could, paying higher premiums to minimize their deductible and out-of-pocket costs.
Then, two months before their baby was due, Crivilare learned she had developed preeclampsia. Her pregnancy would no longer be routine. Crivilare was put on blood pressure medication, and doctors at the local hospital recommended bed rest at a larger medical center in Springfield, about 35 miles away.
“I remember thinking when they insisted that I ride an ambulance from Jacksonville to Springfield … ‘I’m never going to financially recover from this,’” she said. “‘But I want my baby to be OK.’”
For weeks, Crivilare remained in the hospital alone as covid protocols limited visitors. Meanwhile, doctors steadily upped her medications while monitoring the fetus. It was, she said, “the scariest month of my life.”
Fear turned to relief after her daughter, Rita, was born. The baby was small and had to spend nearly two weeks in the neonatal intensive care unit. But there were no complications. “We were incredibly lucky,” Crivilare said.
When she and Rita finally came home, a stack of medical bills awaited. One was already past due.
Crivilare rushed to set up payment plans with the hospitals in Jacksonville and Springfield, as well as the anesthesiologist, the surgeon, and the labs. Some providers demanded hundreds of dollars a month. Some settled for monthly payments of $20 or $25. Some pushed Crivilare to apply for new credit cards to pay the bills.
“It was a blur of just being on the phone constantly with all the different people collecting money,” she recalled. “That was a nightmare.”
Big Bills, Big Consequences
The Crivilares’ bills weren’t unusual. Parents with private health coverage now face on average more than $3,000 in medical bills related to a pregnancy and childbirth that aren’t covered by insurance, researchers at the University of Michigan found.
Out-of-pocket costs are even higher for families with a newborn who needs to stay in a neonatal ICU, averaging $5,000. And for 1 in 11 of these families, medical bills related to pregnancy and childbirth exceed $10,000, the researchers found.
“This forces very difficult trade-offs for families,” said Michelle Moniz, a University of Michigan OB-GYN who worked on the study. “Even though they have insurance, they still have these very high bills.”
Nationwide polls suggest millions of these families end up in debt, with sometimes devastating consequences.
About three-quarters of U.S. adults with debt related to pregnancy or childbirth have cut spending on food, clothing, or other essentials, KFF polling found.
About half have put off buying a home or delayed their own or their children’s education.
These burdens have spurred calls to limit what families must pay out-of-pocket for medical care related to pregnancy and childbirth.
In Massachusetts, state Sen. Cindy Friedman has proposed legislation to exempt all these bills from copays, deductibles, and other cost sharing. This would parallel federal rules that require health plans to cover recommended preventive services like annual physicals without cost sharing for patients. “We want … healthy children, and that starts with healthy mothers,” Friedman said. Massachusetts health insurers have warned the proposal will raise costs, but an independent state analysis estimated the bill would add only $1.24 to monthly insurance premiums.
Tough Lessons
For her part, Crivilare said she wishes new parents could catch their breath before paying down medical debt.
“No one is in the right frame of mind to deal with that when they have a new baby,” she said, noting that college graduates get such a break. “When I graduated with my college degree, it was like: ‘Hey, new adult, it’s going to take you six months to kind of figure out your life, so we’ll give you this six-month grace period before your student loans kick in and you can get a job.’”
Rita is now 2. The family scraped by on their payment plans, retiring the medical debt within a year, with help from Crivilare’s side job selling resources for teachers online.
But they are now back in debt, after Rita’s recurrent ear infections required surgery last year, leaving the family with thousands of dollars in new medical bills.
Crivilare said the stress has made her think twice about seeing a doctor, even for Rita. And, she added, she and her husband have decided their family is complete.
“It’s not for us to have another child,” she said. “I just hope that we can put some of these big bills behind us and give [Rita] the life that we want to give her.”
About This Project
“Diagnosis: Debt” is a reporting partnership between KFF Health News and NPR exploring the scale, impact, and causes of medical debt in America.
The series draws on original polling by KFF, court records, federal data on hospital finances, contracts obtained through public records requests, data on international health systems, and a yearlong investigation into the financial assistance and collection policies of more than 500 hospitals across the country.
Additional research was conducted by the Urban Institute, which analyzed credit bureau and other demographic data on poverty, race, and health status for KFF Health News to explore where medical debt is concentrated in the U.S. and what factors are associated with high debt levels.
The JPMorgan Chase Institute analyzed records from a sampling of Chase credit card holders to look at how customers’ balances may be affected by major medical expenses. And the CED Project, a Denver nonprofit, worked with KFF Health News on a survey of its clients to explore links between medical debt and housing instability.
KFF Health News journalists worked with KFF public opinion researchers to design and analyze the “KFF Health Care Debt Survey.” The survey was conducted Feb. 25 through March 20, 2022, online and via telephone, in English and Spanish, among a nationally representative sample of 2,375 U.S. adults, including 1,292 adults with current health care debt and 382 adults who had health care debt in the past five years. The margin of sampling error is plus or minus 3 percentage points for the full sample and 3 percentage points for those with current debt. For results based on subgroups, the margin of sampling error may be higher.
Reporters from KFF Health News and NPR also conducted hundreds of interviews with patients across the country; spoke with physicians, health industry leaders, consumer advocates, debt lawyers, and researchers; and reviewed scores of studies and surveys about medical debt.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Share This Post
-
New Eye Drops vs Age-Related Macular Degeneration
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve written previously on preventative interventions against age-related macular degeneration (AMD):
How To Avoid Age-Related Macular Degeneration
…and then supplemented that, to to speak, with:
Fatty Acids For The Eyes & Brain: The Good And The Bad
However, what if ADM happens anyway?
Not a dry eye in the house
Age-related macular degeneration comes in two forms, wet and dry, of which, dry is by far the most common (being 9 out of 10 of all cases of AMD).
It sounds like the sort of thing that eye drops should be in order for, but in fact, the wetness vs dryness is about what’s going on inside the macula, not what’s happening on the surface of the eye. Up until now, the only treatments available (aside from supplement regimes, which we linked just above) have been injectable drugs, which:
- are not fun (yes, the injection goes into the eyeball)
- don’t actually work very well (modest improvements in vision; significantly better than nothing though)
…and even those won’t help in the late stages.
However, a Korean research team has developed eye drops with peptides that inhibit the interactions between Toll-like receptors (TLRs) and TLR-signalling proteins, in a way that addresses part of the pathogenesis of AMD:
That’s quite a dense read though, so here’s a pop-science article that explains it more simply, but in more detail than we can here:
New eye drop treatment offers hope for dry AMD patients
This is a big improvement from the state of affairs previously, in which eye drops really couldn’t help at all:
What eye drops can treat macular degeneration? ← pop-science article from January 2023
No AMD, and/but want your eye health to be better?
Check out these:
10 Great Exercises to Improve Your Eyesight ← you can quickly see the results for yourself
Take care!
Share This Post
Related Posts
-
Support For Long COVID & Chronic Fatigue
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Long COVID and Chronic Fatigue
Getting COVID-19 can be very physically draining, so it’s no surprise that getting Long COVID can (and usually does) result in chronic fatigue.
But, what does this mean and what can we do about it?
What makes Long COVID “long”
Long COVID is generally defined as COVID-19 whose symptoms last longer than 28 days, but in reality the symptoms not only tend to last for much longer than that, but also, they can be quite distinct.
Here’s a large (3,762 participants) study of Long COVID, which looked at 203 symptoms:
Characterizing long COVID in an international cohort: 7 months of symptoms and their impact
Three symptoms stood at out as most prevalent:
- Chronic fatigue (CFS)
- Cognitive dysfunction
- Post-exertional malaise (PEM)
The latter means “the symptoms get worse following physical or mental exertion”.
CFS, Chronic Fatigue Syndrome, is also called Myalgic Encephalomyelitis (ME).
What can be done about it?
The main “thing that people do about it” is to reduce their workload to what they can do, but this is not viable for everyone. Note that work doesn’t just mean “one’s profession”, but anything that requires physical or mental energy, including:
- Childcare
- Housework
- Errand-running
- Personal hygiene/maintenance
For many, this means having to get someone else to do the things—either with support of family and friends, or by hiring help. For many who don’t have those safety nets available, this means things simply not getting done.
That seems bleak; isn’t there anything more we can do?
Doctors’ recommendations are chiefly “wait it out and hope for the best”, which is not encouraging. Some people do recover from Long COVID; for others, it so far appears it might be lifelong. We just don’t know yet.
Doctors also recommend to journal, not for the usual mental health benefits, but because that is data collection. Patients who journal about their symptoms and then discuss those symptoms with their doctors, are contributing to the “big picture” of what Long COVID and its associated ME/CFS look like.
You may notice that that’s not so much saying what doctors can do for you, so much as what you can do for doctors (and in the big picture, eventually help them help people, which might include you).
So, is there any support for individuals with Long COVID ME/CFS?
Medically, no. Not that we could find.
However! Socially, there are grassroots support networks, that may be able to offer direct assistance, or at least point individuals to useful local resources.
Grassroots initiatives include Long COVID SOS and the Patient-Led Research Collaborative.
The patient-led organization Body Politic also used to have such a group, until it shut down due to lack of funding, but they do still have a good resource list:
Click here to check out the Body Politic resource list (it has eight more specific resources)
Stay strong!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How To En-Joy Life (With Long-Term Benefits)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
New Year’s Dissolutions?
We have talked previously about:
The Science Of New Year’s Pre-Resolutions
…and here we are now at the end of the first week of January; how’s it going?
Hopefully, based on that article, it’s been going just great since December! For most people, statistically speaking, it hasn’t.
Around now is typically when many people enter the “bargaining” stage of New Year’s Resolutions, which at this point are often in serious danger of becoming New Year’s Dissolutions.
What’s important, really?
When trying to juggle potentially too many new items, it’s important to be able to decide where to focus one’s efforts in the case of needing to drop a ball or two.
First, the laziest way…
The path of least resistance
This is perhaps most people’s go-to. It, without too much thought, drops whatever feels most onerous, and continues with what seems easiest.
This is not a terrible approach, because what we enjoy, we will be more likely to continue. But it can be improved upon, while still getting that benefit.
Marie Kondo your
resolutionsvaluesInstead of throwing out the new habits that “don’t spark joy”, ask yourself:
“What brings me joy?”
…because often, the answer is something that’s a result of a thing that didn’t “spark joy” directly. Many things in life involve delayed gratification.
Let’s separate the [unwanted action] from the [wanted result] for a moment.
Rather than struggling on with something unpleasant for the hope of joy at the end of the rainbow, though, give yourself permission to improve the middle bit.
For example, if the idea of having lots of energy and good cardiovascular fitness is what prompted you to commit to those 6am runs each morning (but they’re not actually joyous in your experience), what would be more fun and still give you the same benefit?
Now that you know “having lots of energy and good CV fitness” is what sparks joy, not “getting up to run at 6am”, you can change lanes without pulling off the highway entirely.
Maybe a dance class will be more your speed, for example.
The key here is: you’ll have changed your resolution, without breaking it in any way that mattered
Want more ways to keep on track without burning out?
Who doesn’t? So, check out:
How To Keep On Keeping On… Long Term!
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How Are You, Really?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How Are You, Really? The Free NHS Health Test
We took this surprisingly incisive 10-minute test from the UK’s famous National Health Service—the test is part of the “Better Health” programme, a free-to-all (yes, even those from/in other countries) initiative aimed at keeping people healthy enough to have less need of medical attention.
As one person who took the test wrote:
❝I didn’t expect that a government initiative would have me talking about how I need to keep myself going to be there for the people I love, let alone that a rapid-pace multiple-choice test would elicit these responses and give personalized replies in turn, but here we are❞
It goes beyond covering the usual bases, in that it also looks at what’s most important to you, and why, and what might keep you from doing the things you want/need to do for your health, AND how those obstacles can be overcome.
Pretty impressive for a 10-minute test!
Is Your Health Above Average Already? Take the Free 10-minute NHS test now!
How old are you, in your heart?
Poetic answers notwithstanding (this writer sometimes feels so old, and yet also much younger than she is), there’s a biological answer here, too.
Again free for the use of all*, here’s a heart age calculator.
*It is suitable for you if you are aged 30–95, and do not have a known complicating cardiovascular disease.
It will ask you your (UK) postcode; just leave that field blank if you’re not in the UK; it’ll be fine.
How Old Are You, In Your Heart? Take the Free 10-minute NHS test now!
(Neither test requires logging into anything, and they do not ask for your email address. The tests are right there on the page, and they give the answers right there on the page, immediately)
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: