Coach’s Plan – by Mike Kavanagh
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A sports coach’s job is to prepare a plan, give it to the player(s), and hold them accountable to it. Change the strategy if needs be, call the shots. The job of the player(s) is then to follow those instructions.
If you have trouble keeping yourself accountable, Kavanagh argues that it can be good to separate how you approach things.
Not just “coach yourself”, but put yourself entirely in the coach’s shoes, as though you were a separate person, then switch back, and follow those instructions, trusting in your coach’s guidance.
The book also provides illustrative examples and guides the reader through some potential pitfalls—for example, what happens when morning you doesn’t want to do the things that evening you decided would be best?
The absolute backbone of this method is that it takes away the paralysing self-doubt that can occur when we second-guess ourselves mid-task.
In short, this book will fire up your enthusiasm and give you a reliable fall-back for when your motivation’s flagging.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Big Think’s #1 Antidote To Aging
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Why This Video Is Important
A lot of what we talk about here at 10almonds is focused on healthy aging. We want you – our lovely readers – to not only live for a long time, but also be healthy enough to enjoy that “long time”.
We’ve talked about anything from Dr. Greger’s eight anti-aging interventions, to the specific benefits of resveratrol or metformin in combatting aging, to even reducing stress-induced aging.
So, why is this video important? It goes beyond just talking about what we know about living longer, but also focuses on how we should live longer; there’s a big difference between living a long life but never leaving your house vs. living a long life beyond your front door.
The Takeaways
The core message that Big Think wants to convey is that our lifestyle is our best bet in slowing the aging process. Our bodies are adaptive systems, responding positively to healthy lifestyle choices. They focus on exercise: regular physical activity increases healthspan, consequently extending lifespan.
A key takeaway is the difference between physical activity and exercise. While any movement counts as physical activity, exercise is a deliberate, health-focused activity. It benefits the brain by releasing growth factors that strengthen critical areas like the hippocampus and prefrontal cortex.
The video encourages embracing physical activity in any form available to you, from gardening to walking. The goal isn’t to hit a specific number of steps but to stay active in a way that suits your lifestyle.
Science may not solve death. Yet. But focusing on maintaining a healthy, functioning state for as long as possible is the real victory in the battle against aging. And, at the moment, exercise seems to be our best bet:
How did you find that video? If you’ve discovered any great videos yourself that you’d like to share with fellow 10almonds readers, then please do email them to us!
Share This Post
-
Your Brain on Art – by Susan Magsamen & Ivy Ross
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The notion of art therapy is popularly considered a little wishy-washy. As it turns out, however, there are thousands of studies showing its effectiveness.
Nor is this just a matter of self-expression. As authors Magsamen and Ross explore, different kinds of engagement with art can convey different benefits.
That’s one of the greatest strengths of this book: “this form of engagement with art will give these benefits, according to these studies”
With benefits ranging from reducing stress and anxiety, to overcoming psychological trauma or physical pain, there’s a lot to be said for art!
And because the book covers many kinds of art, if you can’t imagine yourself taking paintbrush to canvas, that’s fine too. We learn of the very specific cognitive benefits of coloring in mandalas (yes, really), of sculpting something terrible in clay, or even just of repainting the kitchen, and more. Each thing has its set of benefits.
The book’s main goal is to encourage the reader to cultivate what the authors call an aesthetic mindset, which involves four key attributes:
- a high level of curiosity
- a love of playful, open-ended exploration
- a keen sensory awareness
- a drive to engage in creative activities
And, that latter? It’s as a maker and/or a beholder. We learn about what we can gain just by engaging with art that someone else made, too.
Bottom line: come for the evidence-based cognitive benefits; stay for the childlike wonder of the universe. If you already love art, or have thought it’s just “not for you”, then this book is for you.
Click here to check out Your Brain On Art, and open up whole new worlds of experience!
Share This Post
-
The Power of Self-Care – by Dr. Sunil Kumar
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
First, what this book is mostly not about: bubble baths and scented candles. We say “mostly”, because stress management is an important aspect given worthy treatment in this book, but there is more emphasis on evidence-based interventions and thus Dr. Kumar is readier to prescribe nature walks and meditation, than product-based pampering sessions.
As is made clear in the subtitle “Transforming Heart Health with Lifestyle Medicine”, the focus is on heart health throughout, but as 10almonds readers know, “what’s good for your heart is good for your brain” is a truism that indeed holds true here too.
Dr. Kumar also gives nutritional tweaks to optimize heart health, and includes a selection of heart-healthy recipes, too. And exercise? Yes, customizable exercise plans, even. And a plan for getting sleep into order if perchance it has got a bit out of hand (most people get less sleep than necessary for maintenance of good health), and he even delves into “social prescribing”, that is to say, making sure that one’s social connectedness does not get neglected—without letting it, conversely, take over too much of one’s life (done badly, social connectedness can be a big source of unmanaged stress).
Perhaps the most value of this book comes from its 10-week self-care plan (again, with a focus on heart health), basically taking the reader by the hand for long enough that, after those 10 weeks, habits should be quite well-ingrained.
A strong idea throughout is that the things we take up should be sustainable, because well, a heart is for life, not just for a weekend retreat.
Bottom line: if you’d like to improve your heart health in a way that feels like self-care rather than an undue amount of work, then this is the book for you.
Share This Post
Related Posts
-
Health Care AI, Intended To Save Money, Turns Out To Require a Lot of Expensive Humans
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Preparing cancer patients for difficult decisions is an oncologist’s job. They don’t always remember to do it, however. At the University of Pennsylvania Health System, doctors are nudged to talk about a patient’s treatment and end-of-life preferences by an artificially intelligent algorithm that predicts the chances of death.
But it’s far from being a set-it-and-forget-it tool. A routine tech checkup revealed the algorithm decayed during the covid-19 pandemic, getting 7 percentage points worse at predicting who would die, according to a 2022 study.
There were likely real-life impacts. Ravi Parikh, an Emory University oncologist who was the study’s lead author, told KFF Health News the tool failed hundreds of times to prompt doctors to initiate that important discussion — possibly heading off unnecessary chemotherapy — with patients who needed it.
He believes several algorithms designed to enhance medical care weakened during the pandemic, not just the one at Penn Medicine. “Many institutions are not routinely monitoring the performance” of their products, Parikh said.
Algorithm glitches are one facet of a dilemma that computer scientists and doctors have long acknowledged but that is starting to puzzle hospital executives and researchers: Artificial intelligence systems require consistent monitoring and staffing to put in place and to keep them working well.
In essence: You need people, and more machines, to make sure the new tools don’t mess up.
“Everybody thinks that AI will help us with our access and capacity and improve care and so on,” said Nigam Shah, chief data scientist at Stanford Health Care. “All of that is nice and good, but if it increases the cost of care by 20%, is that viable?”
Government officials worry hospitals lack the resources to put these technologies through their paces. “I have looked far and wide,” FDA Commissioner Robert Califf said at a recent agency panel on AI. “I do not believe there’s a single health system, in the United States, that’s capable of validating an AI algorithm that’s put into place in a clinical care system.”
AI is already widespread in health care. Algorithms are used to predict patients’ risk of death or deterioration, to suggest diagnoses or triage patients, to record and summarize visits to save doctors work, and to approve insurance claims.
If tech evangelists are right, the technology will become ubiquitous — and profitable. The investment firm Bessemer Venture Partners has identified some 20 health-focused AI startups on track to make $10 million in revenue each in a year. The FDA has approved nearly a thousand artificially intelligent products.
Evaluating whether these products work is challenging. Evaluating whether they continue to work — or have developed the software equivalent of a blown gasket or leaky engine — is even trickier.
Take a recent study at Yale Medicine evaluating six “early warning systems,” which alert clinicians when patients are likely to deteriorate rapidly. A supercomputer ran the data for several days, said Dana Edelson, a doctor at the University of Chicago and co-founder of a company that provided one algorithm for the study. The process was fruitful, showing huge differences in performance among the six products.
It’s not easy for hospitals and providers to select the best algorithms for their needs. The average doctor doesn’t have a supercomputer sitting around, and there is no Consumer Reports for AI.
“We have no standards,” said Jesse Ehrenfeld, immediate past president of the American Medical Association. “There is nothing I can point you to today that is a standard around how you evaluate, monitor, look at the performance of a model of an algorithm, AI-enabled or not, when it’s deployed.”
Perhaps the most common AI product in doctors’ offices is called ambient documentation, a tech-enabled assistant that listens to and summarizes patient visits. Last year, investors at Rock Health tracked $353 million flowing into these documentation companies. But, Ehrenfeld said, “There is no standard right now for comparing the output of these tools.”
And that’s a problem, when even small errors can be devastating. A team at Stanford University tried using large language models — the technology underlying popular AI tools like ChatGPT — to summarize patients’ medical history. They compared the results with what a physician would write.
“Even in the best case, the models had a 35% error rate,” said Stanford’s Shah. In medicine, “when you’re writing a summary and you forget one word, like ‘fever’ — I mean, that’s a problem, right?”
Sometimes the reasons algorithms fail are fairly logical. For example, changes to underlying data can erode their effectiveness, like when hospitals switch lab providers.
Sometimes, however, the pitfalls yawn open for no apparent reason.
Sandy Aronson, a tech executive at Mass General Brigham’s personalized medicine program in Boston, said that when his team tested one application meant to help genetic counselors locate relevant literature about DNA variants, the product suffered “nondeterminism” — that is, when asked the same question multiple times in a short period, it gave different results.
Aronson is excited about the potential for large language models to summarize knowledge for overburdened genetic counselors, but “the technology needs to improve.”
If metrics and standards are sparse and errors can crop up for strange reasons, what are institutions to do? Invest lots of resources. At Stanford, Shah said, it took eight to 10 months and 115 man-hours just to audit two models for fairness and reliability.
Experts interviewed by KFF Health News floated the idea of artificial intelligence monitoring artificial intelligence, with some (human) data whiz monitoring both. All acknowledged that would require organizations to spend even more money — a tough ask given the realities of hospital budgets and the limited supply of AI tech specialists.
“It’s great to have a vision where we’re melting icebergs in order to have a model monitoring their model,” Shah said. “But is that really what I wanted? How many more people are we going to need?”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
This article first appeared on KFF Health News and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Getting COMFY – by Jordan Gross
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s easy to see how good “morning people” seem to have it; it’s harder, it seems, to become one.
And, if we’re forced by circumstance to be the morning person we’re not? We all-too-easily find ourselves greeting each coming day without the joy that, in an ideal world, we might.
So, is it possible to learn this power? Jordan Gross has it mapped out for it us…
The “COMFY” of the title is indeed an acronym, and it stands for:
- Calm
- Openness
- Movement
- Funny
- You
There’s a chapter explaining each in detail, and they’re bookended with other chapters explaining more about the whys and the hows.
As you might expect, the key to a good morning starts the night before, but there’s also a formula to follow. Of course, you can change it up, mix and match if you like… but this book provides a base framework to build from, which is something that can make a huge difference!
Bottom line: it’s a highly enjoyable book to read, and also provides genuine powerful help to bring us the brighter happier mornings we deserve—the set-up to the perfect day!
Click here to check out “Getting COMFY” and perk up your mornings—you deserve it!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Eat All You Want (But Wisely)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
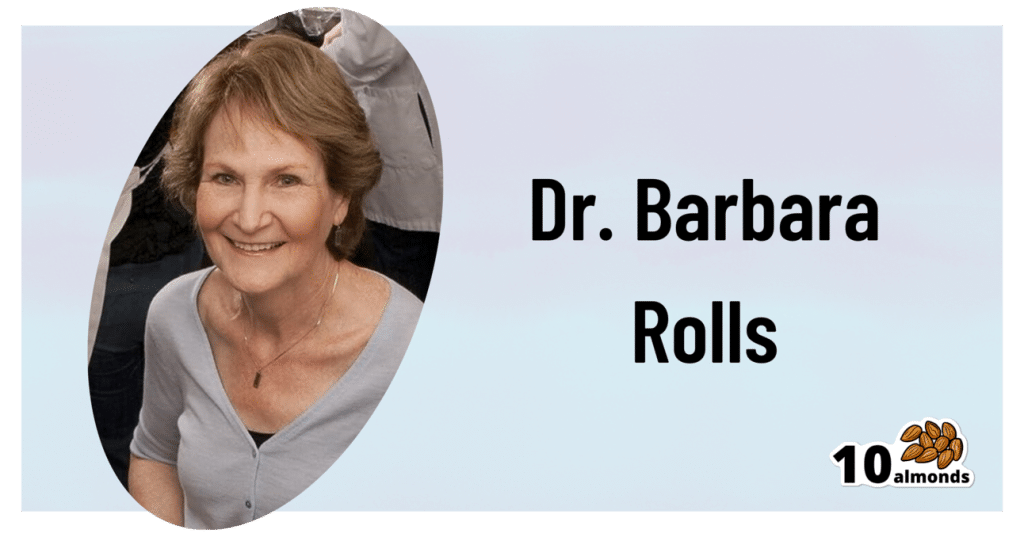
Some Surprising Truths About Hunger And Satiety
This is Dr. Barbara Rolls. She’s Professor and Guthrie Chair in Nutritional Sciences, and Director of the Laboratory for the Study of Human Ingestive Behavior at Pennsylvania State University, after graduating herself from Oxford and Cambridge (yes, both). Her “awards and honors” take up four A4 pages, so we won’t list them all here.
Most importantly, she’s an expert on hunger, satiety, and eating behavior in general.
What does she want us to know?
First and foremost: you cannot starve yourself thin, unless you literally starve yourself to death.
What this is about: any weight lost due to malnutrition (“not eating enough” is malnutrition) will always go back on once food becomes available. So unless you die first (not a great health plan), merely restricting good will always result in “yo-yo dieting”.
So, to avoid putting the weight back on and feeling miserable every day along the way… You need to eat as much as you feel you need.
But, there’s a trick here (it’s about making you genuinely feel you need less)!
Your body is an instrument—so play it
Your body is the tool you use to accomplish pretty much anything you do. It is, in large part, at your command. Then there are other parts you can’t control directly.
Dr. Rolls advises taking advantage of the fact that much of your body is a mindless machine that will simply follow instructions given.
That includes instructions like “feel hungry” or “feel full”. But how to choose those?
Volume matters
An important part of our satiety signalling is based on a physical sensation of fullness. This, by the way, is why bariatric surgery (making a stomach a small fraction of the size it was before) works. It’s not that people can’t eat more (the stomach is stretchy and can also be filled repeatedly), it’s that they don’t want to eat more because the pressure sensors around the stomach feel full, and signal the hormone leptin to tell the brain we’re full now.
Now consider:
- On the one hand, 20 grapes, fresh and bursting with flavor
- On the other hand, 20 raisins (so, dried grapes), containing the same calories
Which do you think will get the leptin flowing sooner? Of course, the fresh grapes, because of the volume.
So if you’ve ever seen those photos that show two foods side by side with the same number of calories but one is much larger (say, a small slice of pizza or a big salad), it’s not quite the cheap trick that it might have appeared.
Or rather… It is a cheap trick; it’s just a cheap trick that works because your stomach is quite a simple organ.
So, Dr. Rolls’ advice: generally speaking, go for voluminous food. Fruit is great from this, because there’s so much water. Air-popped popcorn also works great. Vegetables, too.
Water matters, but differently than you might think
A well-known trick is to drink water before and with a meal. That’s good, it’s good to be hydrated. However, it can be better. Dr. Rolls did an experiment:
The design:
❝Subjects received 1 of 3 isoenergetic (1128 kJ) preloads 17 min before lunch on 3 d and no preload on 1 d.
The preloads consisted of 1) chicken rice casserole, 2) chicken rice casserole served with a glass of water (356 g), and 3) chicken rice soup.
The soup contained the same ingredients (type and amount) as the casserole that was served with water.❞
The results:
❝Decreasing the energy density of and increasing the volume of the preload by adding water to it significantly increased fullness and reduced hunger and subsequent energy intake at lunch.
The equivalent amount of water served as a beverage with a food did not affect satiety.❞
The conclusion:
❝Consuming foods with a high water content more effectively reduced subsequent energy intake than did drinking water with food.❞
You can read the study in full (it’s a worthwhile read!) here:
Water incorporated into a food but not served with a food decreases energy intake in lean women
Protein matters
With all those fruits and vegetables and water, you may be wondering Dr. Rolls’ stance on proteins. It’s simple: protein is an appetite suppressant.
However, it takes about 20 minutes to signal the brain about that, so having some protein in a starter (if like this writer, you’re the cook of the household, a great option is to enjoy a small portion of nuts while cooking!) gets that clock ticking, to signal satiety sooner.
It may also help in other ways:
Clinical Evidence and Mechanisms of High-Protein Diet-Induced Weight Loss
As for other foods that can suppress appetite, by the way, you might like;
25 Foods That Act As Natural Appetite Suppressants
Variety matters, and in ways other than you might think
A wide variety of foods (especially: a wide variety of plants) in one’s diet is well recognized as a key to a good balanced diet.
However…
A wide variety of dishes at the table, meanwhile, promotes greater consumption of food.
Dr. Rolls did a study on this too, a while ago now (you’ll see how old it is) but the science seems robust:
Variety in a Meal Enhances Food Intake in Man
Notwithstanding the title, it wasnot about a man (that was just how scientists wrote in ye ancient times of 1981). The test subjects were, in order: rats, cats, a mixed group of men and women, the same group again, and then a different group of all women.
So, Dr. Rolls’ advice is: it’s better to have one 20-ingredient dish, than 10 dishes with 20 ingredients between them.
Sorry! We love tapas and buffets too, but that’s the science!
So, “one-pot” meals are king in this regard; even if you serve it with one side (reasonable), that’s still only two dishes, which is pretty good going.
Note that the most delicious many-ingredient stir-fries and similar dishes from around the world also fall into this category!
Want to know more?
If you have the time (it’s an hour), you can enjoy a class of hers for free:
Want to watch it, but not right now? Bookmark it for later
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: