How to Prevent Dementia – by Dr. Richard Restak
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve written about this topic here, we know. But there’s a lot more we can do to be on guard against, and pre-emptively strengthen ourselves against, dementia.
The author, a neurologist, takes us on a detailed exploration of dementia in general, with a strong focus on Alzheimer’s in particular, as that accounts for more than half of all dementia cases.
But what if you can’t avoid it? It could be that with the wrong genes and some other factor(s) outside of your control, it will get you if something else doesn’t get you first.
Rather than scaremongering, Dr. Restak tackles this head-on too, and discusses how symptoms can be managed, to make the illness less anxiety-inducing, and look to maintain quality of life as much as possible.
The style of the book is… it reads a lot like an essay compilation. Good essays, then organized and arranged in a sensible order for reading, but distinct self-contained pieces. There are ten or eleven chapters (depending on how we count them), each divided into few or many sections. All this makes for:
- A very “read a bit now and a bit later and a bit the next day” book, if you like
- A feeling of a very quick pace, if you prefer to sit down and read it in one go
Either way, it’s a very informative read.
Bottom line: if you’d like to better understand the many-headed beast that is dementia, this book gives a far more comprehensive overview than we could here, and also explains the prophylactic interventions available.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How to Fall Back Asleep After Waking Up in the Middle of the Night
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Michael Bruce, the Sleep Doctor, addresses a common concern: waking up in the middle of the night and struggling to fall back asleep.
Understanding the Wake-Up
Firstly, why are we waking up during the night?
Waking up between 2 AM and 3 AM is said to be normal, and linked to your core body temperature. As your body core temperature drops, to trigger melatonin release, and then rises again, you get into a lighter stage of sleep. This lighter stage of sleep makes you more prone to waking up.
Note, there are also some medical conditions (such as sleep apnea) that can cause you to wake up during the night.
But, what can we do about it? Aside from constantly shifting sleeping position (Should I be sleeping on my back? On my left? Right?)
Avoid the Clock
The first step is to resist the urge to check the time. It’s easy to be tempted to have a look at the clock, however, doing so can increase anxiety, making it harder to fall back asleep. As Dr. Bruce says, sleep is like love—the less you chase it, the more it comes.
It may be useful to point your alarm clock (if you still have one of those) the opposite direction to your bed.
Embracing Non-Sleep Deep Rest (NSDR)
Whilst this may not help you fall back asleep, it’s worth pointing out that just lying quietly in the dark without moving still offers rejuvenation. This revujenating stage is called Non-Sleep Deep Rest (otherwise known as NSDR)
If you’re not familiar with NSDR, check out our overview of Andrew Huberman’s opinions on NSDR here.
So, you can reassure yourself that whilst you may not be asleep, you are still resting.
Keep Your Heart Rate Down
To fall back asleep, it’s best if your heart rate is below 60 bpm. So, Dr. Bruce advises avoiding void getting up unnecessarily, as moving around can elevate your heart rate.
On a similar vain, he introduces the 4-7-8 breathing technique, which is designed to lower your heart rate. The technique is simple:
- Breathe in for 4 seconds.
- Hold for 7 seconds.
- Exhale for 8 seconds.
Repeat this cycle gently to calm your body and mind.
As per any of our Video Breakdowns, we only try to capture the most important pieces of information in text; the rest can be garnered from the video itself:
Wishing you a thorough night’s rest!
Do you know any other good videos on sleep? Send them to us via email!
Share This Post
-
The Power of Hormones – by Dr. Max Nieuwdorp
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
First a quick note on the author: he’s an MD & PhD, internist, endocrinologist, and professor. He knows his stuff.
There are a lot of books with “the new science of” in the title, and they don’t often pertain to science that is actually new, and in this case, for the most part the science contained within this book is quite well-established.
A strength of this book is that it’s not talking about hormones in just one specific aspect (e.g. menopause, pregnancy, etc) but rather, in the full span of human health, across the spectra of ages and sexes—and yes, also covering hormones that are not sex hormones, so for example also demystifying the different happiness-related neurotransmitters, as well as the hormones responsible for hunger and satiety, weight loss and gain, sleep and wakefulness, etc.
Which is all very good, because there’s a lot of overlap and several hormones fall into several categories there.
Moreover, the book covers how your personal cocktail of hormones impacts how you look, feel, behave, and more—there’s a lot about chronic health issues here too, and how to use the information in this book to if not outright cure, then at least ameliorate, many conditions.
Bottom line: this is an information-dense book with a lot of details great and small; if you read this, you’ll come away with a much better understanding of hormones than you had previously!
Click here to check out The Power of Hormones, and harness that power for yourself!
Share This Post
-
We’re only using a fraction of health workers’ skills. This needs to change
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Roles of health professionals are still unfortunately often stuck in the past. That is, before the shift of education of nurses and other health professionals into universities in the 1980s. So many are still not working to their full scope of practice.
There has been some expansion of roles in recent years – including pharmacists prescribing (under limited circumstances) and administering a wider range of vaccinations.
But the recently released paper from an independent Commonwealth review on health workers’ “scope of practice” identifies the myriad of barriers preventing Australians from fully benefiting from health professionals’ skills.
These include workforce design (who does what, where and how roles interact), legislation and regulation (which often differs according to jurisdiction), and how health workers are funded and paid.
There is no simple quick fix for this type of reform. But we now have a sensible pathway to improve access to care, using all health professionals appropriately.
A new vision for general practice
I recently had a COVID booster. To do this, I logged onto my general practice’s website, answered the question about what I wanted, booked an appointment with the practice nurse that afternoon, got jabbed, was bulk-billed, sat down for a while, and then went home. Nothing remarkable at all about that.
But that interaction required a host of facilitating factors. The Victorian government regulates whether nurses can provide vaccinations, and what additional training the nurse requires. The Commonwealth government has allowed the practice to be paid by Medicare for the nurse’s work. The venture capitalist practice owner has done the sums and decided allocating a room to a practice nurse is economically rational.
The future of primary care is one involving more use of the range of health professionals, in addition to GPs.
It would be good if my general practice also had a physiotherapist, who I could see if I had back pain without seeing the GP, but there is no Medicare rebate for this. This arrangement would need both health professionals to have access to my health record. There also needs to be trust and good communication between the two when the physio might think the GP needs to be alerted to any issues.
This vision is one of integrated primary care, with health professionals working in a team. The nurse should be able to do more than vaccination and checking vital signs. Do I really need to see the GP every time I need a prescription renewed for my regular medication? This is the nub of the “scope of practice” issue.
How about pharmacists?
An integrated future is not the only future on the table. Pharmacy owners especially have argued that pharmacists should be able to practise independently of GPs, prescribing a limited range of medications and dispensing them.
This will inevitably reduce continuity of care and potentially create risks if the GP is not aware of what other medications a patient is using.
But a greater role for pharmacists has benefits for patients. It is often easier and cheaper for the patient to see a pharmacist, especially as bulk billing rates fall, and this is one of the reasons why independent pharmacist prescribing is gaining traction.
It’s often easier for a patient to see a pharmacist than a GP. PeopleImages.com – Yuri A/Shutterstock Every five years or so the government negotiates an agreement with the Pharmacy Guild, the organisation of pharmacy owners, about how much pharmacies will be paid for dispensing medications and other services. These agreements are called “Community Pharmacy Agreements”. Paying pharmacists independent prescribing may be part of the next agreement, the details of which are currently being negotiated.
GPs don’t like competition from this new source, even though there will be plenty of work around for GPs into the foreseeable future. So their organisations highlight the risks of these changes, reopening centuries old turf wars dressed up as concerns about safety and risk.
Who pays for all this?
Funding is at the heart of disputes about scope of practice. As with many policy debates, there is merit on both sides.
Clearly the government must increase its support for comprehensive general practice. Existing funding of fee-for-service medical benefits payments must be redesigned and supplemented by payments that allow practices to engage a range of other health professionals to create health-care teams.
This should be the principal direction of primary care reform, and the final report of the scope of practice review should make that clear. It must focus on the overall goal of better primary care, rather than simply the aspirations of individual health professionals, and working to a professional’s full scope of practice in a team, not a professional silo.
In parallel, governments – state and federal – must ensure all health professionals are used to their best of their abilities. It is a waste to have highly educated professionals not using their skills fully. New funding arrangements should facilitate better access to care from all appropriately qualified health professionals.
In the case of prescribing, it is possible to reconcile the aspirations of pharmacists and the concerns of GPs. New arrangements could be that pharmacists can only renew medications if they have agreements with the GP and there is good communication between them. This may be easier in rural and suburban areas, where the pharmacists are better known to the GPs.
The second issues paper points to the complexity of achieving scope of practice reforms. However, it also sets out a sensible path to improve access to care using all health professionals appropriately.
Stephen Duckett, Honorary Enterprise Professor, School of Population and Global Health, and Department of General Practice and Primary Care, The University of Melbourne
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
Which Sugars Are Healthier, And Which Are Just The Same?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
From Apples to Bees, and High-Fructose Cs
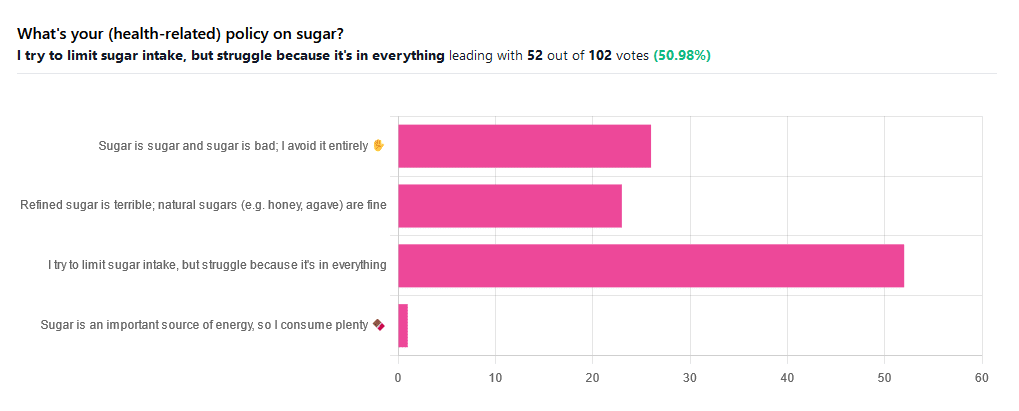
We asked you for your (health-related) policy on sugar. The trends were as follows:
- About half of all respondents voted for “I try to limit sugar intake, but struggle because it’s in everything”
- About a quarter of all respondents voted for “Refined sugar is terrible; natural sugars (e.g. honey, agave) are fine”
- About a quarter of all respondents voted for “Sugar is sugar and sugar is bad; I avoid it entirely”
- One (1) respondent voted for “Sugar is an important source of energy, so I consume plenty”
Writer’s note: I always forget to vote in these, but I’d have voted for “I try to limit sugar intake, but struggle because it’s in everything”.
Sometimes I would like to make my own [whatever] to not have the sugar, but it takes so much more time, and often money too.
So while I make most things from scratch (and typically spend about an hour cooking each day), sometimes store-bought is the regretfully practical timesaver/moneysaver (especially when it comes to condiments).
So, where does the science stand?
There has, of course, been a lot of research into the health impact of sugar.
Unfortunately, a lot of it has been funded by sugar companies, which has not helped. Conversely, there are also studies funded by other institutions with other agendas to push, and some of them will seek to make sugar out to be worse than it is.
So for today’s mythbusting overview, we’ve done our best to quality-control studies for not having financial conflicts of interest. And of course, the usual considerations of favoring high quality studies where possible Large sample sizes, good method, human subjects, that sort of thing.
Sugar is sugar and sugar is bad: True or False?
False and True, respectively.
- Sucrose is sucrose, and is generally bad.
- Fructose is fructose, and is worse.
Both ultimately get converted into glycogen (if not used immediately for energy), but for fructose, this happens mostly* in the liver, which a) taxes it b) goes very unregulated by the pancreas, causing potentially dangerous blood sugar spikes.
This has several interesting effects:
- Because fructose doesn’t directly affect insulin levels, it doesn’t cause insulin insensitivity (yay)
- Because fructose doesn’t directly affect insulin levels, this leaves hyperglycemia untreated (oh dear)
- Because fructose is metabolized by the liver and converted to glycogen which is stored there, it’s one of the main contributors to non-alcoholic fatty liver disease (at this point, we’re retracting our “yay”)
Read more: Fructose and sugar: a major mediator of non-alcoholic fatty liver disease
*”Mostly” in the liver being about 80% in the liver. The remaining 20%ish is processed by the kidneys, where it contributes to kidney stones instead. So, still not fabulous.
Fructose is very bad, so we shouldn’t eat too much fruit: True or False?
False! Fruit is really not the bad guy here. Fruit is good for you!
Fruit does contain fructose yes, but not actually that much in the grand scheme of things, and moreover, fruit contains (unless you have done something unnatural to it) plenty of fiber, which mitigates the impact of the fructose.
- A medium-sized apple (one of the most sugary fruits there is) might contain around 11g of fructose
- A tablespoon of high-fructose corn syrup can have about 27g of fructose (plus about 3g glucose)
Read more about it: Effects of high-fructose (90%) corn syrup on plasma glucose, insulin, and C-peptide in non-insulin-dependent diabetes mellitus and normal subjects
However! The fiber content (in fruit) mitigates the impact of the fructose almost entirely anyway.
And if you take fruits that are high in sugar and/but high in polyphenols, like berries, they now have a considerable net positive impact on glycemic health:
- Polyphenols and Glycemic Control
- Polyphenols and their effects on diabetes management: A review
- Dietary polyphenols as antidiabetic agents: Advances and opportunities
You may be wondering: what was that about “unless you have done something unnatural to it”?
That’s mostly about juicing. Juicing removes much (or all) of the fiber, and if you do that, you’re basically back to shooting fructose into your veins:
- Effect of Fruit Juice on Glucose Control and Insulin Sensitivity in Adults: A Meta-Analysis of 12 Randomized Controlled Trials
- Intake of Fruit, Vegetables, and Fruit Juices and Risk of Diabetes in Women
Natural sugars like honey, agave, and maple syrup, are healthier than refined sugars: True or False?
True… Sometimes, and sometimes marginally.
This is partly because of the glycemic index and glycemic load. The glycemic index scores tail off thus:
- table sugar = 65
- maple syrup = 54
- honey = 46
- agave syrup = 15
So, that’s a big difference there between agave syrup and maple syrup, for example… But it might not matter if you’re using a very small amount, which means it may have a high glycemic index but a low glycemic load.
Note, incidentally, that table sugar, sucrose, is a disaccharide, and is 50% glucose and 50% fructose.
The other more marginal health benefits come from that fact that natural sugars are usually found in foods high in other nutrients. Maple syrup is very high in manganese, for example, and also a fair source of other minerals.
But… Because of its GI, you really don’t want to be relying on it for your nutrients.
Wait, why is sugar bad again?
We’ve been covering mostly the more “mythbusting” aspects of different forms of sugar, rather than the less controversial harms it does, but let’s give at least a cursory nod to the health risks of sugar overall:
- Obesity and associated metabolic risk
- Main contributor to non-alcoholic fatty liver disease
- Increased risk of heart disease
- Insulin resistance and diabetes risk
- Cellular aging (shortened telomeres)
- 95% increased cancer risk
That last one, by the way, was a huge systematic review of 37 large longitudinal cohort studies. Results varied depending on what, specifically, was being examined (e.g. total sugar, fructose content, sugary beverages, etc), and gave up to 200% increased cancer risk in some studies on sugary beverages, but 95% increased risk is a respectable example figure to cite here, pertaining to added sugars in foods.
And finally…
The 56 Most Common Names for Sugar (Some Are Tricky)
How many did you know?
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
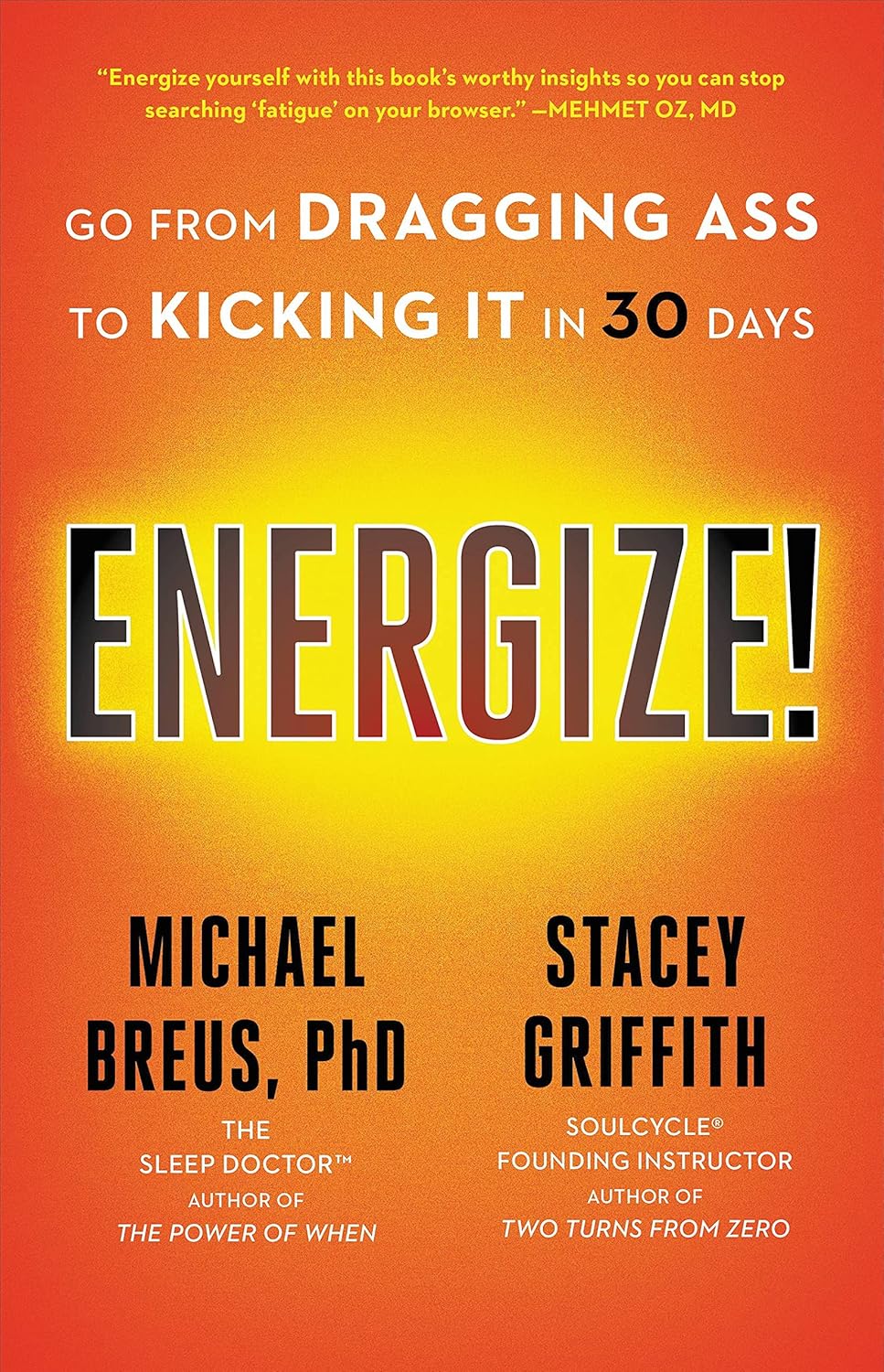
Energize! – by Dr. Michael Breus & Stacey Griffith
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We previously reviewed another book book by Dr. Breus, The Power Of When. So what’s different in this one?
While the chronotypes featured in The Power Of When also feature here (and sufficient explanation is given to make this a fine stand-alone book), this book has a lot to do with metabolism also. By considering a person’s genetically predisposed metabolic rate to be fast, medium, or slow (per being an ectomorph, mesomorph, or endomorph), and then putting that next to one’s sleep chronotype, we get 12 sub-categories that in this book each get an optimized protocol of sleep, exercise (further divided into: what kind of exercise when), and eating/fasting.
Which, in effect, amounts to a personalized coaching program for optimized energy!
The guidance is based on a combination of actual science plus “if this then that” observation-based principles—of the kind that could be described as science if they had been studied clinically instead of informally. Dr. Breus is a sleep scientist, by the way, and his co-author Stacey Griffith is a fitness coach. So between the two of them, they have sleep and exercise covered, and the fasting content is very reasonable and entirely consistent with current consensus of good practice.
The style is very pop-psychology, and very readable, and has a much more upbeat feel than The Power Of When, which seems to be because of Griffith’s presence as a co-author (most of the book is written from a neutral perspective, and some parts have first-person sections by each of the authors, so the style becomes distinct accordingly).
Bottom line: if you’d like to be more energized but [personal reason why not here] then this book may not fix all your problems, but it’ll almost certainly make a big difference and help you to stop sabotaging things and work with your body rather than against it.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
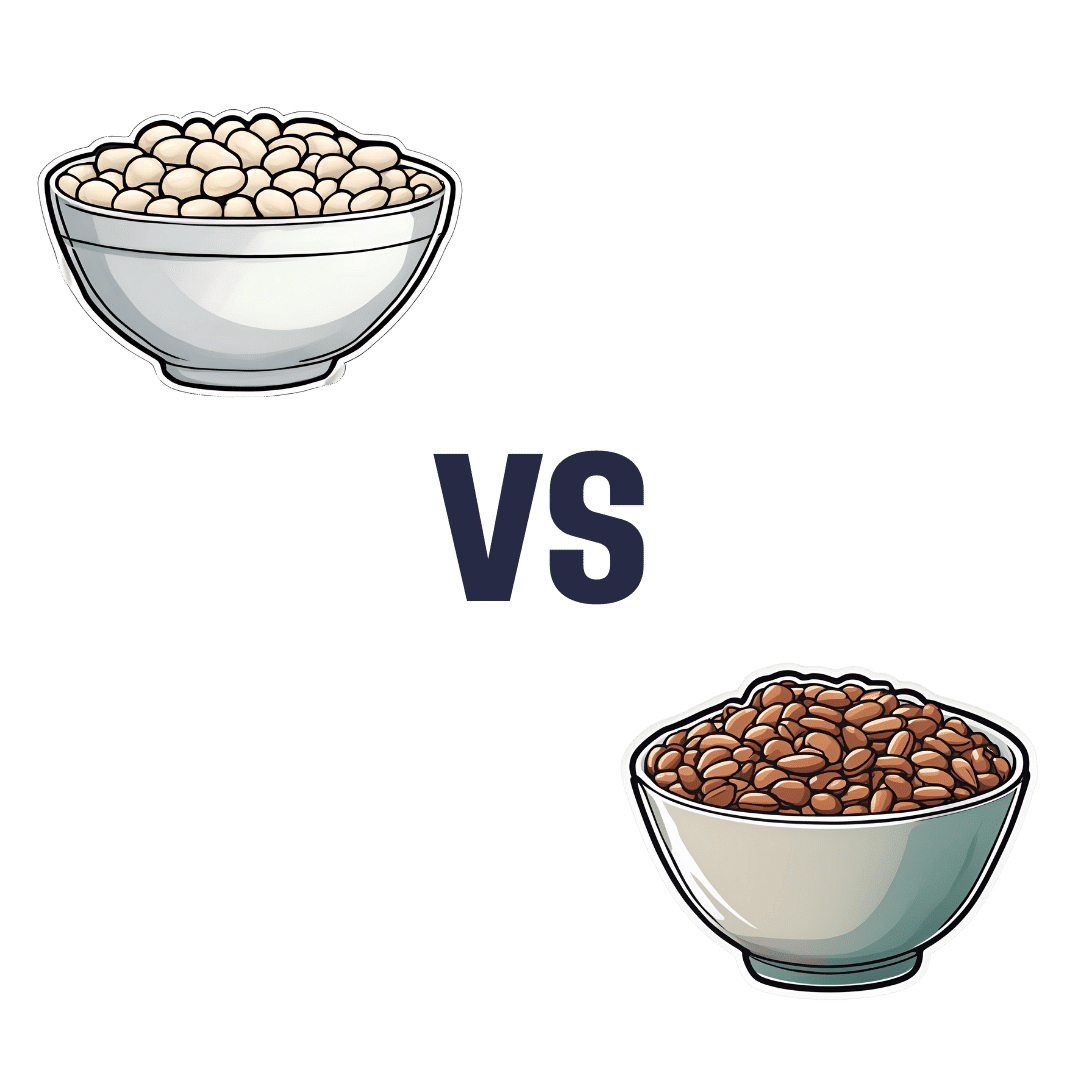
White Beans vs Pinto Beans – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing white beans to pinto beans, we picked the pinto beans.
Why?
Both are good and both have their strengths! But we say the pinto beans come out on top in total:
In terms of macros, the two beans are about equal in protein and carbs, while pinto beans have notably more fiber. White beans were already good, but we say having 1.5x the fiber makes pinto beans the winner in this category.
In the category of vitamins, white beans are not higher in any vitamins, while pinto beans have more of vitamins B1, B2, B3, B6, B7, B9, and C, making for a 7:0 win for pinto beans. It’s worth mentioning that both beans are equal in vitamins B5, E, K, and choline, though. Still, pinto beans win easily on the strength of those 7 vitamins they have more of.
When it comes to minerals, white beans have more calcium, copper, iron, magnesium, manganese, potassium, and zinc, while pinto beans have more phosphorus and selenium, making for a win for white beans this time.
Adding up the sections makes for an overall win for pinto beans, but by all means, enjoy either or both; diversity is good!
Want to learn more?
You might like to read:
What’s Your Plant Diversity Score?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: