The Kindness Method – by Shahroo Izadi
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Shahroo Izadi here covers everything from alcohol addiction to procrastination to weight loss. It’s a catch-all handbook for changing your habits—in general, and/or in whatever area of your life you most feel you want or need to.
She herself went from yo-yo dieting to a stable healthy lifestyle, and wants to share with us how she did it. So she took what worked for her, organized and dilstilled it, and named it “the kindness method”, which…
- promotes positivity not in a “head in the sand” sense but rather: you have strengths, let’s find them and use them
- offers many exploratory exercises to help you figure out what’s actually going to be best for you
- plans support in advance—you’re going to be your own greatest ally here
Basically it’s about:
- being kind to yourself rather than setting yourself up to fail, and “judging a fish by how well it can climb a tree”
- being kind to yourself by being compassionate towards your past self and moving on with lessons learned
- being kind to yourself by getting things in order for your future self, because you need to treat your future self like a loved one
In fact, why not buy a copy of this book as a gift for your future self?
Click Here To Order Your Copy of “The Kindness Method” on Amazon Today!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How a Michigan community center supports young people’s mental health
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Even before the COVID-19 pandemic made mental health problems worse for people of all ages, young people already struggled with a lack of support and treatment for issues like depression, anxiety, and ADHD.
Like many states, Michigan doesn’t have enough health care providers, and youth mental health professionals are in high demand.
Some local groups step in to support kids when they aren’t getting the help they need or experience long wait times for services.
To learn more about how one community-based organization tackles these challenges, Public Good News spoke with Avion Williams, Youth Coordinator at Community Family Life Center.
Here’s what she said.
[Editor’s note: The contents of this interview have been edited for length and clarity.]
Public Good News: Can you tell us more about your organization and where you’re located?
A.W.: Community Family Life Center is a community outreach center. We offer a multitude of after-school programs and services to Ypsilanti-Ann Arbor and even the Belleville community.
Ypsilanti is a small community. It was originally a farmer’s town. You will still see a lot of older families here.
A lot of our restaurants are like mom-and-pop shops. We have our downtown area, which is now being modernized a little bit, but again, a lot of shops are family-owned businesses that have been around for decades.
We have a lot of colleges. We have Eastern Michigan, which is the college I actually attend, and that’s in Ypsilanti. But we also have colleges right next door that are 10 minutes away, like University of Michigan and Concordia.
So it’s a college town, very family-oriented, but also a very small town with not too many resources.
PGN: Can you share some of your experiences as a youth coordinator trying to help young people access your organization’s services and programs?
A.W.: So we offer a ton of different programs, but our main focus is for kids to have something to do. There’s definitely a lot of young people in Ypsilanti.
I’m 25, and when I was in high school, a lot of people in my grade were having children. And they weren’t just having one baby, they were having multiple babies. You know, maybe one in tenth grade, another when we graduated our senior year, another right after. So a lot of people my age have a lot of children. And now I work with a lot of their children.
Many of those children come to after-school programs, and they’re in need of not just school things like math and reading, but they’re in need of, you know, love and care. Maybe mom can’t do everything because she has to work two or three jobs, or she doesn’t have the best financial help, and so she doesn’t know what to do.
And these young children get stuck with teachers that may not necessarily know how to give the best support, because maybe they’re stressed.
We have after-school programs and community centers like ours, where we get all of that.
Not only do we have to deal with mental health, we have to deal with these babies being hungry. We have to teach what mental health is.
PGN: What about therapy? How does that fit into the picture?
A.W.: Sometimes in society, people just throw therapy out there, like, ‘Go to therapy, go to therapy, go to therapy,’ but they don’t talk about the process of what it’s like getting a therapist.
I love the idea of therapy. Don’t get me wrong. Having somebody to talk to is very real. Having the right person to talk to is very real, right?
But I think sometimes we don’t talk about how everybody is not able to get therapy.
And a lot of times when people are ready for therapy, it’s after everything has happened.
You know, ‘Mom is gone, dad is gone. I’m doing terribly in school now. I’m acting out. Now I’m lashing out. I’m super hungry. I don’t have money for this. I don’t have money for that. I don’t know what to do about this…’ and then it’s like, ‘okay, I think I need therapy.’
Instead of us approaching it as, ‘Hey, this person’s mom is a young mom, maybe we should see if we can get therapy for both of them.’ Or when that child is being born, or when we see this young mom at the hospital and we see that she’s pregnant. Let’s offer some help before things start to hit the fan, right?
And maybe this mom doesn’t even have the proper health care to receive therapy, or let alone, doesn’t have the money to pay for it.
PGN: How does your organization respond to this need?
A.W.: We have a lot of ways to access our therapists. We started maybe two years ago, and at first a lot of people weren’t going. And now there’s so many people going that yes, we have this wait list.
So we also all do daily check-ins with our kids. We really do get to know our kids and their families and have consistent conversations with parents.
I always tell my kids this is a safe space to talk. I’m open to hear anything my students have to say.
This article first appeared on Public Good News and is republished here under a Creative Commons license.
Share This Post
-
From banning junk food ads to a sugar tax: with diabetes on the rise, we can’t afford to ignore the evidence any longer
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
There are renewed calls this week for the Australian government to implement a range of measures aimed at improving our diets. These include restrictions on junk food advertising, improvements to food labelling, and a levy on sugary drinks.
This time the recommendations come from a parliamentary inquiry into diabetes in Australia. Its final report, tabled in parliament on Wednesday, was prepared by a parliamentary committee comprising members from across the political spectrum.
The release of this report could be an indication that Australia is finally going to implement the evidence-based healthy eating policies public health experts have been recommending for years.
But we know Australian governments have historically been unwilling to introduce policies the powerful food industry opposes. The question is whether the current government will put the health of Australians above the profits of companies selling unhealthy food.
benjamas11/Shutterstock Diabetes in Australia
Diabetes is one of the fastest growing chronic health conditions in the nation, with more than 1.3 million people affected. Projections show the number of Australians diagnosed with the condition is set to rise rapidly in coming decades.
Type 2 diabetes accounts for the vast majority of cases of diabetes. It’s largely preventable, with obesity among the strongest risk factors.
This latest report makes it clear we need an urgent focus on obesity prevention to reduce the burden of diabetes. Type 2 diabetes and obesity cost the Australian economy billions of dollars each year and preventive solutions are highly cost-effective.
This means the money spent on preventing obesity and diabetes would save the government huge amounts in health care costs. Prevention is also essential to avoid our health systems being overwhelmed in the future.
What does the report recommend?
The report puts forward 23 recommendations for addressing diabetes and obesity. These include:
- restrictions on the marketing of unhealthy foods to children, including on TV and online
- improvements to food labelling that would make it easier for people to understand products’ added sugar content
- a levy on sugary drinks, where products with higher sugar content would be taxed at a higher rate (commonly called a sugar tax).
These key recommendations echo those prioritised in a range of reports on obesity prevention over the past decade. There’s compelling evidence they’re likely to work.
Restrictions on unhealthy food marketing
There was universal support from the committee for the government to consider regulating marketing of unhealthy food to children.
Public health groups have consistently called for comprehensive mandatory legislation to protect children from exposure to marketing of unhealthy foods and related brands.
An increasing number of countries, including Chile and the United Kingdom, have legislated unhealthy food marketing restrictions across a range of settings including on TV, online and in supermarkets. There’s evidence comprehensive policies like these are having positive results.
In Australia, the food industry has made voluntary commitments to reduce some unhealthy food ads directly targeting children. But these promises are widely viewed as ineffective.
The government is currently conducting a feasibility study on additional options to limit unhealthy food marketing to children.
But the effectiveness of any new policies will depend on how comprehensive they are. Food companies are likely to rapidly shift their marketing techniques to maximise their impact. If any new government restrictions do not include all marketing channels (such as TV, online and on packaging) and techniques (including both product and brand marketing), they’re likely to fail to adequately protect children.
Food labelling
Food regulatory authorities are currently considering a range of improvements to food labelling in Australia.
For example, food ministers in Australia and New Zealand are soon set to consider mandating the health star rating front-of-pack labelling scheme.
Public health groups have consistently recommended mandatory implementation of health star ratings as a priority for improving Australian diets. Such changes are likely to result in meaningful improvements to the healthiness of what we eat.
Regulators are also reviewing potential changes to how added sugar is labelled on product packages. The recommendation from the committee to include added sugar labelling on the front of product packaging is likely to support this ongoing work.
But changes to food labelling laws are notoriously slow in Australia. And food companies are known to oppose and delay any policy changes that might hurt their profits.
Health star ratings are not compulsory in Australia. BLACKDAY/Shutterstock A sugary drinks tax
Of the report’s 23 recommendations, the sugary drinks levy was the only one that wasn’t universally supported by the committee. The four Liberal and National party members of the committee opposed implementation of this policy.
As part of their rationale, the dissenting members cited submissions from food industry groups that argued against the measure. This follows a long history of the Liberal party siding with the sugary drinks industry to oppose a levy on their products.
The dissenting members didn’t acknowledge the strong evidence that a sugary drinks levy has worked as intended in a wide range of countries.
In the UK, for example, a levy on sugary drinks implemented in 2018 has successfully lowered the sugar content in UK soft drinks and reduced sugar consumption.
The dissenting committee members argued a sugary drinks levy would hurt families on lower incomes. But previous Australian modelling has shown the two most disadvantaged quintiles would reap the greatest health benefits from such a levy, and accrue the highest savings in health-care costs.
What happens now?
Improvements to population diets and prevention of obesity will require a comprehensive and coordinated package of policy reforms.
Globally, a range of countries facing rising epidemics of obesity and diabetes are starting to take such strong preventive action.
In Australia, after years of inaction, this week’s report is the latest sign that long-awaited policy change may be near.
But meaningful and effective policy change will require politicians to listen to the public health evidence rather than the protestations of food companies concerned about their bottom line.
Gary Sacks, Professor of Public Health Policy, Deakin University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
The Knowledge That Harvard Medical School’s Clinical Instructor Dr. Monique Tello Thinks Everyone SHOULD Have About Heart Health
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
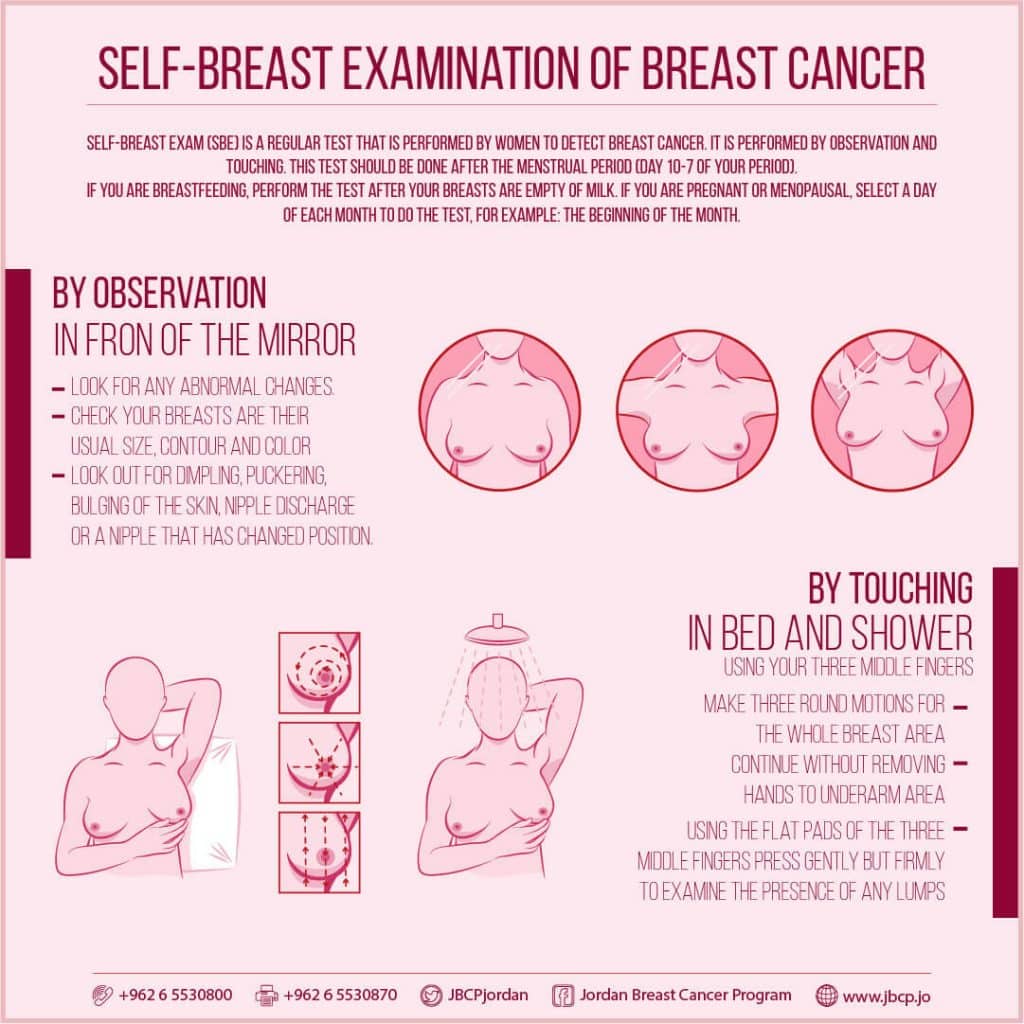
Anyone (who has not had a double mastectomy, anyway) can get breast cancer.
Breast cancer, if diagnosed early (before it spreads), has a 98% survival rate.
That survival rate drops to 31% if diagnosed after it has spread through the body.
(The US CDC’s breast cancer “stat bite” page has more stats and interactive graphs, so click here to see those charts and get the more detailed low-down on mortality/survival rates with various different situations)
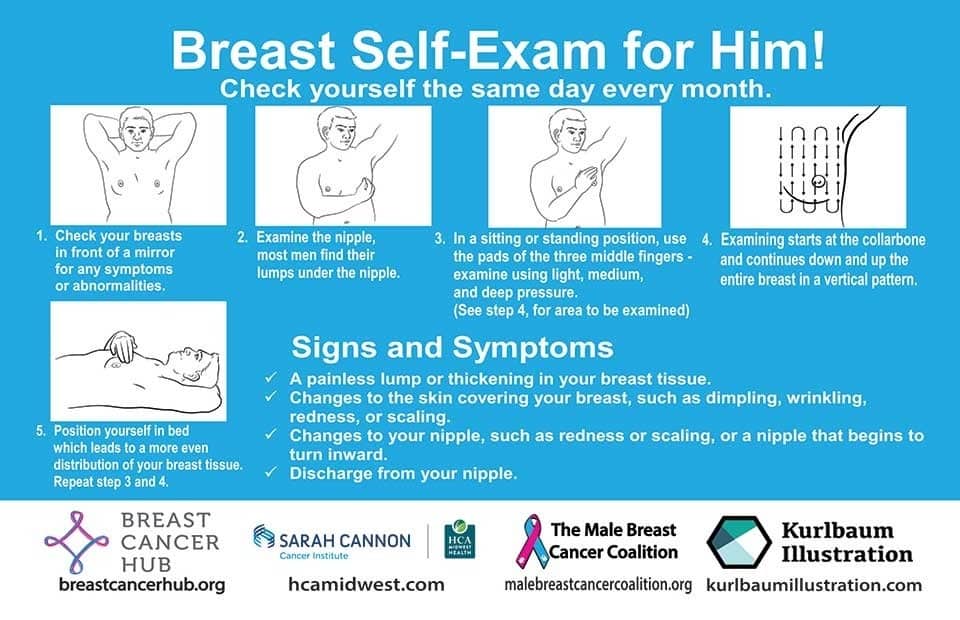
We think that the difference between 98% and 31% survival rates is more than enough reason to give ourselves a monthly self-check at the very least! You’ve probably seen how-to diagrams before, but here are instructions for your convenience:
This graphic created by the Jordan Breast Cancer Program (check them out, as they have lots of resources)
If you don’t have the opportunity to take matters into your own hands right now, rather than just promise yourself “I’ll do that later”, take this free 4-minute Breast Health Assessment from Aurora Healthcare. Again, we think the difference early diagnosis can make to your survival chances make these tests well worth it.
Lest we forget, men can also get breast cancer (the CDC has a page for men too), especially if over 50. But how do you check for breast cancer, when you don’t have breasts in the commonly-understood sense of the word?
So take a moment to do this (yes, really actually do it!), and set a reminder in your calendar to repeat it monthly—there really is no reason not to! Take care of yourself; you’re important.
Pssst! Did you scroll past the diagrams, looking for the online 4-minute test promised by the subtitle? If so, scroll back up; the link is in the middle!
Harvard Medical School’s Clinical Instructor’s Five-Point Plan for Heart Health
Dr. Monique Tello, M.D., M.P.H., is a practicing physician at Massachusetts General Hospital, director of research and academic affairs for the MGH DGM Healthy Lifestyle Program, clinical instructor at Harvard Medical School, and author of the evidence-based lifestyle change guide Healthy Habits for Your Heart.
Here are what she says are the five most important factors to help keep your ticker ticking:
5. Have (at most) a moderate alcohol intake! While there are polyphenols such as resveratrol in red wine that could boost heart health, there’s so little per glass that you may need 100–1000 glasses to get the dosage that provides benefits in mouse studies. If you’re not a mouse, it may not be as beneficial, and Dr. Tello recommends drinking no more than one glass per day of any alcohol. What constitutes a glass? It varies from one kind of drink to another, so here’s a handy guide.
4. Don’t smoke. Best of all to never start. But if you did, quit. Simple as that. There is no healthy amount of smoking. While paradoxically, quitting smoking may of course be stressful to you, the long term gains are considered more than worth it. As with all advice, do consult your own physician for guidance, as individual circumstances may vary, and that may change the best approach for you.
3. Maintain a healthy body weight. While BMI (Body Mass Index) is not a perfect system, it’s a system in popular use, and Dr. Tello recommends keeping a BMI between 18.5 and 24.9.
What’s your BMI? It takes into account your height and weight; here’s a Quick BMI Calculator for your convenience.
2. Keep a healthy level of physical activity—which ideally means at least 30 minutes per day vigorous activity, but obviously if you’re not used to this, take it slowly and build up over time. Even just small lifestyle changes (walking where possible, taking the stairs instead of the elevator where possible, etc) can add up to a big difference.
1. Enjoy a healthy diet. This is the single most important thing, and the best modern scientific consensus holds that the best diet contains plenty of vegetables, fruits and nuts, whole grains, and omega-3 fatty acids, while it avoids processed meats, sugar-sweetened beverages, trans fats (what are trans fats?), and too much sodium.
Share This Post
Related Posts
-
Get Better Sleep: Beyond The Basics
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
First though, for the sake of being methodical, let’s quickly note the basics:
- Aim for 7–9 hours per night
- Set a regular bedtime and (equally important!) regular getting-up time
- Have a 2-hour wind-down period before bed, to decompress from any stresses of the day
- Minimal device/screen usage before bed
- Abstain from stimulants for as long before bed as reasonably possible (caffeine elimination halflife is 4–8 hours depending on your genes, call it 6 hours average to eliminate half (not the whole lot), and you’ll see it’s probably best to put a cap on it earlier rather than later).
- Abstain from alcohol, ideally entirely, but allow at least 1hr/unit before bed. So for example, 1hr for a 1oz single shot of spirits, or 2–3 hours for a glass of wine (depending on size), or 3–4 hours for a martini (depending on recipe). Not that that is not the elimination time, nor even the elimination halflife of alcohol, it’s just a “give your body a chance at least” calculation. If you like to have a drink to relax before bed, then well, only you can decide what you like more: that or actually getting restorative sleep.
- Consider a warm bath/shower before bed, if that suits your schedule.
- Wash and change your bedsheets more often than seems necessary. Or if that’s too onerous, at least change the pillowcases more often, which makes quite a difference already.
- Lower the temperature of your bedroom shortly before bedtime; this will help cue the body to produce melatonin
- Make your bedroom as dark as reasonably possible. Invest in blackout blinds/curtains, and remove any pesky electronics, or at least cover their little LEDs if it’s something that reasonably needs to remain on.
Ok, now, onwards…
Those 7–9 hours? Yes, it goes for you too.
A lot of people mistake getting 6 hours sleep per night for only needing 6 hours sleep per night. Sure, you may still be alive after regularly getting 6 hours, but (unless you have a rare mutation of the ADRB1 gene) it will be causing harm, and yes, that includes later in life; we don’t stop needing so much sleep, even stop getting it:
Why You Probably Need More Sleep
With this in mind, it becomes important to…
Prioritize your sleep—which means planning for it!
When does your bedtime routine start? According to sleep scientist Dr. Lisa Matricciani, it starts before breakfast. This is because the things we do earlier in the day can greatly affect the amount (and quality) of sleep we get later. For example, a morning moderate-to-intense exercise session greatly improves sleep at night:
Planning Ahead For Better Sleep
As for quality, that is as important as quantity, and it’s not just about “soundness” of sleep:
The 6 Dimensions Of Sleep (And Why They Matter)
“What gets measured, gets done” goes for sleep too
Sleep-deprived people usually underestimate how sleep-deprived they are. This is for the same reason as why drunk people usually underestimate how drunk they are—to put it in words that go for both situations: a cognitively impaired person lacks the cognitive function to realize how cognitively impaired they are.
Here’s the science on that, by the way:
How Sleep-Deprived Are You, Really?
For that reason, we recommend using sleep-tracking software (there are many apps for that) on your phone or, ideally, a wearable device (such as a smartwatch or similar).
A benefit of doing so is that we don’t think “well, I slept from 10pm to 6am, so that’s 8 hours”, if our device tells us we slept between 10:43pm and 5:56 am with 74% sleep efficiency because we woke up many times.
As an aside, sleep efficiency should be about 85%, by the way. Why not 100%, you ask? It’s because if your body is truly out like a light for the entire night, something is wrong (either you were very sleep-deprived, or you have been drugged, that kind of thing). See also:
An unbroken night’s sleep is a myth. Here’s what good sleep looks like.
So waking up during the night is normal, and nothing to worry about per se. If you do find trouble getting back to sleep, though:
How to Fall Back Asleep After Waking Up in the Middle of the Night
Be careful about how you try to supplement sleep
This goes both for taking substances of various kinds, and napping. Some sleep aids can help, but many are harmful and/or do not really work as such; here’s a rundown of examples of those:
Safe Effective Sleep Aids For Seniors?
And when it comes to napping, timing is everything:
How To Nap Like A Pro (No More “Sleep Hangovers”!)
Want to know a lot more?
This is the book on sleep:
Why We Sleep – by Dr. Matthew Walker
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Dodging Dengue In The US
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dengue On The Rise
We wrote recently about dengue outbreaks in the Americas, with Puerto Rico declaring an epidemic. Cases are now being reported in Florida too, and are likely to spread, so it’s good to be prepared, if your climate is of the “warm and humid” kind.
If you want to catch up on the news first, here you go:
- UN health agency cites tenfold increase in reported cases of dengue over the last generation
- Puerto Rico has declared an epidemic following a spike in dengue cases
- Dengue fever confirmed in Florida Keys as US on watch for rise in mosquito illness
Note: dengue is far from unheard of in Florida, but the rising average temperatures in each year mean that each year stands a good chance of seeing more cases than the previous. It’s been climbing since at least 2017, took a dip during the time of COVID restrictions keeping people at home more, and then for the more recent years has been climbing again since.
What actually is it?
Dengue is a viral, mosquito-borne disease, characterized by fever, vomiting, muscle pain, and a rash, in about 1 in 4 cases.
Which can sound like “you’ll know if you have it”, but in fact it’s usually asymptomatic for a week or more after infection, so, watch out!
What next, if those symptoms appear?
The good news is: the fever will usually last less than a week
The bad news is: a day or so after that the fever subsided, the more serious symptoms are likely to start—if they’re going to.
If you’re unlucky enough to be one of the 1 in 20 who get the serious symptoms, then you can expect abdominal cramps, repeat vomiting, bleeding from various orifices (you may not get them all, but all are possible), and (hardly surprising, given the previous items) “extreme fatigue and restlessness”.
If you get those symptoms, then definitely get to an ER as soon as possible, as dengue can become life-threatening within hours of such.
Read more: CDC | Symptoms of Dengue and Testing
While there is not a treatment for dengue per se, the Emergency Room will be better able to manage your symptoms and thus keep you alive long enough for them to pass.
If you’d like much more detail (on symptoms, seriousness, at-risk demographics, and prognosis) than what the CDC offers, then…
Read more: BMJ | Dengue Fever
Ok, so how do we dodge the dengue?
It sounds flippant to say “don’t get bitten”, but that’s it. However, there are tips are not getting bitten:
- Use mosquito-repellent, but it has to contain >20% DEET, so check labels
- Use mosquito nets where possible (doors, windows, etc, and the classic bed-tent net is not a bad idea either)
- Wear clothing that covers your skin, especially during the day—it can be light clothing; it doesn’t need to be a HazMat suit! But it does need to reduce the area of attack to reduce the risk of bites.
- Limit standing water around your home—anything that can hold even a small amount of standing water is a potential mosquito-breeding ground. Yes, even if it’s a crack in your driveway or a potted bromeliad.
Further reading
You might also like to check out:
Stickers and wristbands aren’t a reliable way to prevent mosquito bites. Here’s why
…and in case dengue wasn’t bad enough:
Mosquitoes can spread the flesh-eating Buruli ulcer. Here’s how you can protect yourself
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Pomegranate vs Cherries – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing pomegranate to cherries, we picked the pomegranate.
Why?
In terms of macros, pomegranate is slightly higher in carbs, and/but 4x higher in fiber. That’s already a good start for pomegranates. Lest we be accused of cherry-picking, though, we’ll mention that pomegranate is also slightly higher in protein and fat, for what it’s worth—which is not a lot. As with most fruits, the protein and fat numbers are low importance next to the carb:fiber ratio.
When it comes to vitamins, pomegranate has more of vitamins B1, B2, B5, B6, B9. E. K, and choline. On the other hand, cherries have more of vitamins A and B3. The two fruits are equal in vitamin C. This all makes for a clear win for pomegranate.
In the category of minerals, pomegranate boasts more copper, magnesium, phosphorus, potassium, selenium, and zinc. In contrast, cherries have slightly more calcium. Another win for pomegranate.
Both of these fruits have beneficial polyphenols, each with a slightly different profile, but neither pressingly better than the other.
In short: as ever with healthy foods, enjoy both—diversity is good! But if you’re going to pick on, we recommend the pomegranate.
Want to learn more?
You might like to read:
- Pomegranate Peel’s Potent Potential ← so don’t throw it away!
- Cherries’ Very Healthy Wealth Of Benefits!
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: