Mammography AI Can Cost Patients Extra. Is It Worth It?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
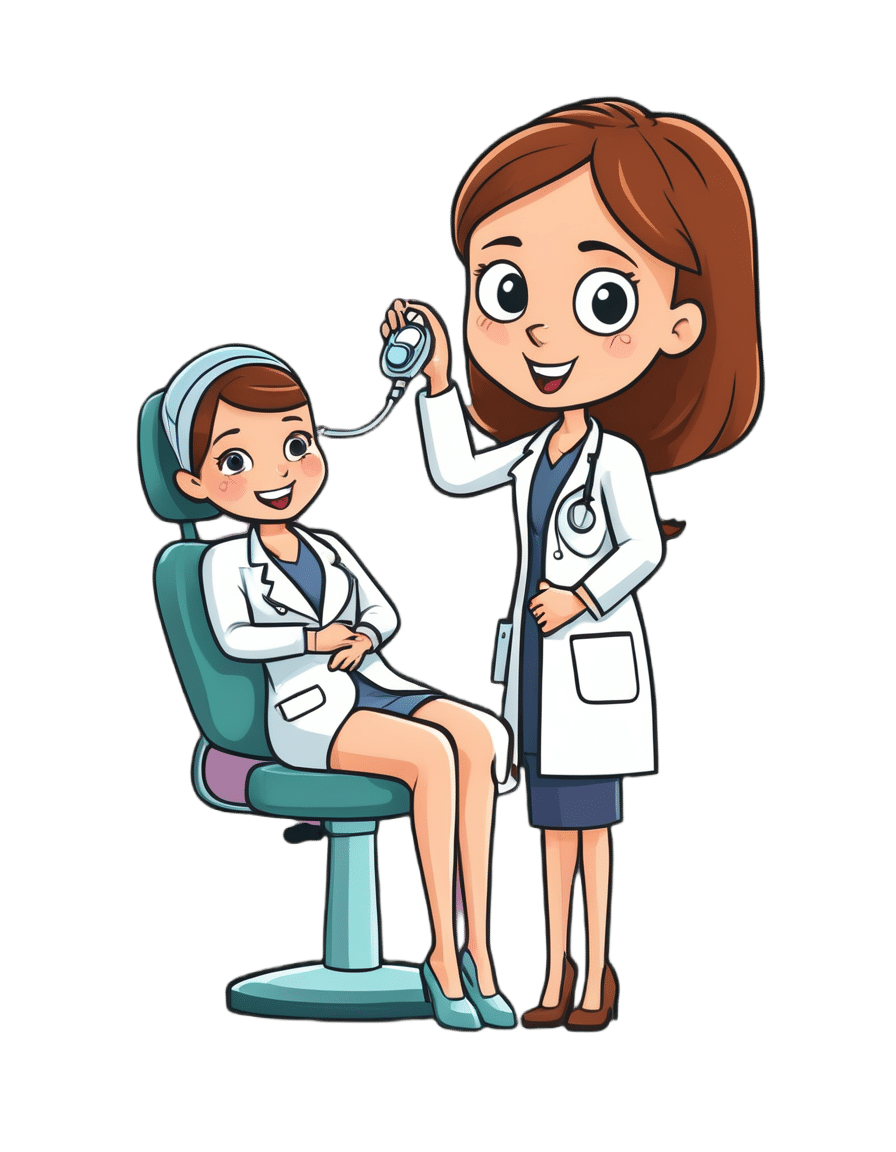
As I checked in at a Manhattan radiology clinic for my annual mammogram in November, the front desk staffer reviewing my paperwork asked an unexpected question: Would I like to spend $40 for an artificial intelligence analysis of my mammogram? It’s not covered by insurance, she added.
I had no idea how to evaluate that offer. Feeling upsold, I said no. But it got me thinking: Is this something I should add to my regular screening routine? Is my regular mammogram not accurate enough? If this AI analysis is so great, why doesn’t insurance cover it?
I’m not the only person posing such questions. The mother of a colleague had a similar experience when she went for a mammogram recently at a suburban Baltimore clinic. She was given a pink pamphlet that said: “You Deserve More. More Accuracy. More Confidence. More power with artificial intelligence behind your mammogram.” The price tag was the same: $40. She also declined.
In recent years, AI software that helps radiologists detect problems or diagnose cancer using mammography has been moving into clinical use. The software can store and evaluate large datasets of images and identify patterns and abnormalities that human radiologists might miss. It typically highlights potential problem areas in an image and assesses any likely malignancies. This extra review has enormous potential to improve the detection of suspicious breast masses and lead to earlier diagnoses of breast cancer.
While studies showing better detection rates are extremely encouraging, some radiologists say, more research and evaluation are needed before drawing conclusions about the value of the routine use of these tools in regular clinical practice.
“I see the promise and I hope it will help us,” said Etta Pisano, a radiologist who is chief research officer at the American College of Radiology, a professional group for radiologists. However, “it really is ambiguous at this point whether it will benefit an individual woman,” she said. “We do need more information.”
The radiology clinics that my colleague’s mother and I visited are both part of RadNet, a company with a network of more than 350 imaging centers around the country. RadNet introduced its AI product for mammography in New York and New Jersey last February and has since rolled it out in several other states, according to Gregory Sorensen, the company’s chief science officer.
Sorensen pointed to research the company conducted with 18 radiologists, some of whom were specialists in breast mammography and some of whom were generalists who spent less than 75% of their time reading mammograms. The doctors were asked to find the cancers in 240 images, with and without AI. Every doctor’s performance improved using AI, Sorensen said.
Among all radiologists, “not every doctor is equally good,” Sorensen said. With RadNet’s AI tool, “it’s as if all patients get the benefit of our very top performer.”
But is the tech analysis worth the extra cost to patients? There’s no easy answer.
“Some people are always going to be more anxious about their mammograms, and using AI may give them more reassurance,” said Laura Heacock, a breast imaging specialist at NYU Langone Health’s Perlmutter Cancer Center in New York. The health system has developed AI models and is testing the technology with mammograms but doesn’t yet offer it to patients, she said.
Still, Heacock said, women shouldn’t worry that they need to get an additional AI analysis if it’s offered.
“At the end of the day, you still have an expert breast imager interpreting your mammogram, and that is the standard of care,” she said.
About 1 in 8 women will be diagnosed with breast cancer during their lifetime, and regular screening mammograms are recommended to help identify cancerous tumors early. But mammograms are hardly foolproof: They miss about 20% of breast cancers, according to the National Cancer Institute.
The FDA has authorized roughly two dozen AI products to help detect and diagnose cancer from mammograms. However, there are currently no billing codes radiologists can use to charge health plans for the use of AI to interpret mammograms. Typically, the federal Centers for Medicare & Medicaid Services would introduce new billing codes and private health plans would follow their lead for payment. But that hasn’t happened in this field yet and it’s unclear when or if it will.
CMS didn’t respond to requests for comment.
Thirty-five percent of women who visit a RadNet facility for mammograms pay for the additional AI review, Sorensen said.
Radiology practices don’t handle payment for AI mammography all in the same way.
The practices affiliated with Boston-based Massachusetts General Hospital don’t charge patients for the AI analysis, said Constance Lehman, a professor of radiology at Harvard Medical School who is co-director of the Breast Imaging Research Center at Mass General.
Asking patients to pay “isn’t a model that will support equity,” Lehman said, since only patients who can afford the extra charge will get the enhanced analysis. She said she believes many radiologists would never agree to post a sign listing a charge for AI analysis because it would be off-putting to low-income patients.
Sorensen said RadNet’s goal is to stop charging patients once health plans realize the value of the screening and start paying for it.
Some large trials are underway in the United States, though much of the published research on AI and mammography to date has been done in Europe. There, the standard practice is for two radiologists to read a mammogram, whereas in the States only one radiologist typically evaluates a screening test.
Interim results from the highly regarded MASAI randomized controlled trial of 80,000 women in Sweden found that cancer detection rates were 20% higher in women whose mammograms were read by a radiologist using AI compared with women whose mammograms were read by two radiologists without any AI intervention, which is the standard of care there.
“The MASAI trial was great, but will that generalize to the U.S.? We can’t say,” Lehman said.
In addition, there is a need for “more diverse training and testing sets for AI algorithm development and refinement” across different races and ethnicities, said Christoph Lee, director of the Northwest Screening and Cancer Outcomes Research Enterprise at the University of Washington School of Medicine.
The long shadow of an earlier and largely unsuccessful type of computer-assisted mammography hangs over the adoption of newer AI tools. In the late 1980s and early 1990s, “computer-assisted detection” software promised to improve breast cancer detection. Then the studies started coming in, and the results were often far from encouraging. Using CAD at best provided no benefit, and at worst reduced the accuracy of radiologists’ interpretations, resulting in higher rates of recalls and biopsies.
“CAD was not that sophisticated,” said Robert Smith, senior vice president of early cancer detection science at the American Cancer Society. Artificial intelligence tools today are a whole different ballgame, he said. “You can train the algorithm to pick up things, or it learns on its own.”
Smith said he found it “troubling” that radiologists would charge for the AI analysis.
“There are too many women who can’t afford any out-of-pocket cost” for a mammogram, Smith said. “If we’re not going to increase the number of radiologists we use for mammograms, then these new AI tools are going to be very useful, and I don’t think we can defend charging women extra for them.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Holy Basil: What Does (And Doesn’t) It Do?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
First, a quick clarification:
- Ocimum sanctum is the botanical name given to what in English we call holy basil, and is what we will be discussing today. It’s also called “tulsi“, so if you see that name around, it is the same plant.
- Ocimum basilicum is the botanical name given to culinary basil, the kind you will find in your local supermarket. This one looks similar, but it has a different taste (culinary basil is sweeter) and a different phytochemical profile, and is certainly not the same plant.
We have touched on holy basil before, in our article:
Herbs For Evidence-Based Health & Healing
…where we listed that it helps boost immunity, per:
It’s popularly also consumed in the hopes of getting many other benefits, including:
- Calming effects on the mood (anti-stress)
- Accelerated wound-healing
- Anticancer activity
So, does it actually do those things?
Against stress
We literally couldn’t find anything. It’s often listed as being adaptogenic (reduces stress) in the preamble part of a given paper’s abstract, but we could find no study in any reputable journal that actually tested its effects against stress, and any citations for the claim just link to other papers that also include it in the preamble—and while “no original research” is a fine policy for, say, Wikipedia, it’s not a great policy when it comes to actual research science.
So… It might! There’s also no research (that we could find) showing that it doesn’t work. But one cannot claim something works on the basis of “we haven’t proved it doesn’t”.
For wound healing
Possibly! We found one (1) paper with a small (n=29) sample, and the results were promising, but that sample size of 29 was divided between three groups: a placebo control, holy basil, and another herb (which latter worked less well). So the resultant groups were tiny, arguably to the point of statistical insignificance. However, taking the study at face value and ignoring the small sample size, the results were very promising, as the holy basil group enjoyed a recovery in 4 weeks, rather than the 5 weeks recovery time of the control group:
Herbal remedies for mandibular fracture healing
An extra limitation that’s worth noting, though, is that healing bone is not necessarily the same as healing other injuries in all ways, so the same results might not be replicated in, say, organ or tissue injuries.
Against cancer
This time, there’s lots of evidence! Its mechanism of action appears to be severalfold:
- Anti-inflammatory
- Antioxidant
- Antitumor
- Chemopreventive
Because of the abundance of evidence (including specifically against skin cancer, lung cancer, breast cancer, and more), we could list studies all day here, but instead we’ll just link this one really good research review that has a handy navigation menu on the right, where you can see how it works in each of the stated ways.
Here’s the paper:
An Update on the Therapeutic Anticancer Potential of Ocimum sanctum L.: “Elixir of Life”
Want to try some?
We don’t sell it, but here for your convenience is an example product on Amazon 😎
Enjoy!
Share This Post
-
Elderberries vs Cranberries – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing elderberries to cranberries, we picked the elderberries.
Why?
In terms of macros, elderberry has slightly more carbs and 2x the fiber, the ratio of which gives elderberries the lower glycemic index also. A win for elderberries, then.
Looking at the vitamins, elderberries have more of vitamins A, B1, B2, B3, B6, B9, and C, while cranberries have more vitamin B5. An easy win for elderberries in this category.
In the category of minerals, we see a similar story: elderberries have more calcium, copper, iron, phosphorus, potassium, selenium, and zinc, while cranberries have (barely) more magnesium. Another clear win for elderberries.
Both of these fruits have additional “special” properties, and it’s worth noting that:
- elderberries’ bonus properties include that they significantly hasten recovery from upper respiratory tract viral infections.
- cranberries’ bonus properties (including: famously very good at reducing UTI risk) come with some warnings, including that they may increase the risk of kidney stones if you are prone to such, and also that cranberries have anti-clotting effects, which are great for heart health but can be a risk of you’re on blood thinners or have a bleeding disorder.
You can read about both of these fruits’ special properties in more detail below:
Want to learn more?
You might like to read:
- Herbs for Evidence-Based Health & Healing ← elderberry is in the list. We haven’t, at time of writing, done a main feature just on elderberry. Maybe soon!
- Health Benefits Of Cranberries (But: You’d Better Watch Out)
Enjoy!
Share This Post
-
Paracetamol pack sizes and availability are changing. Here’s what you need to know
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Changes are coming into effect from February 1 about how paracetamol is sold in Australia.
This mainly affects pack sizes of paracetamol sold outside pharmacies and how paracetamol is accessed in pharmacies.
The changes, announced by Australia’s drug regulator, are in line with moves internationally to reduce the harms of liver toxicity and the risk of overdose.
However, there are no new safety concerns when paracetamol is used as directed. And children’s products are not affected.
Bowonpat Sakaew/Shutterstock What is paracetamol?
Paracetamol is commonly sold under brand names such as Panadol, Dymadon and Panamax. It’s used to treat mild pain and fever for short periods or can be prescribed for chronic (long-term) pain.
Millions of packs of this cheap and accessible medicine are sold in Australia every year.
Small packs (up to 20 tablets) have been available from supermarkets and other retailers such as petrol stations. Larger packs (up to 100 tablets) are only available from pharmacies.
Paracetamol is relatively safe when used as directed. However, at higher-than-recommended doses, it can cause liver toxicity. In severe cases and when left untreated, this can be lethal.
Why are the rules changing?
In 2022, we wrote about how the Therapeutic Goods Administration (TGA) was considering changes to paracetamol access because of an increase in people going to hospital with paracetamol poisoning.
An expert review it commissioned found there were about 40–50 deaths every year from paracetamol poisoning between 2007 and 2020. Between 2009–10 and 2016–17, hospital admissions for this increased (from 8,617 to 11,697), before reducing in 2019–20 (8,723). Most admissions were due to intentional self-poisonings, and about half of these were among people aged ten to 24.
After the report, the TGA consulted with the public to work out how to prevent paracetamol poisonings.
Options included reducing pack sizes, limiting how many packs could be bought at once, moving larger packs behind the pharmacy counter and restricting access by age.
Responses were mixed. Although responses supported the need to prevent poisonings, there were concerns about how changes might affect:
- people with chronic pain, especially those in regional areas, where it may be harder to access pharmacies and, therefore, larger packs
- people on limited incomes, if certain products were made prescription-only.
Although deaths from paracetamol poisoning are tragic and preventable, they are rare considering how much paracetamol Australians use. There is less than one death due to poisoning for every million packs sold.
Because of this, it was important the TGA addressed concerns about poisonings while making sure Australians still had easy access to this essential medicine.
If you buy large packs of paracetamol for chronic pain, you’ll need to go to the pharmacy counter. StratfordProductions/Shutterstock So what’s changing?
The key changes being introduced relate to new rules about the pack sizes that can be sold outside pharmacies, and the location of products sold in pharmacies.
From February 1, packs sold in supermarkets and places other than pharmacies will reduce from a maximum 20 tablets to 16 tablets per pack. These changes bring Australia in line with other countries. These include the United Kingdom, which restricted supermarket packs to 16 tablets in 1998, and saw reductions in poisonings.
In all jurisdictions except Queensland and Western Australia, packs sold in pharmacies larger than 50 tablets will move behind the pharmacy counter and can only be sold under pharmacist supervision. In Queensland and WA, products containing more than 16 tablets will only be available from behind the pharmacy counter and sold under pharmacist supervision.
In all jurisdictions, any packs containing more than 50 tablets will need to be sold in blister packs, rather than bottles.
Several paracetamol products are not affected by these changes. These include children’s products, slow-release formulations (for example, “osteo” products), and products already behind the pharmacy counter or only available via prescription.
What else do I need to know?
These changes have been introduced to reduce the risk of poisonings from people exceeding recommended doses. The overall safety profile of paracetamol has not changed.
Paracetamol is still available from all current locations and there are no plans to make it prescription-only or remove it from supermarkets altogether. Many companies have already been updating their packaging to ensure there are no gaps in supply.
The reduction in pack sizes of paracetamol available in supermarkets means a pack of 16 tablets will now last two days instead of two-and-a-half days if taken at the maximum dose (two tablets, four times a day). Anyone in pain that does not improve after short-term use should speak to their pharmacist or GP.
For people who use paracetamol regularly for chronic pain, it is more cost-effective to continue buying larger packs from pharmacies. As larger packs (50+ tablets) need to be kept out of sight, you will need to ask at the pharmacy counter. Pharmacists know that for many people it’s appropriate to use paracetamol daily for chronic pain.
Natasa Gisev, Clinical pharmacist and Scientia Associate Professor at the National Drug and Alcohol Research Centre, UNSW Sydney and Ria Hopkins, Postdoctoral Research Fellow, National Drug and Alcohol Research Centre, UNSW Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
How To *Really* Pick Up (And Keep!) Those Habits
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Healthiest Habit-Building
Why was that book “Atomic Habits” called that? It wasn’t just because it’s a catchy title…
Habits are—much like atoms—things that are almost imperceptibly small, yet when stacked, they make up the substance of many much larger and more obvious things, and also contain an immense amount of potential power.
About that power…
Habits are the “compound interest” of natural human life. Every action we take, every decision we make, makes our life (often imperceptibly) better or worse. But getting even just 1% better or 1% worse at something every day? That’s going to not just add up over time… It’ll actively compound over time.
Habits will snowball one way or the other, good or bad. So, we want to control that snowball so that it works for us rather than against us.
Thus, we need to choose habits that are helpful to us, rather than those that are harmful to us. Top examples include:
- Making healthy food choices rather than unhealthy ones
- Moving our body regularly rather than being sedentary
- Having a good bedtime/morning routine rather than a daily chaotic blur
- Learning constantly rather than digging into old beliefs out of habit
- Forging healthy relationships rather than isolating ourselves
We all know that to make a habit stick, we need to practice it regularly, with opinions varying on how long it takes for something to become habit. Some say 21 days; some say 66. The number isn’t the important part!
What is important
You will never get to day 66, much less will you get to day 366, if you don’t first get to day 6 (New Year’s Resolutions, anyone?).
So in the early days especially, when the habit is most likely to get dropped, it’s critical to make the habit as easy as possible to form.
That means:
- The habit should be made as pleasant as possible
- (e.g. by making modifications to it if it’s not already intrinsically pleasant)
- The habit should take under 2 minutes to do at first
- (no matter if it takes longer than 2 minutes to be useful; it’ll never be useful if you don’t first get it to stick, so make your initial commitment only 2 minutes, just to get in the habit)
- The habit should have cues to remind you
- (as it’s not habit yet, you will need to either set a reminder on your phone, or leave a visual reminder, such as your workout clothes laid out ready for you in the morning, or a bowl of fruit in plain view where you spend a lot of time)
What gets measured, gets done
Streaks are a great way to do this. Habit-tracking apps help. Marks on a calendar or in a journal are also totally fine.
What can help especially, and that a lot of people don’t do, is to have a system of regular personal reviews—like a work “performance review”, but for oneself and one’s own life.
Set a reminder or write on the calendar / in your diary, to review monthly, or weekly if you prefer, such things as:
- How am I doing in the areas of life that are important to me?
- Have a list of the areas of life that are important to you, by the way, and genuinely reflect on each of them, e.g:
- Health
- Finances
- Relationships
- Learning
- Sleep
- Etc
- Have a list of the areas of life that are important to you, by the way, and genuinely reflect on each of them, e.g:
- What is working for me, and what isn’t working for me?
- What will I do better in this next month/week?
…and then do it!
Good luck, and may it all stack up in your favor!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Wandering Mind – by Dr. Michael Corballis
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our mind’s tendency to wander can be a disability, but could it also be a superpower? Dr. Corballis makes the case for such.
While many authors focus on, well, how to focus, Dr. Corballis argues in this book that our wandering imagination can be more effective at problem-solving and creative tasks, than a focused, blinkered mind.
The book’s a quick read (184 pages of quite light reading), and yet still quite dense with content. He takes us on a tour of the brain, theory of mind, the Default Mode Network (where a lot of the brain’s general ongoing organization occurs), learning, memory, forgetting, and creativity.
Furthermore, he cites (and explains) studies showing what kinds of “breaks” from mental work allow the wandering mind to do its thing at peak efficiency, and what kinds of breaks are counterproductive. Certainly this has practical applications for all of us!
Bottom line: if you’d like to be less frustrated by your mind’s tendency to wander, this is a fine book to show how to leverage that trait to your benefit.
Click here to check out The Wandering Mind, and set yours onto more useful tracks!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Blue Cheese vs Brunost – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing blue cheese to brunost, we picked the brunost.
Why?
First, for the unfamiliar, as brunost isn’t necessarily as popular as blue cheese in N. America where most of our readers are:
Brunost, literally “brown cheese” is a traditional Norwegian affair made from aggressively boiling milk, cream, and whey in an iron cauldron. Whereas the blue in blue cheese comes from mold, the brown in brown cheese comes from caramelizing the milk sugars in the cauldron. When we say “cauldron”, yes, there is nowadays mass-produced brunost that is no longer made in something that could be mistaken for a witch’s brew, but the use of cast iron is actually important to the process, and has been the subject of regulatory controversy in Norway; first the cast iron was abandoned, then because that changed the cheese they fortified the product with added iron supplementation, then that was banned, then they reversed it because it affected iron levels in the general population. Nowadays, it is usually made with iron, one way or another.
Ok, so let’s see how they stack up against each other:
In terms of macronutrients, the two cheeses are comparable in fat, but brunost has more carbs—because whereas bacteria (and to a lesser extent, the mold) ate nearly all the carbs in the blue cheese, the caramelization of the milk sugars in brunost meant the result stayed higher in carbs. Both are considered “low GI” foods, but this category is still at least a moderate win for blue cheese.
When it comes to vitamins, brunost is higher in vitamins A, B1, B2, B3, B5, B6, and B12, while blue cheese is higher in vitamin B9. In other words, a clear and easy win for brunost.
In the category of minerals, brunost has more copper, iron, magnesium, manganese, phosphorus, and potassium. Meanwhile, blue cheese contains more zinc, although we can also mention that blue cheese has about 2x the sodium, which is generally not considered a benefit. The two cheeses are about equal in calcium and selenium. Adding these up makes for another clear and easy win for brunost.
In short, unless you are strongly avoiding [even low-GI foods’] carbs for some reason, brunost wins the day by virtue of its overwhelmingly better vitamin and mineral content.
Still, like most fermented dairy products, both cheeses can be enjoyed in moderation as part of a healthy diet (assuming you don’t have an allergy/intolerance).
Want to learn more?
You might like to read:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: