25 Healthy Habits That Will Change Your Life
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Cori Lefkowith, of “Redefining Strength” and “Strong At Every Age” fame, has compiled a list of the simple habits that make a big difference, and here they are!
The Tips
Her recommendations include…
- The healthy activities you’re most prone to skipping? Do those first
- Create staple meals… Consciously! This means: instead of getting into a rut of cooking the same few things in rotation because it’s what you have the ingredients in for, consciously and deliberately make a list of at least 7 meals that, between them, constitute a healthy balanced diet, and choose to make them your staples. That doesn’t mean don’t eat anything else (indeed, variety is good!) but having a robust collection of healthy staples to fall back on will help you avoid falling into unhealthy eating traps.
- Schedule time for healthy activities that you love. Instead of thinking “it would be nice to…”, actually figure out a timeslot, plan in advance, making it recurring, and do it!
- Have (healthy!) no-spoil food options always available. No-spoil doesn’t have to mean “won’t spoil ever”, but does mean at least that it has a long shelf-life. Nuts are a good example, assuming you’re not allergic. Sundried fruits are good too; not nearly as good as fresh fruit, but a lot better than some random processed snack because it’s what in. If you eat fish, then see if you can get dried fish in; it’s high in protein and keeps for a very long time indeed.
- Stock up on spices! Not only do they all have great health-giving properties (at least, we can’t think of a refutation by counterexample, Arrakis be damned), but also, they literally spice up our culinary repertoire, and bring joy to cooking and eating healthy food.
If you like these, check out the rest:
Click Here If The Embedded Video Doesn’t Load Automatically
Further reading
For more about actually making habits stick quickly and reliably,enjoy:
How To Really Pick Up (And Keep!) Those Habits
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Move – by Caroline Williams
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
- Get 150 minutes of moderate exercise per week, says the American Heart Association
- There are over 10,000 minutes per week, says the pocket calculator
Is 150/10,000 really the goal here? Really?
For Caroline Williams, the answer is no.
In this book that’s practically a manifesto, she outlines the case that:
- Humans evolved to move
- Industrialization and capitalism scuppered that
- We now spend far too long each day without movement
Furthermore, for Williams this isn’t just an anthropological observation, it’s a problem to be solved, because:
- Our lack of movement is crippling us—literally
- Our stagnation affects not just our bodies, but also our minds
- (again literally—there’s a direct correlation with mental health)
- We urgently need to fix this
So, what now, do we need to move in to the gym and become full-time athletes to clock up enough hours of movement? No.
Williams convincingly argues the case (using data from supercentenarian “blue zones” around the world) that even non-exertive movement is sufficient. In other words, you don’t have to be running; walking is great. You don’t have to be lifting weights; doing the housework or gardening will suffice.
From that foundational axiom, she calls on us to find ways to build our life around movement… rather than production-efficiency and/or convenience. She gives plenty of tips for such too!
Bottom line: some books are “I couldn’t put it down!” books. This one’s more of a “I got the urge to get up and get moving!” book.
Get your get-up-and-go up and going with “Move”—order yours from Amazon today!
Share This Post
-
10almonds Tells The Tea…
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Let’s Bust Some Myths!
It’s too late after puberty, hormones won’t change xyz
While yes, many adult trans people dearly wish they’d been able to medically transition before going through the “wrong” puberty, the truth is that a lot of changes will still occur later… even to “unchangeable” things like the skeleton.
The body is remaking itself throughout life, and hormones tell it how to do that. Some parts are just quicker or slower than others. Also: the skeleton is pulled-on constantly by our muscles, and in a battle of muscle vs bone, muscle will always win over time.
Examples of this include:
- trans men building bigger bones to support their bigger muscles
- trans women getting smaller, with wider hips and a pelvic tilt
Trans people have sporting advantages
Assuming at least a year’s cross-sex hormonal treatment, there is no useful advantage to being trans when engaging in a sport. There are small advantages and disadvantages (which goes for any person’s body, really). For example:
- Trans women will tend to be taller than cis women on average…
- …but that larger frame is now being powered by smaller muscles, because they shrink much quicker than the skeleton.
- Trans men taking T are the only athletes allowed to take testosterone…
- …but they will still often be smaller than their fellow male competitors, for example.
Read: Do Trans Women Athletes Have Advantages? (A rather balanced expert overview, which does also cover trans men)
There’s a trans population explosion; it’s a social contagion epidemic!
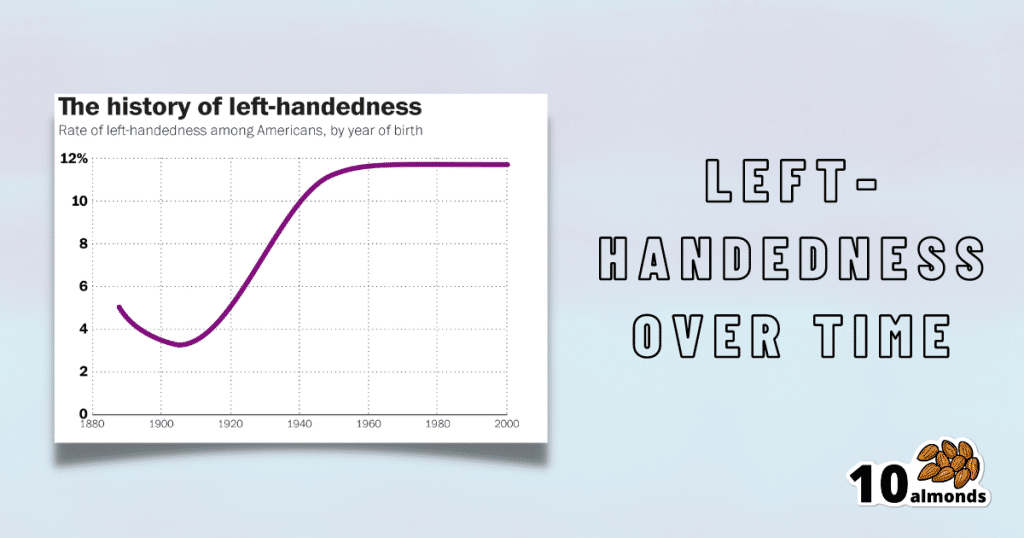
Source for figures: The Overall Rate Of Left-Handedness (Researchgate)
Left-handed people used to make up around 3% of the population… Until the 1920s, when that figure jumped sharply upwards, before plateauing at around 12% in around 1960, where it’s stayed since. What happened?! Simple, schools stopped forcing children to use their right hand.
Today, people ask for trans healthcare because they know it exists! Decades ago, it wasn’t such common knowledge.
The same explanation can be applied to other “population explosions” such as for autism and ADHD.
Fun fact: Mt. Everest was “discovered” in 1852, but scientists suspect it probably existed long before then! People whose ancestors were living on it long before 1852 also agree. Sometimes something exists for a long time, and only comes to wider public awareness later.
Transgender healthcare is too readily available, especially to children!
To believe some press outlets, you’d think:
- HRT is available from school vending machines,
- kids can get a walk-in top surgery at recess,
- and there’s an after-school sterilization club.
In reality, while availability varies from place to place, trans healthcare is heavily gatekept. Even adults have trouble getting it, often having to wait years and/or pay large sums of money… and get permission from a flock of doctors, psychologists, and the like. For those under the age of 18, it’s almost impossible in many places, even with parental support.
Puberty-blockers shouldn’t be given to teenagers, as the effects are irreversible
Quick question: who do you think should be given puberty-blockers? For whom do you think they were developed? Not adults, for sure! They were not developed for trans teens either, but for cis pre-teens with precocious puberty, to keep puberty at bay, to do it correctly later. Nobody argues they’re unsafe for much younger cis children, and only object when it’s trans teens.
They’re not only safe and reversible, but also self-reversing. Stop taking them, and the normally scheduled puberty promptly ensues by itself. For trans kids, the desired effect is to buy the kid time to make an informed and well-considered decision. After all, the effects of the wrong puberty are really difficult to undo!
A lot of people rush medical transition and regret it!
Trans people wish it could be rushed! It’s a lot harder to get gender-affirming care as a trans person, than it is to get the same (or comparable) care as a cis person. Yes, cis people get gender-affirming care, from hormones to surgeries, and have done for a long time.
As for regret… Medical transition has around a 1% regret rate. For comparison, hip replacement has a 4.8% regret rate and knee replacement has a 17.1% regret rate.
A medical procedure with a 99% success rate would generally be considered a miracle cure!
Share This Post
-
Wildfires ignite infection risks, by weakening the body’s immune defences and spreading bugs in smoke
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Over the past several days, the world has watched on in shock as wildfires have devastated large parts of Los Angeles.
Beyond the obvious destruction – to landscapes, homes, businesses and more – fires at this scale have far-reaching effects on communities. A number of these concern human health.
We know fire can harm directly, causing injuries and death. Tragically, the death toll in LA is now at least 24.
But wildfires, or bushfires, can also have indirect consequences for human health. In particular, they can promote the incidence and spread of a range of infections.
Effects on the immune system
Most people appreciate that fires can cause burns and smoke inhalation, both of which can be life-threatening in their own right.
What’s perhaps less well known is that both burns and smoke inhalation can cause acute and chronic changes in the immune system. This can leave those affected vulnerable to infections at the time of the injury, and for years to come.
Burns induce profound changes in the immune system. Some parts go into overdrive, becoming too reactive and leading to hyper-inflammation. In the immediate aftermath of serious burns, this can contribute to sepsis and organ failure.
Other parts of the immune system appear to be suppressed. Our ability to recognise and fight off bugs can be compromised after sustaining burns. Research shows people who have experienced serious burns have an increased risk of influenza, pneumonia and other types of respiratory infections for at least the first five years after injury compared to people who haven’t experienced burns.
Wildfire smoke is a complex mixture containing particulate matter, volatile organic compounds, ozone, toxic gases, and microbes. When people inhale smoke during wildfires, each of these elements can play a role in increasing inflammation in the airways, which can lead to increased susceptibility to respiratory infections and asthma.
Research published after Australia’s Black Summer of 2019–20 found a higher risk of COVID infections in areas of New South Wales where bushfires had occurred weeks earlier.
We need more research to understand the magnitude of these increased risks, how long they persist after exposure, and the mechanisms. But these effects are thought to be due to sustained changes to the immune response.
Microbes travel in smoky air
Another opportunity for infection arises from the fire-induced movement of microbes from niches they usually occupy in soils and plants in natural areas, into densely populated urban areas.
Recent evidence from forest fires in Utah shows microbes, such as bacteria and fungal spores, can be transported in smoke. These microbes are associated with particles from the source, such as burned vegetation and soil.
There are thousands of different species of microbes in smoke, many of which are not common in background, non-smoky air.
Only a small number of studies on this have been published so far, but researchers have shown the majority of microbes in smoke are still alive and remain alive in smoke long enough to colonise the places where they eventually land.
How far specific microbes can be transported remains an open question, but fungi associated with smoke particles have been detected hundreds of miles downwind from wildfires, even weeks after the fire.
So does this cause human infections?
A subset of these airborne microbes are known to cause infections in humans.
Scientists are probing records of human fungal infections in relation to wildfire smoke exposure. In particular, they’re looking at soil-borne infectious agents such as the fungi Coccidioides immitis and Coccidioides posadasii which thrive in dry soils that can be picked up in dust and smoke plumes.
These fungi cause valley fever, a lung infection with symptoms that can resemble the flu, across arid western parts of the United States.
A study of wildland firefighters in California showed high rates of valley fever infections, which spurred occupational health warnings including recommended use of respirators when in endemic regions.
A California-based study of the wider population showed a 20% increase in hospital admissions for valley fever following any amount of exposure to wildfire smoke.
However, another found only limited evidence of excess cases after smoke exposure in wildfire-adjacent populations in California’s San Joaquin Valley.
These contrasting results show more research is needed to evaluate the infectious potential of wildfire smoke from this and other fungal and bacterial causes.
Staying safe
Much remains to be learned about the links between wildfires and infections, and the multiple pathways by which wildfires can increase the risk of certain infections.
There’s also a risk people gathering together after a disaster like this, such as in potentially overcrowded shelters, can increase the transmission of infections. We’ve seen this happen after previous natural disasters.
Despite the gaps in our knowledge, public health responses to wildfires should encompass infection prevention (such as through the provision of effective masks) and surveillance to enable early detection and effective management of any outbreaks.
Christine Carson, Senior Research Fellow, School of Medicine, The University of Western Australia and Leda Kobziar, Professor of Wildland Fire Science, University of Idaho
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
The Green Roasting Tin – by Rukmini Iyer
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
You may be wondering: “do I really need a book to tell me to put some vegetables in a roasting tin and roast them?” and maybe not, but the book offers a lot more than that.
Indeed, the author notes “this book was slightly in danger of becoming the gratin and tart book, because I love both”, but don’t worry, most of the recipes are—as you might expect—very healthy.
As for formatting: the 75 recipes are divided first into vegan or vegetarian, and then into quick/medium/slow, in terms of how long they take.
However, even the “slow” recipes don’t actually take more effort, just, more time in the oven.
One of the greatest strengths of this book is that not only does it offer a wide selection of wholesome mains, but also, if you’re putting on a big spread, these can easily double up as high-class low-effort sides.
Bottom line: if you’d like to eat more vegetables in 2024 but want to make it delicious and with little effort, put this book on your Christmas list!
Click here to check out The Green Roasting Tin, and level-up yours!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Aging Minds: Normal vs Abnormal Cognitive Decline
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Having a “senior moment” and having dementia are things that are quite distinct from one another; while we may very reasonably intend to fight every part of it, it’s good to know what’s “normal” as well as what is starting to look like progress into something more severe:
Know the differences
Cognitive abilities naturally decline with age, often beginning around 30 (yes, really—the first changes are mostly metabolic though, so this is far from set in stone). Commonly-noticed changes include:
- slower thinking
- difficulty multitasking
- reduced attention
- weaker memory.
Over time, these changes have what is believed to be a two-way association (as in, each causes/worsens the other) with changes in brain structure, especially reduced hippocampal and frontal lobe volume.
- Gradual cognitive changes are normal with age, whereas dementia involves a pathological decline affecting memory, problem-solving, and behavior.
- Mild Cognitive Impairment (MCI) involves noticeable cognitive decline without disrupting daily life, while dementia affects everyday tasks like cooking or driving.
- Dementia causes significant impairments, including motor challenges like falls or tremors, and dementia-induced cognitive decline symptoms include forgetfulness, getting lost, personality changes, and planning difficulties, often worsening with stress or illness.
To best avoid these, consider: regular exercise, a nutritious diet, good quality sleep, social interaction, and mentally stimulating activities.
Also, often forgotten (in terms of its relevance at least): managing cardiovascular health is very important too. We’ve said it before, and we’ll say it again: what’s good for your heart is good for your brain (since the former feeds the latter with oxygen and nutrients, and also takes away detritus that will otherwise build up in the brain).
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Is It Dementia? Spot The Signs (Because None Of Us Are Immune) ← we go into more specific detail here
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
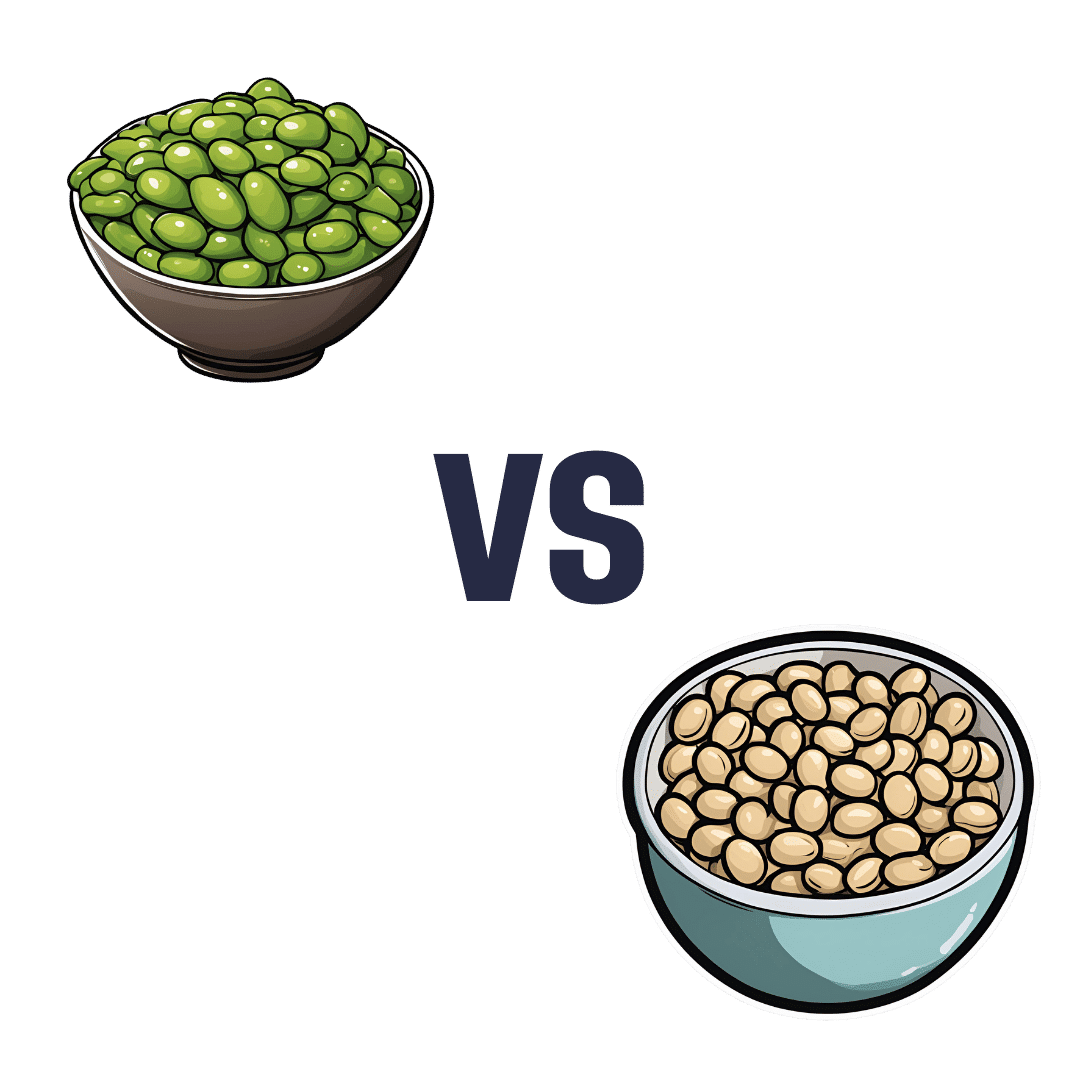
Edamame vs Soybeans – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing edamame to soybeans, we picked the soybeans.
Why?
You may be thinking: aren’t edamame soybeans? And yes, yes they are. But just like our many instances of pitting Brassica oleracea vs Brassica oleracea (one species, many cultivars e.g. broccoli, cauliflower, kale, cabbage, Brussels sprouts, etc), there are still differences. In this case, edamame and soybeans aren’t even different cultivars, what are conventionally called edamame are just the young beans of the plant, while what are conventionally called soybeans are the mature beans of the plant.
The main nutritional difference is: as they get older, they lose vitamins and gain minerals. More on that later. But first, “main difference” isn’t “only difference”, so…
In terms of macros, edamame have more carbs, while soybeans have a little more fiber and a lot more protein. An easy win for the mature soybeans.
In the category of vitamins, edamame have more of vitamins A, B1, B3, B5, B9, C, E, K, and choline, while soybeans have more of vitamins B2 and B6. A clear win for edamame, this time.
When it comes to minerals, the nutritional tables are turned, and edamame have more manganese and zinc, while soybeans have more calcium, copper, iron, magnesium, phosphorus, potassium, and selenium. An easy win for soybeans.
Adding up the sections makes for a two-to-one victory for soybeans, but by all means enjoy either or both; diversity is good!
Want to learn more?
You might like to read:
What’s Your Plant Diversity Score?
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: