7 Minutes, 30 Days, Honest Review: How Does The 7-Minute Workout Stack Up?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
For those who don’t like exercising, “the 7-minute workout” (developed by exercise scientists Chris Jordan and Bret Klika) has a lot of allure. After all, it’s just 7 minutes and then you’re done! But how well does it stand up, outside of the lab?
Down-to-Earth
Business Insider’s Kelly Reilly is not a health guru, and here he reviews the workout for us, so that we can get a real view of what it’s really like in the real world. What does he want us to know?
- It’s basically an optimized kind of circuit training, and can be done with no equipment aside from a floor, a wall, and a chair
- It’s one exercise for 30 seconds, then 10 seconds rest, then onto the next exercise
- He found it a lot easier to find the motivation to do this, than go to the gym. After all “it’s just 7 minutes” is less offputting than getting in the car, driving someplace, using public facilities, driving back, etc. Instead, it’s just him in the comfort of his home
- The exercise did make him sweat and felt like a “real” workout in that regard
- He didn’t like missing out on training his biceps, though, since there are no pulling movements
- He lost a little weight over the course of the month, though that wasn’t his main goal (and indeed, he was not eating healthily)
- He did feel better each day after working out, and at the end of the month, he enjoyed feeling self-confident in a tux that now fitted him better than it did before
For more details, his own words, and down-to-earth visuals of what this looked like for him, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Further reading
Want to know more? Check out…
- How To Do HIIT (Without Wrecking Your Body)
- HIIT, But Make It HIRT ← this is about high-intensity resistance training!
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Lose Weight (Healthily!)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What Do You Have To Lose?
For something that’s a very commonly sought-after thing, we’ve not yet done a main feature specifically about how to lose weight, so we’re going to do that today, and make it part of a three-part series about changing one’s weight:
- Losing weight (specifically, losing fat)
- Gaining weight (specifically, gaining muscle)
- Gaining weight (specifically, gaining fat)
And yes, that last one is something that some people want/need to do (healthily!), and want/need help with that.
There will be, however, no need for a “losing muscle” article, because (even though sometimes a person might have some reason to want to do this), it’s really just a case of “those things we said for gaining muscle? Don’t do those and the muscle will atrophy naturally”.
One reason we’ve not covered this before is because the association between weight loss and good health is not nearly so strong as the weight loss industry would have you believe:
And, while BMI is not a useful measure of health in general, it’s worth noting that over the age of 65, a BMI of 27 (which is in the high end of “overweight”, without being obese) is associated with the lowest all-cause mortality:
BMI and all-cause mortality in older adults: a meta-analysis
Important: the above does mean that for very many of our readers, weight loss would not actually be healthy.
Today’s article is intended as a guide only for those who are sure that weight loss is the correct path forward. If in doubt, please talk to your doctor.
With that in mind…
Start in the kitchen
You will not be able to exercise well if your body is malnourished.
Counterintuitively, malnourishment and obesity often go hand-in-hand, partly for this reason.
Important: it’s not the calories in your food; it’s the food in your calories
See also: Mythbusting Calories
The kind of diet that most readily produces unhealthy overweight, the diet that nutritional scientists often call the “Standard American Diet”, or “SAD” for short, is high on calories but low on nutrients.
So you will want to flip this, and focus on enjoying nutrient-dense whole foods.
The Mediterranean Diet is the current “gold standard” in this regard, so for your interest we offer:
Four Ways To Upgrade The Mediterranean Diet
And since you may be wondering:
Should You Go Light Or Heavy On Carbs?
The dining room is the next most important place
Many people do not appreciate food enough for good health. The trick here is, having prepared a nice meal, to actually take the time to enjoy it.
It can be tempting when hungry (or just plain busy) to want to wolf down dinner in 47 seconds, but that is the metabolic equivalent of “oh no, our campfire needs more fuel, let’s spray it with a gallon of gasoline”.
To counter this, here’s the very good advice of Dr. Rupy Aujla, “The Kitchen Doctor”:
Interoception & Mindful Eating
The bedroom is important too
You snooze, you lose… Visceral belly fat, anyway! We’ve talked before about how waist circumference is a better indicator of metabolic health than BMI, and in our article about trimming that down, we covered how good sleep is critical for one’s waistline:
Visceral Belly Fat & How To Lose It
Exercise, yes! But in one important way.
There are various types of exercise that are good for various kinds of health, but there’s only one type of exercise that is good for boosting one’s metabolism.
Whereas most kinds of exercise will raise one’s metabolism while exercising, and then lower it afterwards (to below its previous metabolic base rate!) to compensate, high-intensity interval training (HIIT) will raise your metabolism while training, and for two hours afterwards:
…which means that unlike most kinds of exercise, HIIT actually works for fat loss:
So if you’d like to take up HIIT, here’s how:
How (And Why) To Do HIIT (Without Wrecking Your Body)
Want more?
Check out our previous article about specifically how to…
Burn! How To Boost Your Metabolism
Take care!
Share This Post
-
Creamy Zucchini, Edamame, & Asparagus Linguine
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Protein, fiber, and polyphenols are the dish of the day here:
You will need
- 1½ cups milk (your choice what kind; we recommend soy for its neutral taste, though hazelnut’s nutty flavor would also work in this recipe)
- 6 oz wholegrain linguine (or your pasta of choice)
- 2 zucchini, thinly sliced
- 5 oz edamame beans (frozen is fine)
- 5 oz asparagus tips, cut into 2″ lengths
- ½ bulb garlic, crushed
- 1 tbsp chia seeds
- 1 small handful arugula
- 1 small handful parsley, chopped
- A few mint leaves, chopped
- Juice of ½ lemon
- 2 tsp black pepper, coarse ground
- ½ tsp MSG or 1 tsp low-sodium salt
- Extra virgin olive oil
Method
(we suggest you read everything at least once before doing anything)
1) Heat some oil in a sauté pan or similar, over a low to medium heat. Add the zucchini and cook for 5 minutes until they start to soften.
2) Add the garlic and continue cooking for 1 minute, stirring gently.
3) Add the milk, bring to the boil, and add the past, chia seeds (the resistant starch from the pasta will help thicken the sauce, as will the chia seeds), and MSG or salt.
4) Reduce the heat, cover, and simmer for 8 minutes.
5) Add the edamame beans and asparagus, and cook for a further 2 minutes, or until the pasta is cooked but still firm to the bite. The sauce should be quite thick now.
6) Stir in the remaining ingredients and serve, adding a garnish if you wish.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- The Many Health Benefits Of Garlic
- Black Pepper’s Impressive Anti-Cancer Arsenal (And More)
- If You’re Not Taking Chia, You’re Missing Out
Take care!
Share This Post
-
I’m Moving Forward and Facing the Uncertainty of Aging
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It takes a lot of courage to grow old.
I’ve come to appreciate this after conversations with hundreds of older adults over the past eight years for nearly 200 “Navigating Aging” columns.
Time and again, people have described what it’s like to let go of certainties they once lived with and adjust to new circumstances.
These older adults’ lives are filled with change. They don’t know what the future holds except that the end is nearer than it’s ever been.
And yet, they find ways to adapt. To move forward. To find meaning in their lives. And I find myself resolving to follow this path as I ready myself for retirement.
Patricia Estess, 85, of the Brooklyn borough of New York City spoke eloquently about the unpredictability of later life when I reached out to her as I reported a series of columns on older adults who live alone, sometimes known as “solo agers.”
Estess had taken a course on solo aging. “You realize that other people are in the same boat as you are,” she said when I asked what she had learned. “We’re all dealing with uncertainty.”
Consider the questions that older adults — whether living with others or by themselves — deal with year in and out: Will my bones break? Will my thinking skills and memory endure? Will I be able to make it up the stairs of my home, where I’m trying to age in place?
Will beloved friends and family members remain an ongoing source of support? If not, who will be around to provide help when it’s needed?
Will I have enough money to support a long and healthy life, if that’s in the cards? Will community and government resources be available, if needed?
It takes courage to face these uncertainties and advance into the unknown with a measure of equanimity.
“It’s a question of attitude,” Estess told me. “I have honed an attitude of: ‘I am getting older. Things will happen. I will do what I can to plan in advance. I will be more careful. But I will deal with things as they come up.’”
For many people, becoming old alters their sense of identity. They feel like strangers to themselves. Their bodies and minds aren’t working as they used to. They don’t feel the sense of control they once felt.
That requires a different type of courage — the courage to embrace and accept their older selves.
Marna Clarke, a photographer, spent more than a dozen years documenting her changing body and her life with her partner as they grew older. Along the way, she learned to view aging with new eyes.
“Now, I think there’s a beauty that comes out of people when they accept who they are,” she told me in 2022, when she was 70, just before her 93-year-old husband died.
Arthur Kleinman, a Harvard professor who’s now 83, gained a deeper sense of soulfulness after caring for his beloved wife, who had dementia and eventually died, leaving him grief-stricken.
“We endure, we learn how to endure, how to keep going. We’re marked, we’re injured, we’re wounded. We’re changed, in my case for the better,” he told me when I interviewed him in 2019. He was referring to a newfound sense of vulnerability and empathy he gained as a caregiver.
Herbert Brown, 68, who lives in one of Chicago’s poorest neighborhoods, was philosophical when I met him at his apartment building’s annual barbecue in June.
“I was a very wild person in my youth. I’m surprised I’ve lived this long,” he said. “I never planned on being a senior. I thought I’d die before that happened.”
Truthfully, no one is ever prepared to grow old, including me. (I’m turning 70 in February.)
Chalk it up to denial or the limits of imagination. As May Sarton, a writer who thought deeply about aging, put it so well: Old age is “a foreign country with an unknown language.” I, along with all my similarly aged friends, are surprised we’ve arrived at this destination.
For me, 2025 is a turning point. I’m retiring after four decades as a journalist. Most of that time, I’ve written about our nation’s enormously complex health care system. For the past eight years, I’ve focused on the unprecedented growth of the older population — the most significant demographic trend of our time — and its many implications.
In some ways, I’m ready for the challenges that lie ahead. In many ways, I’m not.
The biggest unknown is what will happen to my vision. I have moderate macular degeneration in both eyes. Last year, I lost central vision in my right eye. How long will my left eye pick up the slack? What will happen when that eye deteriorates?
Like many people, I’m hoping scientific advances outpace the progression of my condition. But I’m not counting on it. Realistically, I have to plan for a future in which I might become partially blind.
It’ll take courage to deal with that.
Then, there’s the matter of my four-story Denver house, where I’ve lived for 33 years. Climbing the stairs has helped keep me in shape. But that won’t be possible if my vision becomes worse.
So my husband and I are taking a leap into the unknown. We’re renovating the house, installing an elevator, and inviting our son, daughter-in-law, and grandson to move in with us. Going intergenerational. Giving up privacy. In exchange, we hope our home will be full of mutual assistance and love.
There are no guarantees this will work. But we’re giving it a shot.
Without all the conversations I’ve had over all these years, I might not have been up for it. But I’ve come to see that “no guarantees” isn’t a reason to dig in my heels and resist change.
Thank you to everyone who has taken time to share your experiences and insights about aging. Thank you for your openness, honesty, and courage. These conversations will become even more important in the years ahead, as baby boomers like me make their way through their 70s, 80s, and beyond. May the conversations continue.
USE OUR CONTENT
This story can be republished for free (details).
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
This article first appeared on KFF Health News and is republished here under a Creative Commons license.
Share This Post
Related Posts
-
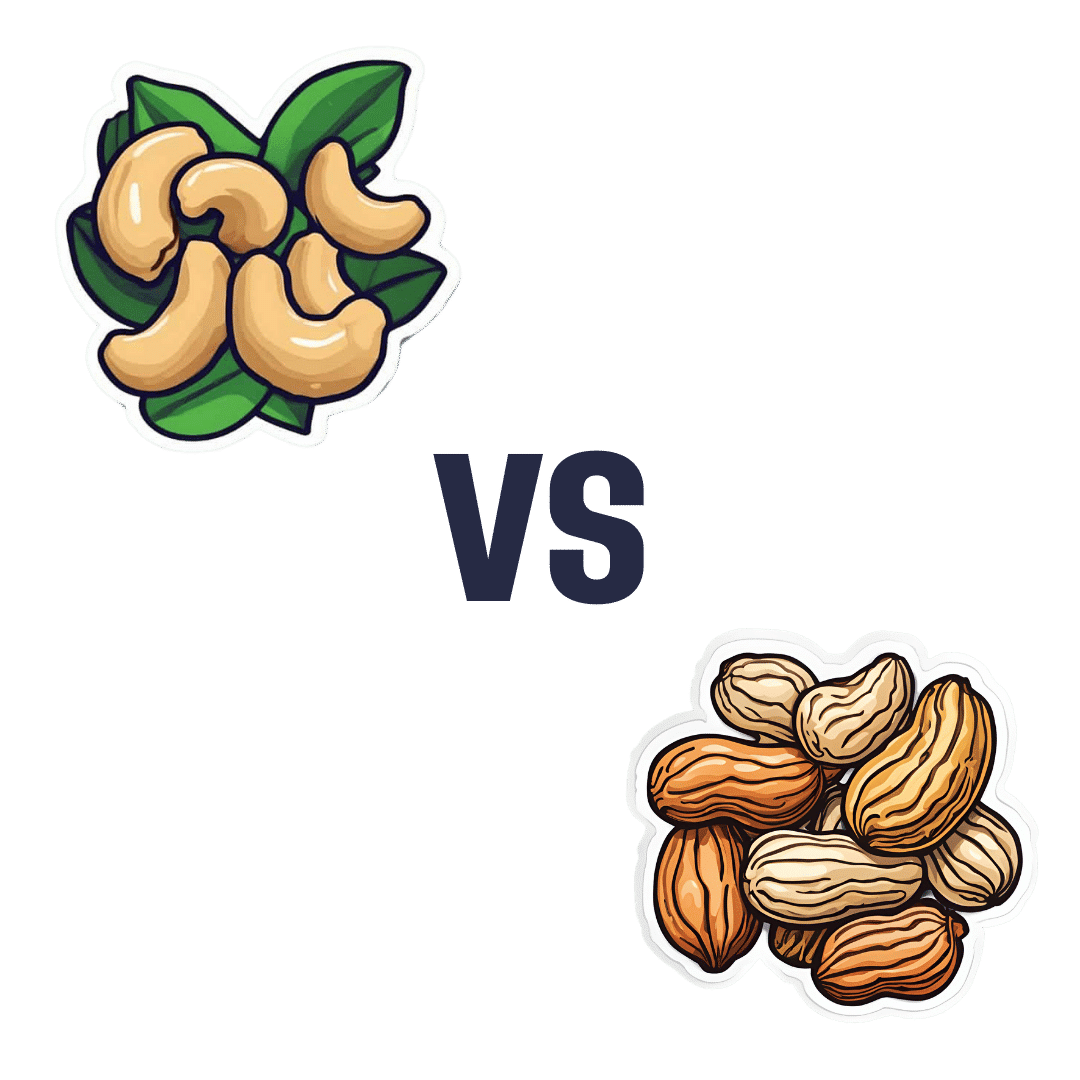
Cashews vs Peanuts – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing cashews to peanuts, we picked the peanuts.
Why?
Another one for “that which is more expensive is not necessarily the healthier”! Although, certainly both are good:
In terms of macros, cashews have about 2x the carbs while peanuts have a little more (healthy!) fat and more than 2x the fiber, meaning that peanuts also enjoy the lower glycemic index. All in all, a fair win for peanuts here.
When it comes to vitamins, cashews have more of vitamins B6 and K, while peanuts have a lot more of vitamins B1, B2, B3, B5, B7, B9, and E. Another easy win for peanuts.
In the category of minerals; cashews have more copper, iron, magnesium, phosphorus, and selenium, while peanuts have more calcium, manganese, and potassium. A win for cashews, this time.
Adding up the sections makes for an overall win for peanuts, but (assuming you are not allergic) enjoy either or both! In fact, enjoying both is best; diversity is good.
Want to learn more?
You might like to read:
Why You Should Diversify Your Nuts!
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
What Nobody Teaches You About Strengthening Your Knees
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Strengthening unhappy knees can seem difficult, because many obvious exercises like squats may hurt, and can feel like they are doing harm (and if your knees are bad enough, maybe they are; it depends on many factors). Here’s a way to improve things:
The muscle nobody talks about
Well, not nobody. But, it’s a muscle that’s rarely talked about; namely, the tibialis anterior.
It plays a key role in decelerating knee motion—in other words, the movement that hurts if you have bad knees. It’s essential for absorbing shock during activities like walking, climbing stairs, and stepping off curbs
So, of course, strengthening this muscle supports knee health.
The exercise this video recommends for strengthening it involves leaning against a wall with feet about a foot away (closer feet make it easier, further makes it harder). Note, this is a lean, not a “Roman chair”.
The exercise involves squeezing the quadriceps, lifting toes toward the nose, and engaging the tibialis anterior muscle. If you’re wondering what to do with your hands, they can be held out with palms open to work on posture, or hanging by the sides. Do this for about 1½–2 minutes.
For more on all this, plus a visual demonstration, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
When Bad Joints Stop You From Exercising (5 Things To Change)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Planning Festivities Your Body Won’t Regret
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Festive Dilemma
For many, Christmas is approaching. Other holidays abound too, and even for the non-observant, it’d be hard to escape seasonal jollities entirely.
So, what’s the plan?
- Eat, drink, and be merry, and have New Year’s Resolutions for the first few days of January before collapsing in a heap?
- Approach the Yuletide with Spartan abstemiousness and miss all the fun while simultaneously annoying your relatives?
Let’s try to find a third approach instead…
What’s festive and healthy?
We’re doing this article this week, because many people will be shopping already, making plans, and so forth. So here are some things to bear in mind:
Make your own mindful choices
Coca-Cola company really did a number on Christmas, but it doesn’t mean their product is truly integral to the season. Same goes for many other things that flood the stores around this time of year. So much sugary confectionary! But remember, they’re not the boss of you. If you wouldn’t buy it ordinarily, why are you buying it now? Do you actually even want it?
If you really do, then you do you, but mindful choices will invariably be healthier than “because there were three additional aisles of confectionary now so I stopped and looked and picked some things”.
Pick your battles
If you’re having a big family gathering, likely there will be occasions with few healthy options available. But you can decide what’s most important for you to avoid, perhaps picking a theme, e.g:
- No alcohol this year, or
- No processed sugary foods, or
- Eat/drink whatever, but practice intermittent fasting
Some resources:
Fight inflammation
This is a big one so it deserves its own category. In the season of sugar and alcohol and fatty meat, inflammation can be a big problem to come around and bite us in the behind. We’ve written on this previously:
Positive dieting
In other words, less of a focus on what to exclude, and more of a focus on what to include in your diet. Fruity drinks and sweets are common at this time of year, but you know what’s also fruity? Fruit!
And it can be festive, too! Berries are great, and those tiny orange-like fruits that may be called clementines or tangerines or satsumas or, as Aldi would have it, “easy peelers”. Apple and cinnamon are also a great combination that both bring sweetness without needing added sugar.
And as for mains? Make your salads that bit fancier, get plenty of greens with your main, have hearty soups and strews with lentils and beams!
See also: Level-Up Your Fiber Intake! (Without Difficulty Or Discomfort)
Your gut will thank us later!
Get moving!
That doesn’t mean you have to beat the New Year rush to the gym (unless you want to!). But it could mean, for example, more time in your walking shoes (or dancing shoes! With a nod to today’s sponsor) and less time in the armchair.
See also: The doctor who wants us to exercise less; move more
Lastly…
Remember it’s supposed to be fun! And being healthy can be a lot more fun than suffering because of unfortunate choices that we come to regret.
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: