Lost Connections – by Johann Hari
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Johann Hari had a long journey through (and out of!) depression, and shares his personal findings, including his disappointment with medical options, and a focus on the external factors that lead to depression.
And that’s key to this book—while he acknowledges later in the book that there are physiological factors involved in depression, he wants to look past things we can’t change (like genes accounting for 37% of depression) or things that there may be unwanted side-effects to changing (as in the case of antidepressants, for many people), to things we genuinely can choose.
And no, it’s not a “think yourself happy” book either; rather, it looks at nine key external factorsthat a) influence depression b) can mostly be changed.
If the book has a downside, it’s that the author does tend to extrapolate his own experience a lot more than might be ideal. If SSRIs didn’t help him, they are useless, and also the only kind of antidepressant. If getting into a green space helped him, a Londoner, someone who lives in the countryside will not be depressed in the first place. And so forth. It can also be argued that he cherry-picked data to arrive at some of his pre-decided conclusions. He also misinterprets data sometimes; which is understandable; he is after all a journalist, not a scientist.
Nevertheless, he offers a fresh perspective with a lot of ideas, and whether or not we agree with them all, new ideas tend to be worth reading. And if even one of his nine ideas helps you, that’s a win.
Bottom line: if you’d like to explore the treatment of depression from a direction other than medicalization or psychotherapy, then this is will be a good book for you.
Click here to check out Lost Connections, and reforge yours!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The End of Alzheimer’s – by Dr. Dale Bredesen
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This one didn’t use the “The New Science Of…” subtitle that many books do, and this one actually is a “new science of”!
Which is exciting, and/but comes with the caveat that the overall protocol itself is still undergoing testing, but the results so far are promising. The constituent parts of the protocol are for the most already well-established, but have not previously been put together in this way.
Dr. Bredesen argues that Alzheimer’s Disease is not one condition but three (medical consensus agrees at least that it is a collection of conditions, but different schools of thought slice them differently), and outlines 36 metabolic factors that are implicated, and the good news is, most of them are within our control.
Since there’s a lot to put together, he also offers many workarounds and “crutches”, making for very practical advice.
The style of the book is on the hard end of pop-science, that is to say while the feel and tone is very pop-sciencey, there are nevertheless a lot of words that you might know but your spellchecker probably wouldn’t. He does explain everything along the way, but this does mean that if you’re not already well-versed, you can’t just dip in to a later point without reading the earlier parts.
Bottom line: even if you only implement half the advice in this book, you’ll be doing your long-term cognitive health a huge favor.
Click here to check out The End of Alzheimer’s, and keep cognitive decline at bay!
Share This Post
-
This salt alternative could help reduce blood pressure. So why are so few people using it?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
One in three Australian adults has high blood pressure (hypertension). Excess salt (sodium) increases the risk of high blood pressure so everyone with hypertension is advised to reduce salt in their diet.
But despite decades of strong recommendations we have failed to get Australians to cut their intake. It’s hard for people to change the way they cook, season their food differently, pick low-salt foods off the supermarket shelves and accept a less salty taste.
Now there is a simple and effective solution: potassium-enriched salt. It can be used just like regular salt and most people don’t notice any important difference in taste.
Switching to potassium-enriched salt is feasible in a way that cutting salt intake is not. Our new research concludes clinical guidelines for hypertension should give patients clear recommendations to switch.
What is potassium-enriched salt?
Potassium-enriched salts replace some of the sodium chloride that makes up regular salt with potassium chloride. They’re also called low-sodium salt, potassium salt, heart salt, mineral salt, or sodium-reduced salt.
Potassium chloride looks the same as sodium chloride and tastes very similar.
Potassium-enriched salt works to lower blood pressure not only because it reduces sodium intake but also because it increases potassium intake. Insufficient potassium, which mostly comes from fruit and vegetables, is another big cause of high blood pressure.
What is the evidence?
We have strong evidence from a randomised trial of 20,995 people that switching to potassium-enriched salt lowers blood pressure and reduces the risks of stroke, heart attacks and early death. The participants had a history of stroke or were 60 years of age or older and had high blood pressure.
An overview of 21 other studies suggests much of the world’s population could benefit from potassium-enriched salt.
The World Health Organisation’s 2023 global report on hypertension highlighted potassium-enriched salt as an “affordable strategy” to reduce blood pressure and prevent cardiovascular events such as strokes.
What should clinical guidelines say?
We teamed up with researchers from the United States, Australia, Japan, South Africa and India to review 32 clinical guidelines for managing high blood pressure across the world. Our findings are published today in the American Heart Association’s journal, Hypertension.
We found current guidelines don’t give clear and consistent advice on using potassium-enriched salt.
While many guidelines recommend increasing dietary potassium intake, and all refer to reducing sodium intake, only two guidelines – the Chinese and European – recommend using potassium-enriched salt.
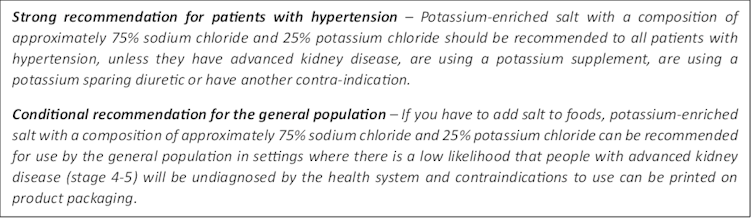
To help guidelines reflect the latest evidence, we suggested specific wording which could be adopted in Australia and around the world:
Recommended wording for guidance about the use of potassium-enriched salt in clinical management guidelines. Why do so few people use it?
Most people are unaware of how much salt they eat or the health issues it can cause. Few people know a simple switch to potassium-enriched salt can help lower blood pressure and reduce the risk of a stroke and heart disease.
Limited availability is another challenge. Several Australian retailers stock potassium-enriched salt but there is usually only one brand available, and it is often on the bottom shelf or in a special food aisle.
Potassium-enriched salts also cost more than regular salt, though it’s still low cost compared to most other foods, and not as expensive as many fancy salts now available.
It looks and tastes like normal salt.
Jimmy Dean/UnsplashA 2021 review found potassium-enriched salts were marketed in only 47 countries and those were mostly high-income countries. Prices ranged from the same as regular salt to almost 15 times greater.
Even though generally more expensive, potassium-enriched salt has the potential to be highly cost effective for disease prevention.
Preventing harm
A frequently raised concern about using potassium-enriched salt is the risk of high blood potassium levels (hyperkalemia) in the approximately 2% of the population with serious kidney disease.
People with serious kidney disease are already advised to avoid regular salt and to avoid foods high in potassium.
No harm from potassium-enriched salt has been recorded in any trial done to date, but all studies were done in a clinical setting with specific guidance for people with kidney disease.
Our current priority is to get people being managed for hypertension to use potassium-enriched salt because health-care providers can advise against its use in people at risk of hyperkalemia.
In some countries, potassium-enriched salt is recommended to the entire community because the potential benefits are so large. A modelling study showed almost half a million strokes and heart attacks would be averted every year in China if the population switched to potassium-enriched salt.
What will happen next?
In 2022, the health minister launched the National Hypertension Taskforce, which aims to improve blood pressure control rates from 32% to 70% by 2030 in Australia.
Potassium-enriched salt can play a key role in achieving this. We are working with the taskforce to update Australian hypertension management guidelines, and to promote the new guidelines to health professionals.
In parallel, we need potassium-enriched salt to be more accessible. We are engaging stakeholders to increase the availability of these products nationwide.
The world has already changed its salt supply once: from regular salt to iodised salt. Iodisation efforts began in the 1920s and took the best part of 100 years to achieve traction. Salt iodisation is a key public health achievement of the last century preventing goitre (a condition where your thyroid gland grows larger) and enhancing educational outcomes for millions of the poorest children in the world, as iodine is essential for normal growth and brain development.
The next switch to iodised and potassium-enriched salt offers at least the same potential for global health gains. But we need to make it happen in a fraction of the time.
Xiaoyue Xu (Luna), Scientia Lecturer, UNSW Sydney; Alta Schutte, SHARP Professor of Cardiovascular Medicine, UNSW Sydney, and Bruce Neal, Executive Director, George Institute Australia, George Institute for Global Health
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
The Complete Anti-Inflammatory Diet for Beginners – by Dorothy Calimeris and Lulu Cook
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
First, about the authors: notwithstanding the names, Calimeris is the cook, and Cook is the nutritionist (and an RDN at that).
As for the book: we get a good primer on the science of inflammation, what it is, why it happens, what things are known to cause/trigger it, and what things are known to fight it. They do also go outside of nutrition a bit for this, speaking briefly on other lifestyle factors too, but the main focus is of course nutrition.
As for the recipes: while distinctly plants-forward (as one might expect of an anti-inflammatory eating book), it’s not outright vegan or even vegetarian, indeed, in the category of main dishes, there are sections for:
- Vegetarian and vegan
- Fish and shellfish
- Poultry and meat
…as well as, before and after those, sections for breakfast and brunch and snacks and sweets. As well as a not-to-be-underestimated section, for sauces, condiments, and dressings. This is important, because those are quite often the most inflammatory parts of an otherwise healthy meal! So being able to make anti-inflammatory versions is a real boon.
The recipes are mostly not illustrated, but the steps are very clearly described and easy to follow.
Bottom line: if inflammation is currently on your to-tackle list, this book will be an excellent companion in the kitchen.
Share This Post
Related Posts
-
Radishes vs Endives – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing radishes to endives, we picked the endives.
Why?
These are both great, but there’s a clear winner here in every category!
In terms of macros, radishes have more carbs while endives have more fiber and protein.
In the category of vitamins, radishes have more of vitamins B6 and C, while endives have more of vitamins A, B1, B2, B4, B5, B7, B9, E, K, and choline.
When it comes to minerals, things are not less one-sided: radishes have more selenium, while endives have more calcium, copper, iron, magnesium, manganese, phosphorus, potassium, and zinc.
You may be thinking: but what about radishes’ shiny red bit? Doesn’t that usually mean more of something important, like carotenoids or anthocyanins or something? And the answer is that the red pigment in radishes is so thinly-distributed on the exterior that it’s barely there and if we’re looking at values per 100g, it’s a tiny fraction of a tiny fraction.
In both cases, their bitter taste comes mostly from flavonols, of which mostly kaempferol, of which endives have about 20x what radishes have, on average.
All in all, an overwhelming win for endives.
Want to learn more?
You might like to read:
Enjoy Bitter Foods For Your Heart & Brain
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Is Vitamin C Worth The Hype? (Doctorly Investigates)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Double Board-Certified Dermatologists Dr. Muneeb Shah & Dr. Luke Maxfield weigh in on vitamin C; is it worth the hype?
Yes it is, but…
There are some caveats, for example:
- It’s best to apply vitamin C on clean, dry skin and let it set before layering other products.
- Avoid mixing with oxidants like benzoyl peroxide (cancels out antioxidant effects).
- Avoid combining with copper (may negate brightening benefits).
- Do not use with hypochlorous acid (oxidative reactions cancel out benefits).
- Be cautious with retinol due to irritation risks.
However, used correctly, it does give very worthy benefits, and they recommend:
- Morning use: acts as an antioxidant, pairs well with sunscreen for better protection from sun and environmental damage.
- Night use: maximizes functions like improving tone, collagen production, texture, and reducing wrinkles.
That’s not to say that at night it stops being an antioxidant or during the day it isn’t critical for collagen synthesis, but it is to say: because of the different things our bodies typically encounter and/or do during the day or night, those are the best times to get the most out of those benefits.
They also review some popular products; here are some notes on their comments about them:
- Skinceuticals C E Ferulic: research-backed, $180, effective but potentially irritating.
- Skinceuticals Phloretin CF: includes 0.5% salicylic acid, good for acne-prone skin.
- Dermatology Vitamin C E Ferulic: relatively more affordable ($70), fragrance-free, includes peptides and ceramides.
- Drunk Elephant C-Firma: powder-to-serum formula, sued for patent infringement.
- Paula’s Choice C15 Booster: reformulated, fragrance-free, similar to Skinceuticals.
- Neutrogena Vitamin C Capsules: stabilized 20% ascorbic acid, single-use, travel-friendly.
- La Roche-Posay Vitamin C Serum: contains fragrance and alcohol, not ideal for sensitive skin.
- Matter of Fact Vitamin C Serum: includes ascorbic acid and ferulic acid, oily texture for dry skin.
- Medik8 Super C Ferulic: stable 30% ethyl ascorbic acid, lightweight texture.
- Naturium Vitamin C Complex: multi-form Vitamin C with niacinamide, alpha arbutin, and turmeric.
- Timeless Vitamin C Serum: affordable ($20), 20% ascorbic acid with E and ferulic acid.
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like:
More Than Skin-Deep: Six Ways To Eat For Healthier Skin ← this one’s about a lot more than just vitamin C 😎
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
5 Ways To Make Your Smoothie Blood Sugar Friendly (Avoid the Spike!)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
At 10almonds, we are often saying “eat whole fruit; don’t drink your calories”. Whole fruit is great for blood sugars; fruit juices and many smoothies on the other hand, not so much. Especially juices, being near-completely or perhaps even completely stripped of fiber, but even smoothies have had a lot of the fiber broken down and are still a liquid, meaning they are very quickly and easily digestible, and thus their sugars (whatever carbs are in there) can just zip straight into your veins.
However, there are ways to mitigate this…
Slow it down
The theme here is “give the digestive process something else to do”; some things are more quickly and easily digestible than others, and if it’s working on breaking down some of the slower things, it’s not waving sugars straight on through; they have to wait their turn.
To that end, recommendations include:
- Full-fat Greek yogurt which provides both protein and fat, helping to slow down the absorption of sugar. Always choose unsweetened versions to avoid added sugars, though!
- Coconut milk (canned) which is low in sugar and carbs, high in fat. This helps reduce blood sugar spikes, as she found through personal experimentation too.
- Avocado which is rich in healthy fats that help stabilize blood sugar. As a bonus, it blends well into smoothies without affecting the taste much.
- Coconut oil which contains medium-chain triglycerides (MCTs) that are quickly absorbed for energy without involving glucose, promoting fat-burning and reducing blood sugar spikes.
- Collagen powder which is a protein that helps lower blood sugar spikes while also supporting muscle growth, skin, and joints.
For more on all of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: