8 Critical Signs Of Blood Clots That You Shouldn’t Ignore
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Blood clots can form as part of deep vein thrombosis or for other reasons; wherever they form (unless they are just doing their job healing a wound) they can cause problems. But how to know what’s going on inside our body?
Telltale signs
Our usual medical/legal disclaimer applies here, and we are not doctors, let alone your doctors, and even if we were we couldn’t diagnose from afar… But for educational purposes, here are the eight signs from the video:
- Swelling: especially if only on one leg (assuming you have no injury to account for it), which may feel tight and uncomfortable
- Warmness: does the area warmer to the touch? This may be because of the body’s inflammatory response trying to deal with a blood clot
- Tenderness: again, caused by the inflammation in response to the clot
- Discolored skin: it could be reddish, or bruise-like. This could be patchy or spread over a larger area, because of a clot blocking the flow of blood
- Shortness of breath: if a clot makes it to the lungs, it can cause extra problems there (pulmonary embolism), and shortness of breath is the first sign of this
- Coughing up blood: less common than the above but a much more serious sign; get thee to a hospital
- Chest pain: a sharp or stabbing pain, in particular. The pain may worsen with deep breaths or coughing. Again, seek medical attention.
For more on recognizing these signs (including helpful visuals), and more on what to do about them and how to avoid them in the first place, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Further reading
You might like to read:
Dietary Changes for Artery Health
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Spiced Fruit & Nut Chutney
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
‘Tis the season to make the chutney that will then be aged chutney when you want it later! And unlike supermarket varieties with their ingredients list that goes “Sugar, spirit vinegar, inverted glucose-fructose syrup,” this one has an array of health-giving fruits and nuts (just omit the nuts if you or someone you may want to give this to has an allergy), and really nothing bad in here at all. And of course, tasty healthful spices!
You will need
- 2 red onions, chopped
- 1½ cups dried apricots, chopped
- 1½ cups dried figs, chopped
- 1 cup raisins
- ½ cup apple cider vinegar
- ½ cup slivered almonds
- ½ lime, chopped and deseeded
- ¼ bulb garlic, chopped
- 1 hot pepper, chopped (your choice what kind; omit if you don’t like heat at all; multiply if you want more heat)
- 2 tablespoons honey or maple syrup (omit for a less sweet chutney; there is sweetness in the dried fruits already, after all)
- 1 tbsp freshly grated ginger
- 2 tsp sweet cinnamon
- 1 tsp nutmeg
- 1 tsp black pepper
- ½ teaspoon allspice
- ½ MSG or 1 tsp low-sodium salt
- Extra virgin olive oil
Method
(we suggest you read everything at least once before doing anything)
1) Heat some oil in a heavy-based pan that will be large enough for all ingredients to go into eventually. Fry the onions on a gentle heat for around 15 minutes. We don’t need to caramelize them yet (this will happen with time), but we do want them soft and sweet already.
2) Add the ginger, garlic, and chili, and stir in well.
3) When the onions start to brown, add the fruit and stir well to mix thoroughly.
4) Add the honey or maple syrup (if using), and the vinegar; add the remaining spices/seasonings, so everything is in there now except the almonds.
5) Cook gently for another 30 minutes while stirring. At some point it’ll become thick and sticky; add a little water as necessary. You don’t want to drown it, but you do want it to stay moist. It’ll probably take only a few tablespoons of added water in total, but add them one at a time and stir in before judging whether more is needed. By the end of the 30 minutes, it should be more solid, to the point it can stand up by itself.
6) Add the almonds, stir to combine, and leave to cool. Put it in jars until you need it (or perhaps give it as gifts).
Alternative method: if you don’t want to be standing at a stove stirring for about an hour in total, you can use a slow cooker / crock pot instead. Put the same ingredients in the same order, but don’t stir them, just leave them in layers (this is because of the pattern of heat distribution; it’ll be hotter at the bottom, so the things that need to be more cooked should be there, and the design means they won’t burn) for about two hours, then stir well to mix thoroughly, and leave it for another hour or two, before turning it off to let it cool. Put it in jars until you need it (or perhaps give it as gifts).
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Top 8 Fruits That Prevent & Kill Cancer ← figs and apricots appear here
- Apricots vs Peaches – Which is Healthier? ← have a guess
- Almonds vs Walnuts – Which is Healthier? ← almonds won, but walnuts were close and would also work in this recipe
- Pistachios vs Almonds – Which is Healthier? ← almonds won, but pistachios were close and would also work in this recipe
- Our Top 5 Spices: How Much Is Enough For Benefits? ← we scored 4/5 today!
Take care!
Share This Post
-
The Blood Sugar Solution – by Dr. Mark Hyman
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The main purpose of this book is combating metabolic disease, the amalgam of what’s often prediabetes (sometimes fully-fledged diabetes) and cardiovascular disease (sometimes fully-fledged heart disease).
To achieve this (after an introductory section explaining what the sociomedical problems are and why the sociomedical problems are happening), he offers a seven-step program; we’ll not keep those steps a mystery; they are:
- Boost your nutrition
- Regulate your hormones
- Reduce inflammation
- Improve your digestion
- Maximize detoxification
- Enhance energy metabolism
- Soothe your mind
Thereafter, it’s all about leading the reader by the hand through the steps; he also offers a six-week action plan, and a six-week meal plan with recipes.
The style is very sensationalist (too sensationalist for this reviewer’s personal taste) but nevertheless backed up with hard science when it comes to hard claims. So, if you don’t mind wading through (or skipping) some early chapters that are a bit “used car salesman” in feel, there’s actually a lot of good information, especially in the middle of the book, and useful practical guides in the middle and end.
Bottom line: if you want a good comprehensive science-based practical guide to addressing the risk of metabolic disease, this is that.
Click here to check out The Blood Sugar Solution, and look after yours!
Share This Post
-
Millet vs Buckwheat – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing millet to buckwheat, we picked the buckwheat.
Why?
Both of these naturally gluten-free grains* have their merits, but we say buckwheat comes out on top for most people (we’ll discuss the exception later).
*actually buckwheat is a flowering pseudocereal, but in culinary terms, we’ll call it a grain, much like we call tomato a vegetable.
Considering the macros first of all, millet has slightly more carbs while buckwheat has more than 2x the fiber. An easy win for buckwheat (they’re about equal on protein, by the way).
In the category of vitamins, millet has more of vitamins B1, B2, B3, B6, and B9, while buckwheat has more of vitamins B5, E, K, and choline. Superficially that’s a 5:4 win for millet, though buckwheat’s margins of difference are notably greater, so the overall vitamin coverage could arguably be considered a tie.
When it comes to minerals, millet has more phosphorus and zinc, while buckwheat has more calcium, copper, iron, magnesium, manganese, potassium, and selenium. For most of them, buckwheat’s margins of difference are again greater. An easy win for buckwheat, in any case.
This all adds up to a clear win for buckwheat, but as promised, there is an exception: if you have issues with your kidneys that mean you are avoiding oxalates, then millet becomes the healthier choice, as buckwheat is rather high in oxalates while millet is low in same.
For everyone else: enjoy both! Diversity is good. But if you’re going to pick one, buckwheat’s the winner.
Want to learn more?
You might like to read:
Grains: Bread Of Life, Or Cereal Killer?
Take care!
Share This Post
Related Posts
-
When Doctors Make House Calls, Modern-Style!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
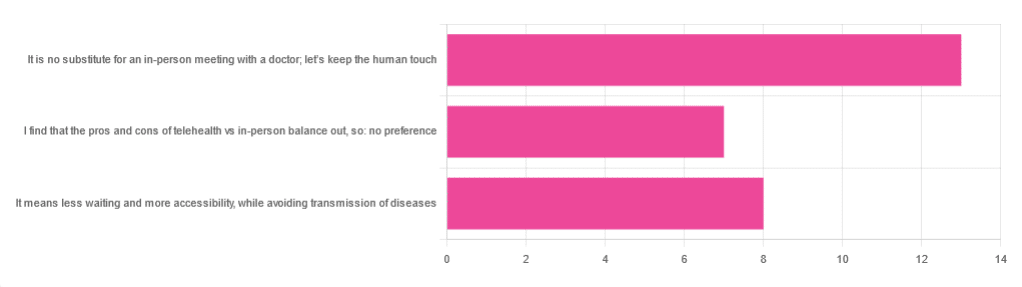
In Tuesday’s newsletter, we asked you foryour opinion of telehealth for primary care consultations*, and got the above-depicted, below-described, set of responses:
- About 46% said “It is no substitute for an in-person meeting with a doctor; let’s keep the human touch”
- About 29% said “It means less waiting and more accessibility, while avoiding transmission of diseases”
- And 25 % said “I find that the pros and cons of telehealth vs in-person balance out, so: no preference”
*We specified that by “primary care” we mean the initial consultation with a non-specialist doctor, before receiving treatment or being referred to a specialist. By “telehealth” we mean by videocall or phonecall.
So, what does the science say?
A quick note first
Because telehealth was barely a thing (statistically speaking) before the first stages of the COVID pandemic, compared to how it is now, most of the science for this is young, and a lot of the science simply hasn’t been done yet, and/or has not been published yet, because the process can take years.
Because of this, some studies we do have aren’t specifically about primary care, and are sometimes about specialists. We think this should not affect the results much, but it bears highlighting.
Nevertheless, we’ll do what we can with the science we have!
Telehealth is more accessible than in-person consultations: True or False?
True, for most people. For example…
❝Data was found from a variety of emergency and non-emergency departments of primary, secondary, and specialised healthcare.
Satisfaction was high among recipients of healthcare, scoring 9-10 on a scale of 0-10 or ranging from 73.3% to 100%.
Convenience was rated high in every specialty examined. Satisfaction of clinicians was high throughout the specialities despite connection failure and concerns about confidentiality of information.❞
whereas…
❝Nonetheless, studies reported perception of increased barriers to accessing care and inequalities for vulnerable patients especially in older people❞
~ Ibid.
Source: Satisfaction with telemedicine use during COVID-19 pandemic in the UK: a systematic review
Now, perception of those things does necessarily equate to an actual increased barrier, but it is reasonable that someone who thinks something is inaccessible will be less inclined to try to access it.
The quality of care provided via telehealth is as good as in-person: True or False?
True, ostensibly, with caveats. The caveats are:
- We’re going offreported patient satisfaction, not objective patient health outcomes (we found little* science as yet for the relative incidence of misdiagnosis, for example—which kind of thing will take time to be revealed).
- We’re also therefore speaking (as statistics do) for the significant majority of people. However, if we happen to be (statistically speaking) an insignificant minority, well, that just sucks for us personally.
*we did find some, but it wasn’t very helpful yet. For example:
An electronic trigger to detect telemedicine-related diagnostic errors
this one does look at the incidence of diagnostic errors, but provides no control group (i.e. otherwise-comparable in-person consultations) for comparison.
While most oft-considered demographic groups reported comparable patient satisfaction (per race, gender, and socioeconomic status, for example), there was one outlier variable, which was age (as we quoted from that first study above).
However!
Looking under the hood of these stats, it seems that age is not the real culprit, so much as technological illiteracy, which is heavily correlated with age:
❝Lower eHealth literacy is associated with more negative attitudes towards I/C technology in healthcare. This trend is consistent across diverse demographics and regions. ❞
Source: Meta-analysis: eHealth literacy and attitudes towards internet/computer technology
There are things that can be done at an in-person consultation that can’t be done by telehealth: True or False?
True, of course. It is incredibly rare that we will cite “common sense”, (as sometimes “common sense” is actually “common mistakes” and is simply and verifiably wrong), but in this case, as one 10almonds subscriber put it:
❝The doctor uses his five senses to assess. This cannot be attained over the phone❞
~ 10almonds subscriber
A quick note first: if your doctor is using their sense of taste to diagnose you, please get a different doctor, because they should definitely not be doing that!
Not in this century, anyway… Once upon a time, diabetes was diagnosed by urine-tasting (and yes, that was a fairly reliable method).
However, nowadays indeed a doctor will use sight, sound, touch, and sometimes even smell.
In a videocall we’re down to two of those senses (sight and sound), and in a phonecall, down to one (sound) and even that is hampered. Your doctor cannot, for example, use a stethoscope over the phone.
With this in mind, it really comes down to what you need from your doctor in that consultation.
- If you’re 99% sure that what you need is to be prescribed an antidepressant, that probably doesn’t need a full physical.
- If you’re 99% sure that what you need is a referral, chances are that’ll be fine by telehealth too.
- If your doctor is 99% sure that what you need is a verbal check-up (e.g. “How’s it been going for you, with the medication that I prescribed for you a month ago?”, then again, a call is probably fine.
If you have a worrying lump, or an unhappy bodily discharge, or an unexplained mysterious pain? These things, more likely an in-person check-up is in order.
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Almonds vs Peanuts – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing almonds to peanuts, we picked the almonds.
Why?
No, it’s not just our pro-almonds bias… But it’s also not as one-sided, nutritionally speaking, as you might think!
In terms of macros, almonds have a lot more fiber, and moderately more carbs, the ratio of which give almonds the lower glycemic index. On the other hand, peanuts have a little more protein. Both of these nuts are equally fatty, but peanuts have the higher saturated fat content. All in all, we say the biggest deciding factor is the fiber, and hand this one to the almonds.
In the category of vitamins, almonds have more of vitamins B2 and E, while peanuts have more of vitamins B1, B3, B5, B6, B7, and B9. An easy win for peanuts this time.
When it comes to minerals, almonds have more calcium, magnesium, manganese, phosphorus, and potassium, while peanuts have more copper, iron, selenium, and zinc. Thus, a 5:4 marginal win for almonds.
Adding up the sections makes for an overall win for almonds, but as you can see, it was close and peanuts certainly have their merits too, so by all means enjoy either or both; diversity is good!
Unless you are allergic, in which case, obviously please don’t do that.
Want to learn more?
You might like to read:
Why You Should Diversify Your Nuts!
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Forks Over Knives: Flavor! – by Darshana Thacker
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s important to not have to choose too much between health and flavor, because the outcome will never be a good one, either for your health or your happiness. And what’s bad for your happiness will ultimately not work out and thus will be bad for your general health, so, the question becomes: how to get both?
This book handles that nicely, delivering plant-based dishes that are also incidentally oil-free, and also either gluten-free or else there’s an obvious easy substitution to make it such. The flavor here comes from the ingredients as a whole, including the main ingredients as well as seasonings.
On the downside, occasionally those ingredients may be a little obscure if you don’t live in, say, San Francisco, and the ingredients weren’t necessarily chosen for cooking on a budget, either.
However, in most cases for most people it will, at worse, inspire you to try using an ingredient you don’t usually use—so that’s a good result.
The recipes are very clear and easy to follow, although not all are illustrated, and the “ready in…” times are about as accurate as they are for any cookbook, that is to say, it’s the time in which it conceivably can be done if (like the author, a head chef) you have a team of sous-chefs who have done a bunch of prep for you (e.g. sweet potato does not normally come in ½” dice; it comes in sweet potatoes) and laid everything out in little bowls mise-en-place style, and also you know the procedure well enough to not have to stop, hesitate, check anything, wash anything, wait for water to boil or anything else to heat up, or so forth. In other words, if you’re on your own in your home kitchen with normal domestic appliances, it’s going to take a little longer than for a professional in a professional kitchen with professional help.
But don’t let that detract from the honestly very good recipes.
Bottom line: if you’d like to level-up your plant-based cooking, this will definitely make your dishes that bit better!
Click here to check out Forks Over Knives: Flavor!, and dig in!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: