12 Foods That Fight Depression & Anxiety
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Food impacts mental health, and while it won’t magically cure mental illness, dietary changes can do a lot to improve mood. Here’s how:
Nutraceuticals
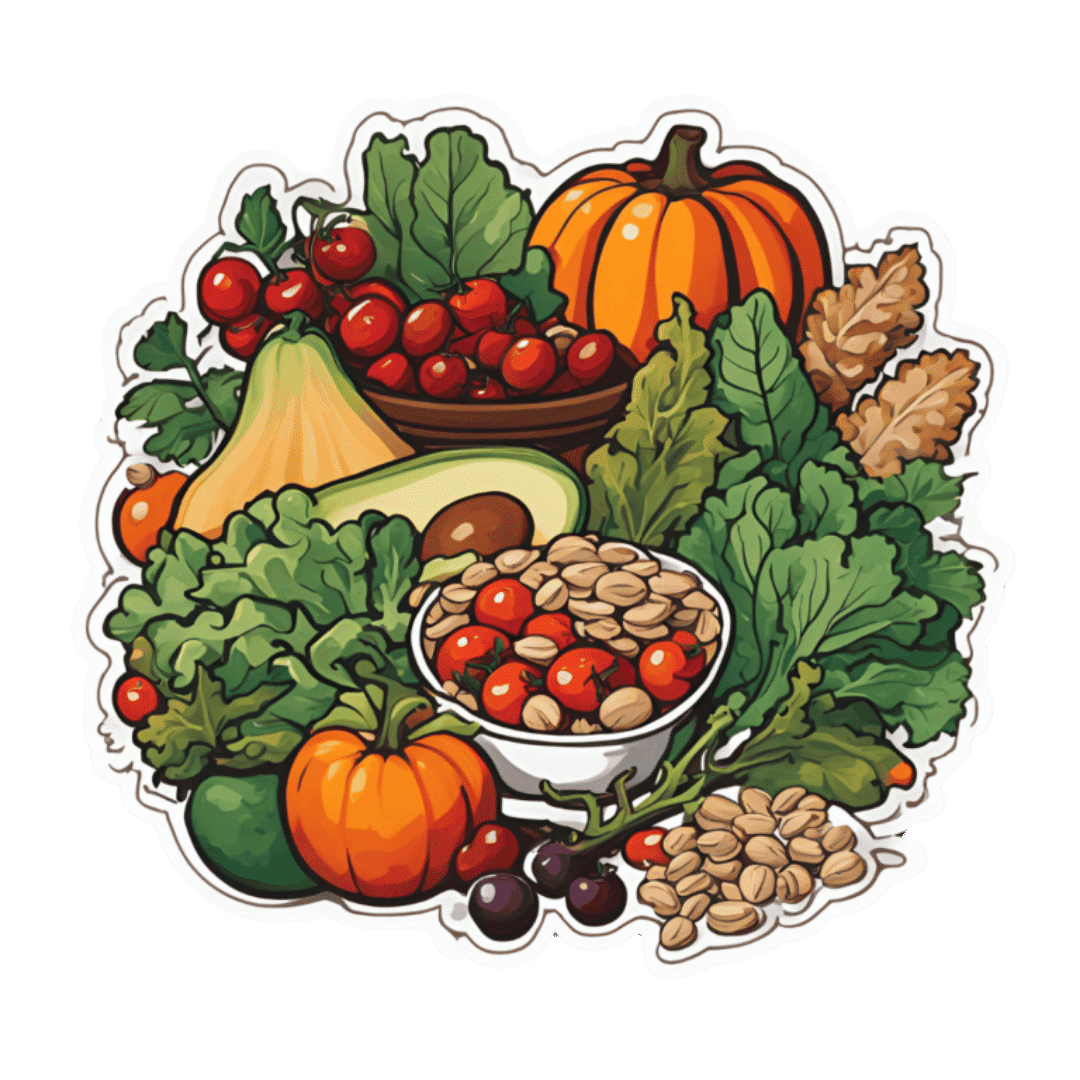
We’ll not keep the 12 nutraceutical foods a mystery; here’s what they are and a few words on how they work (in many cases, we could write whole articles about them; in some cases, we already have! You can find many of them by using the search function in the top-right of each page).
- Walnuts are rich in omega-3s for brain health; arguably the best nut for depression relief.
- Fermented foods because probiotics in foods like yogurt and sauerkraut support the gut-brain connection as well as serotonin production there, enhancing mood.
- Cherry tomatoes are rich in lycopene, which helps combat both depression and mood swings.
- Leafy greens reduce brain inflammation linked to depression.
- Apples and other fruit are high in fiber and antioxidants that stabilize blood sugar and mood, reducing brain inflammation.
- Beans are high in B vitamins, crucial for neurotransmitter production and mood regulation (without also being high in brain-harmful things, as red meat is).
- Berries are super-high antioxidants and cortisol-lowering anthocyanidins, promoting calmness and reducing stress.
- Oats contain the healthiest kind of fiber, β-glucan, and additionally help stabilize blood sugar and mood; they’re also rich in selenium, which boosts mood.
- Mushrooms help regulate blood sugar and act as prebiotics, supporting serotonin production in the gut.
- Avocados are famously rich in healthy fats, including omega-3s and oleic acid, which support brain health and combat depression.
- Dark chocolate contains antioxidants, magnesium, and gut-healthy prebiotics that indirectly reduce mental stress and improve brain function. Also a famous comfort food for many, of course, and that factor’s not to be overlooked either.
- Pumpkin seeds are rich in tryptophan, which boosts serotonin production. As a bonus, they also help some kinds of antidepressant to work better—check with your doctor or pharmacist to be sure in your case, though.
For more on all of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
The 6 Pillars Of Nutritional Psychiatry
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Strong Curves – by Bret Contreras & Kellie Davis
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The title (and subtitle) is, of course, an appeal to vanity. However, the first-listed author is well-known as “The Glute Guy”, and he takes this very seriously, not just for aesthetic reasons but also for practical reasons.
After all, when it comes to posture and stability, a lot rests on our hips, and hips, well, they rest on our butt and thighs. What’s more, the gluteus maximus is the largest muscle in the human body, so really, is it a good one to neglect? Probably not, and your lower back will definitely thank you for keeping your glutes in good order, too.
That said, while it’s a focal point, it’s not the be-all-and-end-all, and this book does cover the whole body.
The book takes the reader from “absolute beginner” to “could compete professionally”, with clearly-illustrated and well-described exercises. We also get a strong “crash course” in the relevant anatomy and physiology, and even a chapter on nutrition, which is a lot better than a lot of exercise books’ efforts in that regard.
For those who like short courses, this book has several progressive 12-week workout plans that take the reader from a very clear starting point to a very clear goal point.
Another strength of the book is that while a lot of exercises expect (and require) access to a gym, there are also whole sections of “at home / bodyweight” exercises, including 12-week workout plans for such, as described above.
Bottom line: there’s really nothing bad that this reviewer can find to say about this one—highly recommendable to any woman who wants to get strong while keeping a feminine look.
Click here to check out Strong Curves, and rebuild your body, your way!
PS: at first glance, the cover art looks like an AI model; it’s not; that’s the co-author Kellie Davis, who also serves as the model through the book’s many photographic illustrations.
Share This Post
-
Asparagus vs Edamame – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing asparagus to edamame, we picked the edamame.
Why?
Perhaps it’s a little unfair comparing a legume to a vegetable that’s not leguminous (given legumes’ high protein content), but these two vegetables often serve a similar culinary role, and there is more to nutrition than protein. That said…
In terms of macros, edamame has a lot more protein and fiber; it also has more carbs, but the ratio is such that edamame still has the lower glycemic index. Thus, the macros category is a win for edamame in all relevant aspects.
When it comes to vitamins, things are a little closer; asparagus has more of vitamins A, B3, and C, while edamame has more of vitamins B1, B2, B5, B6, and B9. All in all, a moderate win for edamame, unless we want to consider the much higher vitamin C content of asparagus as particularly more relevant.
In the category of minerals, asparagus boasts only more selenium (and more sodium, not that that’s a good thing for most people in industrialized countries), while edamame has more calcium, copper, iron, magnesium, manganese, phosphorus, potassium, and zinc. An easy win for edamame.
In short, enjoy both (unless you have a soy allergy, because edamame is young soy beans), but edamame is the more nutritionally dense by far.
Want to learn more?
You might like to read:
Take care!
Share This Post
-
Eye Drops: Safety & Alternatives
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝Before important business meetings my father used to use eye drops to add a “sparkle” to his eyes. I think that is a step too far, but what, short of eye drops, can we do to keep our eyes bright throughout the day?❞
Firstly, we’d indeed not recommend eye drops unless advised to do so by your doctor to treat a specific health condition:
- Infections from over-the-counter artificial tears
- Are my eye drops safe to use?
- More eye drops recalled due to infection danger
Those eye drops that “add sparkle” are often based on astringents such as witch hazel. This means that the capillaries in the eye undergo vasoconstriction, becoming much less visible and the eye thus appears much whiter and thus brighter.
There isn’t a way to do the same thing from the inside, as taking a vasoconstrictor will simply increase your general blood pressure, making the capillaries of your eyes more, rather than less, visible.
However, what you can do is…
- look after your general vasculature (cardiovascular health)
- in particular, reduce hypertension
- that includes limiting salt
- stay away from vasoconstrictors (including caffeine)
- reduce your resting cortisol levels
- that certainly also means reducing alcohol consumption
- maintain good hydration
Take care!
Share This Post
Related Posts
-
You could be stress eating these holidays – or eating your way to stress. 5 tips for the table
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The holiday season can be a time of joy, celebration, and indulgence in delicious foods and meals. However, for many, it can also be an emotional and stressful period.
This stress can manifest in our eating habits, leading to what is known as emotional or stress eating.
There are certain foods we tend to eat more of when we’re stressed, and these can affect our health. What’s more, our food choices can influence our stress levels and make us feel worse. Here’s how.
Dean Clarke/Shutterstock Why we might eat more when stressed
The human stress response is a complex signalling network across the body and brain. Our nervous system then responds to physical and psychological events to maintain our health. Our stress response – which can be subtle or trigger a fight-or-flight response – is essential and part of daily life.
The stress response increases production of the hormones cortisol and insulin and the release of glucose (blood sugars) and brain chemicals to meet demand. Eating when we experience stress is a normal behaviour to meet a spike in energy needs.
But sometimes our relationship with food becomes strained in response to different types of stress. We might attach shame or guilt to overeating. And anxiety or insecurity can mean some people under-eat in stressful times.
Over time, people can start to associate eating with negative emotions – such as anger, sadness, fear or worry. This link can create behavioural cycles of emotional eating. “Emotional eaters” may go on to develop altered brain responses to the sight or smell of food.
What stress eating can do to the body
Stress eating can include binge eating, grazing, eating late at night, eating quickly or eating past the feeling of fullness. It can also involve craving or eating foods we don’t normally choose. For example, stressed people often reach for ultra-processed foods. While eating these foods is not necessarily a sign of stress, having them can activate the reward system in our brain to alleviate stress and create a pattern.
Short-term stress eating, such as across the holiday period, can lead to symptoms such as acid reflux and poor sleep – particularly when combined with drinking alcohol.
In the longer term, stress eating can lead to weight gain and obesity, increasing the risks of cancer, heart diseases and diabetes.
While stress eating may help reduce stress in the moment, long-term stress eating is linked with an increase in depressive symptoms and poor mental health.
If you do over eat at a big gathering, don’t try and compensate by eating very little the next day. Peopleimage.com – Yuri A/Shutterstock What we eat can make us more or less stressed
The foods we choose can also influence our stress levels.
Diets high in refined carbohydrates and sugar (such as sugary drinks, sweets, crackers, cakes and most chocolates) can make blood sugar levels spike and then crash.
Diets high in unhealthy saturated and trans fats (processed foods, animal fats and commercially fried foods) can increase inflammatory responses.
Rapid changes in blood sugar and inflammation can increase anxiety and can change our mood.
Meanwhile, certain foods can improve the balance of neurotransmitters in the brain that regulate stress and mood.
Omega-3 fatty acids, found in fish and flaxseeds, are known to reduce inflammation and support brain health. Magnesium, found in leafy greens and nuts, helps regulate cortisol levels and the body’s stress response.
Vitamin Bs, found in whole grains, nuts, seeds, beans and animal products (mostly B12), help maintain a healthy nervous system and energy metabolism, improving mood and cognitive performance.
5 tips for the holiday table and beyond
Food is a big part of the festive season, and treating yourself to delicious treats can be part of the fun. Here are some tips for enjoying festive foods, while avoiding stress eating:
1. slow down: be mindful about the speed of your eating. Slow down, chew food well and put down your utensils after each bite
2. watch the clock: even if you’re eating more food than you normally would, sticking to the same timing of eating can help maintain your body’s response to the food. If you normally have an eight-hour eating window (the time between your first meal and last meal of the day) then stick to this even if you’re eating more
3. continue other health behaviours: even if we are eating more food or different food during the festive season, try to keep up other healthy behaviours, such as sleep and exercise
4. stay hydrated: make sure to drink plenty of fluids, especially water. This helps our body function and can help with feelings of hunger. When our brain gets the message something has entered the stomach (what we drink) this can provide a temporary reduction in feelings of hunger
5. don’t restrict: if we have a big day of eating, it can be tempting to restrict eating in the days before or after. But it is never a good idea to overly constrain food intake. It can lead to more overeating and worsen stress.
Reaching for cookies late at night can be characteristic of stress eating. Stokkete/Shutterstock Plus 3 bonus tips to manage holiday stress
1. shift your thinking: try reframing festive stress. Instead of viewing it as “something bad”, see it as “providing the energy” to reach your goals, such as a family gathering or present shopping
2. be kind to yourself and others: practise an act of compassion for someone else or try talking to yourself as you would a friend. These actions can stimulate our brains and improve wellbeing
3. do something enjoyable: being absorbed in enjoyable activities – such as crafting, movement or even breathing exercises – can help our brains and bodies to return to a more relaxed state, feel steady and connected.
For support and more information about eating disorders, contact the Butterfly Foundation on 1800 33 4673 or Kids Helpline on 1800 551 800. If this article has raised issues for you, or if you’re concerned about someone you know, call Lifeline on 13 11 14. In an emergency, call 000.
Saman Khalesi, Senior Lecturer and Discipline Lead in Nutrition, School of Health, Medical and Applied Sciences, CQUniversity Australia; Charlotte Gupta, Senior Postdoctoral Research Fellow, Appleton Institute, HealthWise research group, CQUniversity Australia, and Talitha Best, Professor of Psychology, NeuroHealth Lab, Appleton Institute, CQUniversity Australia
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Miracle of Flexibility – by Miranda Esmonde-White
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve reviewed books about stretching before, so what makes this one different?
Mostly, it’s that this one takes a holistic approach, making the argument for looking after all parts of flexibility (even parts that might seem useless) because if one bit of us isn’t flexible, the others will start to suffer in compensation because of how that affects our posture, or movement, or in many cases our lack of movement.
Esmonde-White’s “flexibility, from your toes to your shoulders” approach is very consistent with her background as a professional ballet dancer, and now she brings it into her profession as a coach.
The book’s not just about stretching, though. It looks at problems and what can go wrong with posture and the body’s “musculoskeletal trifecta”, and also shares daily training routines that are tailored for specific sporting interests, and/or for those with specific chronic conditions and/or chronic pain. Working around what needs to be worked around, but also looking at strengthening what can be strengthened and fixing what can be fixed along the way.
Bottom line: if your flexibility needs an overhaul, this book is a very good “one-stop shop” for that.
Click here to check out The Miracle Of Flexibility, and discover what you can do!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
We’re only using a fraction of health workers’ skills. This needs to change
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Roles of health professionals are still unfortunately often stuck in the past. That is, before the shift of education of nurses and other health professionals into universities in the 1980s. So many are still not working to their full scope of practice.
There has been some expansion of roles in recent years – including pharmacists prescribing (under limited circumstances) and administering a wider range of vaccinations.
But the recently released paper from an independent Commonwealth review on health workers’ “scope of practice” identifies the myriad of barriers preventing Australians from fully benefiting from health professionals’ skills.
These include workforce design (who does what, where and how roles interact), legislation and regulation (which often differs according to jurisdiction), and how health workers are funded and paid.
There is no simple quick fix for this type of reform. But we now have a sensible pathway to improve access to care, using all health professionals appropriately.
A new vision for general practice
I recently had a COVID booster. To do this, I logged onto my general practice’s website, answered the question about what I wanted, booked an appointment with the practice nurse that afternoon, got jabbed, was bulk-billed, sat down for a while, and then went home. Nothing remarkable at all about that.
But that interaction required a host of facilitating factors. The Victorian government regulates whether nurses can provide vaccinations, and what additional training the nurse requires. The Commonwealth government has allowed the practice to be paid by Medicare for the nurse’s work. The venture capitalist practice owner has done the sums and decided allocating a room to a practice nurse is economically rational.
The future of primary care is one involving more use of the range of health professionals, in addition to GPs.
It would be good if my general practice also had a physiotherapist, who I could see if I had back pain without seeing the GP, but there is no Medicare rebate for this. This arrangement would need both health professionals to have access to my health record. There also needs to be trust and good communication between the two when the physio might think the GP needs to be alerted to any issues.
This vision is one of integrated primary care, with health professionals working in a team. The nurse should be able to do more than vaccination and checking vital signs. Do I really need to see the GP every time I need a prescription renewed for my regular medication? This is the nub of the “scope of practice” issue.
How about pharmacists?
An integrated future is not the only future on the table. Pharmacy owners especially have argued that pharmacists should be able to practise independently of GPs, prescribing a limited range of medications and dispensing them.
This will inevitably reduce continuity of care and potentially create risks if the GP is not aware of what other medications a patient is using.
But a greater role for pharmacists has benefits for patients. It is often easier and cheaper for the patient to see a pharmacist, especially as bulk billing rates fall, and this is one of the reasons why independent pharmacist prescribing is gaining traction.
It’s often easier for a patient to see a pharmacist than a GP. PeopleImages.com – Yuri A/Shutterstock Every five years or so the government negotiates an agreement with the Pharmacy Guild, the organisation of pharmacy owners, about how much pharmacies will be paid for dispensing medications and other services. These agreements are called “Community Pharmacy Agreements”. Paying pharmacists independent prescribing may be part of the next agreement, the details of which are currently being negotiated.
GPs don’t like competition from this new source, even though there will be plenty of work around for GPs into the foreseeable future. So their organisations highlight the risks of these changes, reopening centuries old turf wars dressed up as concerns about safety and risk.
Who pays for all this?
Funding is at the heart of disputes about scope of practice. As with many policy debates, there is merit on both sides.
Clearly the government must increase its support for comprehensive general practice. Existing funding of fee-for-service medical benefits payments must be redesigned and supplemented by payments that allow practices to engage a range of other health professionals to create health-care teams.
This should be the principal direction of primary care reform, and the final report of the scope of practice review should make that clear. It must focus on the overall goal of better primary care, rather than simply the aspirations of individual health professionals, and working to a professional’s full scope of practice in a team, not a professional silo.
In parallel, governments – state and federal – must ensure all health professionals are used to their best of their abilities. It is a waste to have highly educated professionals not using their skills fully. New funding arrangements should facilitate better access to care from all appropriately qualified health professionals.
In the case of prescribing, it is possible to reconcile the aspirations of pharmacists and the concerns of GPs. New arrangements could be that pharmacists can only renew medications if they have agreements with the GP and there is good communication between them. This may be easier in rural and suburban areas, where the pharmacists are better known to the GPs.
The second issues paper points to the complexity of achieving scope of practice reforms. However, it also sets out a sensible path to improve access to care using all health professionals appropriately.
Stephen Duckett, Honorary Enterprise Professor, School of Population and Global Health, and Department of General Practice and Primary Care, The University of Melbourne
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: