Peace Is Every Step – by Thích Nhất Hạnh
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Mindfulness is one of the few practices to make its way from religion (in this case, Buddhism) into hard science. We’ve written before about its many evidence-based benefits, and many national health information outlets recommend it. So, what does this book have to add?
Thích Nhất Hạnh spent most of his 95 years devoted to the practice and teaching of mindfulness and compassion. In this book, the focus is on bringing mindfulness off the meditation mat and into general life.
After all, what if we could extend that “unflappability” into situations that pressure and antagonize us? That would be some superpower!
The author offers techniques to do just that, simple exercises to transform negative emotions, and to make us more likely to remember to do so.
After all, “in the heat of the moment” is rarely when many of us are at our best, this book gives way to allow those moments themselves to serve as immediate triggers to be our best.
The title “Peace Is Every Step” is not a random collection of words; the goal of this book is to enable to reader to indeed carry peace with us as we go.
Not just “peace is always available to us”, but if we do it right: “we have now arranged for our own peace to automatically step in and help us when we need it most”.
Bottom line: if you’d like to practice mindfulness, or practice it more consistently, this book offers some powerful tools.
Click here to check out Peace Is Every Step, and carry yours with you!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
From Lupus To Arthritis: New Developments
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This week’s health news round-up highlights some things that are getting better, and some things that are getting worse, and how to be on the right side of both:
New hope for lupus sufferers
Lupus is currently treated mostly with lifelong medications to suppress the immune system, which is not only inconvenient, but also can leave people more open to infectious diseases. The latest development uses CAR T-cell technology (as has been used in cancer treatment for a while) to genetically modify cells to enable the body’s own immune system to behave properly:
Read in full: Exciting new lupus treatment could end need for lifelong medication
Related: How to Prevent (Or Reduce The Severity Of) Inflammatory Diseases
It’s in the hips
There are a lot of different kinds of hip replacements, and those with either delta ceramic or oxidised zirconium head with a highly cross-linked polyethylene liner/cup have the lowest risk of need for revision in the 15 years after surgery. This is important, because obviously, once it’s in there, you want it to be able to stay in there and not have to be touched again any time soon:
Read in full: Study identifies hip implant materials with the lowest risk of needing revision
Related: Nobody Likes Surgery, But Here’s How To Make It Much Less Bad
Sooner is better than later
Often, people won’t know about an unwanted pregnancy in the first six weeks, but for those who are able to catch it early, Very Early Medical Abortion (VEMA) offers a safe an effective way of doing so, with success rate being linked to earliness of intervention:
Read in full: Very early medication abortion is effective and safe, study finds
Related: What Might A Second Trump Presidency Look Like for Health Care?
Increased infectious disease risks from cattle farms
Many serious-to-humans infectious diseases enter the human population via the animal food chain, and in this case, bird flu becoming more rampant amongst cows is starting to pose a clear threat to humans, so this is definitely something to be aware of:
Read in full: Bird flu infects 1 in 14 dairy workers exposed; CDC urges better protections
Related: With Only Gloves To Protect Them, Farmworkers Say They Tend Sick Cows Amid Bird Flu
Herald of woe
Gut health affects most of the rest of health, and there are a lot of links between gut and bone health. In this case, an association has been found between certain changes in the gut microbiome, and subsequent onset of rheumatoid arthritis:
Read in full: Changes in gut microbiome could signal onset of rheumatoid arthritis
Related: Stop Sabotaging Your Gut
Take care!
Share This Post
-
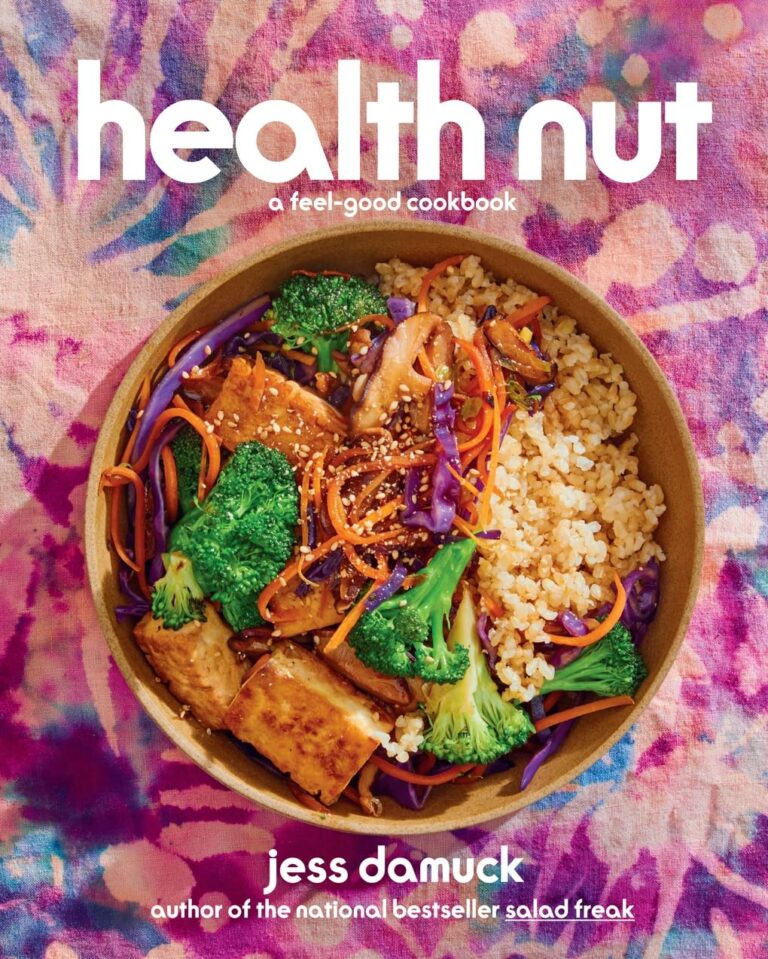
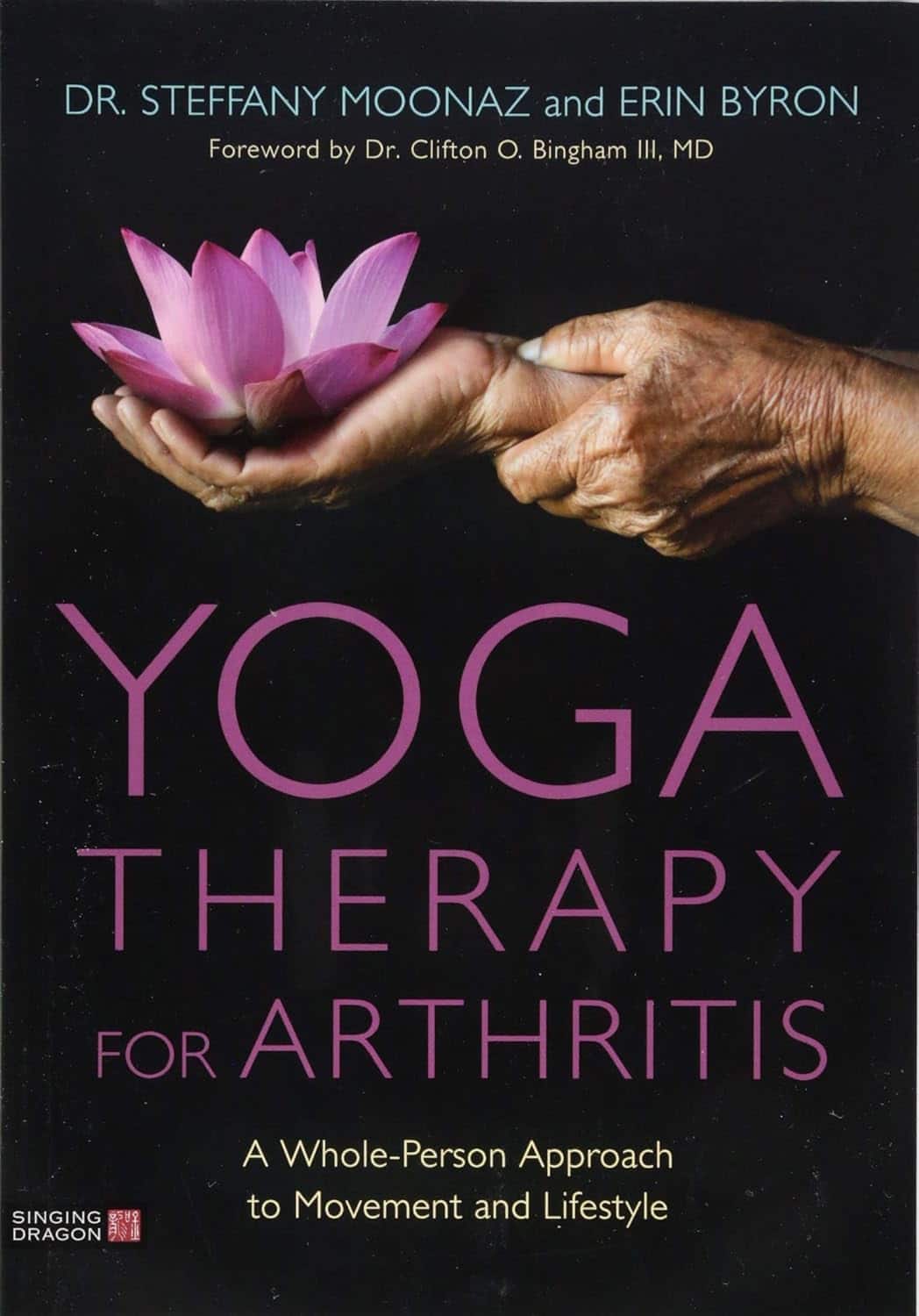
Yoga Therapy for Arthritis – by Dr. Steffany Moonaz & Erin Byron
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Two quick notes to start with:
- One of the problems with arthritis and exercise is that arthritis can often impede exercise.
- Another of the problems with arthritis and exercise is that some kinds of exercise can exacerbate arthritis.
This book deals with both of those issues, by providing yoga specifically tailored to living with arthritis. Indeed, the first-listed author’s PhD in public health was the result of 8 years of study developing an evidence-based yoga program for people with arthritis, including osteoarthritis and rheumatoid arthritis.
The authors take the view that arthritis is a whole-person disease (i.e. it affects all parts of you), and so addressing it requires a whole-person approach, which is what this book delivers.
As such, this is not just a book of asana (yoga postures). It does provide that, of course (as well as breathing exercises), but also its 328 pages additionally cover a lot of conscious work from the inside out, including attention to the brain, energy levels, pain, and so forth, and that the practice of yoga should not merely directly improve the joints via gentle physical exercise, but also should help to heal the whole person, including reducing stress levels, reducing physical tension, and with those two things, reducing inflammation also—and also, due to both that and the asana side of practice, better-functioning organs, which is always a bonus.
The style is interesting, as it refers to both science (8 pages of hard-science bibliography) and yogic principles (enough esoterica to put off, say, James Randi or Penn & Teller). This reviewer is very comfortable with both, and so if you, dear reader, are comfortable with both too, then you will surely enjoy this book.
Bottom line: if you or a loved one has arthritis, you’ll wish you got this book sooner.
Click here to check out Yoga Therapy For Arthritis, and live better!
Share This Post
-
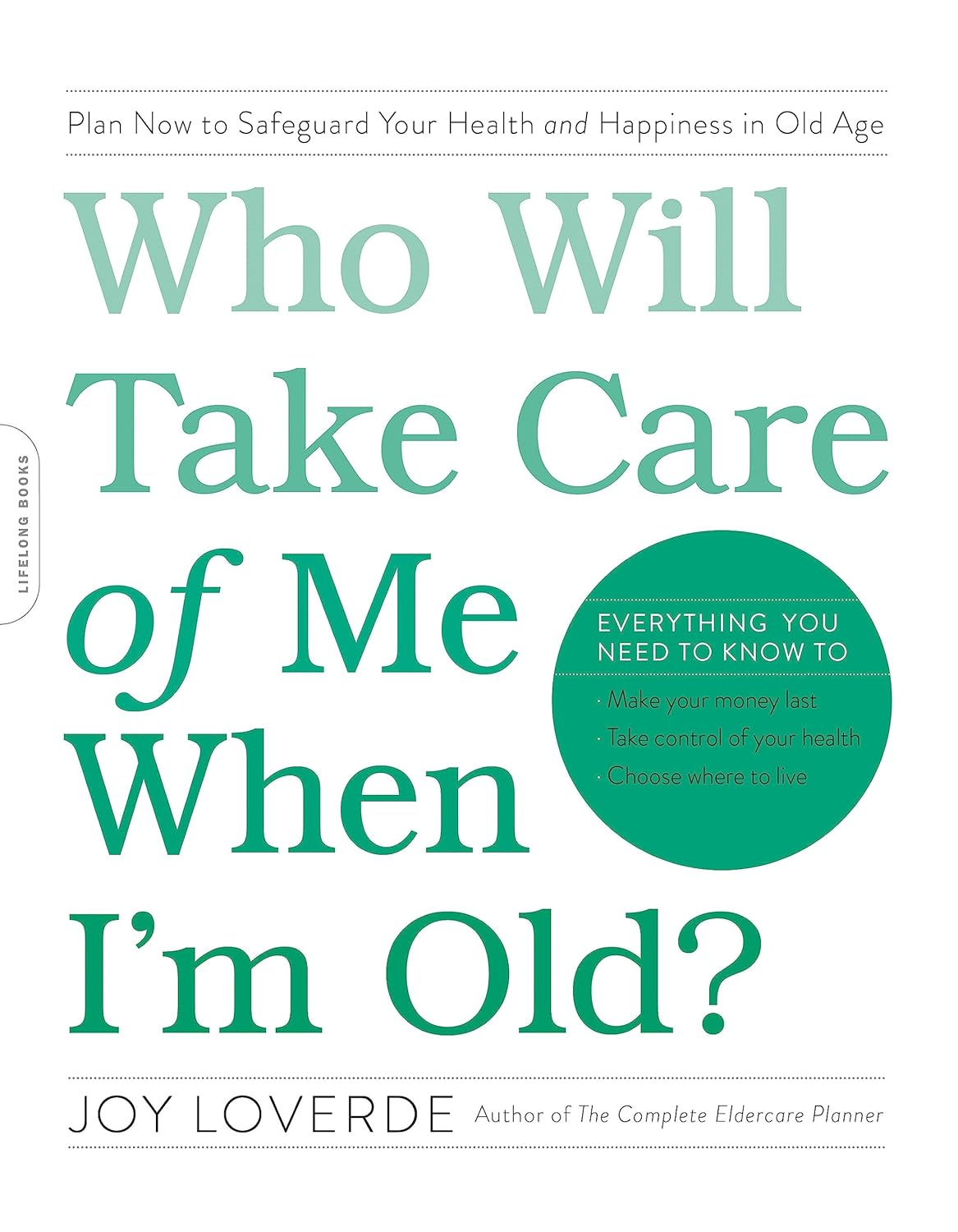
Who Will Take Care of Me When I’m Old? – by Joy Loverde
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Regular readers of 10almonds will know we’ve written before about how isolation kills (in numerous ways), and this book tackles that in much greater length and depth than we ever have room for here.
Specifically, she talks about preparing for medical and related (financial, living will in case of dementia, housing, etc) considerations down the line, with checklists and worksheets and such to make it easy, and help you make sure it actually gets done.
She also talks about creating a support network, from scratch if necessary (“foraging a family”), so that even if you will now be prepared to handle things alone, you’ll become a lot less likely to need to do so.
Unlike many books of this genre, she also covers managing your mortality; that “just shoot me” is not a plan, and what lessons can be learned from the dying to make our own last years the best they can be.
The style is upbeat and positive in outlook; less “prepare for doom” and more “get ready to do things right”, and it’s worth mentioning that the format is particularly helpful, outlining objectives towards the beginning of each chapter, and additional resources at the end of each chapter.
Over on Amazon, most of the reviews that contain any criticism are some manner of “I’m in my 70s and wish I had read this sooner”. Still, better late than never.
Bottom line: if you do not have an overabundance of support network around you, then this is an important book to read and to put into action.
Share This Post
Related Posts
-
Age Proof – by Dr. Rose Anne Kenny
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We don’t generally include an author bio, but in this case it’s worth noting that Dr. Kenny, the Chair of Medical Gerontology at Trinity College Dublin, with over 300 staff under her, has 704 peer-reviewed publications to her name, and enough awards and honors and achievements to more than fill a page on her university’s website.
In short, she knows her stuff.
A lot of the material in this book will not be completely new to regular 10almonds readers; there’s a lot about Blue Zones supercentenarians, the usual qualities associated with healthy longevity in those places (diet, lifestyle, etc), as well as genetic factors and epigenetic, and so forth.
Some items are… Not new, but not so commonly focused on in such works; for example, Dr. Kenny devotes a chapter to sleep, a chapter to laughter, a chapter to hormesis, and a chapter to sexual activity, amongst others.
Another thing she delivers that a lot of books of this kind don’t is that she has a collection of “Test Yourself” appendices, so that you can establish where you are relative to various benchmarks of aging.
Dr. Kenny also references her own work especially with TILDA (The Irish Longitudinal Study on Aging) that she has directed for many years, which has a vast amount of data and many important findings, which adds another extra strength to this book often not found in others.
The style is surprisingly personal, making it an enjoyable read as well as an educational one, and yet with a lot of hard science throughout—explained well for the layperson though, and thoroughly referenced with an extensive bibliography.
Bottom line: if you’d like to be (and continue to be!) “young for your years”, then this is an excellent book to get (and/or keep) you on the right track.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Non-Sleep Deep Rest: A Neurobiologist’s Take
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How to get many benefits of sleep, while awake!
Today we’re talking about Dr. Andrew Huberman, a neuroscientist and professor in the department of neurobiology at Stanford School of Medicine.
He’s also a popular podcaster, and as his Wikipedia page notes:
❝In episodes lasting several hours, Huberman talks about the state of research in a specific topic, both within and outside his specialty❞
Today, we won’t be taking hours, and we will be taking notes from within his field of specialty (neurobiology). Specifically, in this case:
Non-Sleep Deep Rest (NSDR)
What is it? To quote from his own dedicated site on the topic:
❝What is NSDR (Yoga Nidra)? Non-Sleep Deep Rest, also known as NSDR, is a method of deep relaxation developed by Dr. Andrew Huberman, a neuroscientist at Stanford University School of Medicine.
It’s a process that combines controlled breathing and detailed body scanning to bring you into a state of heightened awareness and profound relaxation. The main purpose of NSDR is to reduce stress, enhance focus, and improve overall well-being.❞
While it seems a bit bold of Dr. Huberman to claim that he developed yoga nidra, it is nevertheless reassuring to get a neurobiologist’s view on this:
How it works, by science
Dr. Huberman says that by monitoring EEG readings during NSDR, we can see how the brain slows down. Measurably!
- It goes from an active beta range of 13–30 Hz (normal waking) to a conscious meditation state of an alpha range of 8–13 Hz.
- However, with practice, it can drop further, into a theta range of 4–8 Hz.
- Ultimately, sustained SSDR practice can get us to 0.5–3 Hz.
This means that the brain is functioning in the delta range, something that typically only occurs during our deepest sleep.
You may be wondering: why is delta lower than theta? That’s not how I remember the Greek alphabet being ordered!
Indeed, while the Greek alphabet goes alpha beta gamma delta epsilon zeta eta theta (and so on), the brainwave frequency bands are:
- Gamma = concentrated focus, >30 Hz
- Beta = normal waking, 13–30 Hz
- Alpha = relaxed state, 8–13 Hz
- Theta = light sleep, 4–8 Hz
- Delta = deep sleep, 1–4 Hz
Source: Sleep Foundation ← with a nice infographic there too
NSDR uses somatic cues to engage our parasympathetic nervous system, which in turn enables us to reach those states. The steps are simple:
- Pick a time and place when you won’t be disturbed
- Lie on your back and make yourself comfortable
- Close your eyes as soon as you wish, and now that you’ve closed them, imagine closing them again. And again.
- Slowly bring your attention to each part of your body in turn, from head to toe. As your attention goes to each part, allow it to relax more.
- If you wish, you can repeat this process for another wave, or even a third.
- Find yourself well-rested!
Note: this engagement of the parasympathetic nervous system and slowing down of brain activity accesses restorative states not normally available while waking, but 10 minutes of NSDR will not replace 7–9 hours of sleep; nor will it give you the vital benefits of REM sleep specifically.
So: it’s an adjunct, not a replacement
Want to try it, but not sure where/how to start?
When you’re ready, let Dr. Huberman himself guide you through it in this shortish (10:49) soundtrack:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to try it, but not right now? Bookmark it for later
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
This Naked Mind – by Annie Grace
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve all read about the many, many, dangers of drinking. We’ve also probably all read about how to make the change to not drinking. Put things out of sight, tell your friends, have this rule, have this excuse (for not drinking) ready to give to people who challenge you, consider a support group, and so on.
What Annie Grace offers in this #1 bestseller is different:
A blend of mostly psychology and sociology, to examine the “liminal thinking” stages that funnel us to drink in the first place… and where that leads, and how to clamber back out of the pitcher plant we weren’t necessarily aware we were sliding into.
While she kicks off citing Jung, from a psychological perspective more of this book is CBTish, as it pertains a lot to examining the process of:
- belief—held and defended, based on the…
- conclusion—drawn, often irrationally, from the…
- experience—that we had upon acting on an…
- observation—often mistaking an illusion for the underlying…
- reality
…and how we can and often do go wrong at each step, and how little of the previous steps we can perceive at any given time.
What does this mean for managing/treating alcoholism or a tendency towards alchoholism?
It means interrupting those processes in a careful, surgically precise fashion, so that suddenly… The thing has no more power over us.
Whether you or a loved one struggle with a tendency to addiction (any addiction, actually, the advice goes the same), or are just curious about the wider factors at hand in the epidemiology of addiction, this book is for you.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: